Search
- Page Path
- HOME > Search
Original Articles
- Hook plate fixation for volar plate avulsion fractures of the middle phalanges in Korea: a case series
- Kang-San Lee, Sang-Woo Son, Hee-June Kim, Hyun-Joo Lee, Dong Hee Kim
- J Musculoskelet Trauma 2026;39(1):48-53. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00339

-
 Abstract
Abstract
 PDF
PDF - Background
Volar plate avulsion fractures in phalanges are relatively common injuries. While surgical treatment can help reduce limitations in motion after injury, the small size of the fracture fragment can make the procedure challenging. In this study, we used hook plate fixation as a surgical technique for treating volar avulsion fractures in phalanges and evaluated its radiological and clinical outcomes.
Methods
The medical records of eight patients (nine digits) with volar plate avulsion fractures of the middle phalanx were retrospectively reviewed. All fractures were treated with a 1.5-mm hook plate after open reduction. Radiologic evaluations were performed using simple radiographs, and clinical outcomes were assessed through range of motion, instability, and pain.
Results
The mean follow-up period was 4.89 months (range, 1–9 months). All nine digits achieved bone union at the final follow-up. The mean union time was 2.2 months (range, 1–4 months). In all patients, the range of motion in the proximal interphalangeal joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. All patients demonstrated no joint instability and no residual pain.
Conclusion
Using a hook plate for volar plate avulsion fractures presents a promising alternative to existing fixation methods. Its biomechanical advantages and ease of fabrication make it a valuable tool in hand surgery. Level of evidence: IV.
- 191 View
- 8 Download

- Association between decreased bone mineral density and Pauwels angle in femoral neck fractures: a cross-sectional study
- Soo-Hwan Jung, Yong-Uk Kwon, Ji-Hun Park
- J Musculoskelet Trauma 2026;39(1):20-29. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00269

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
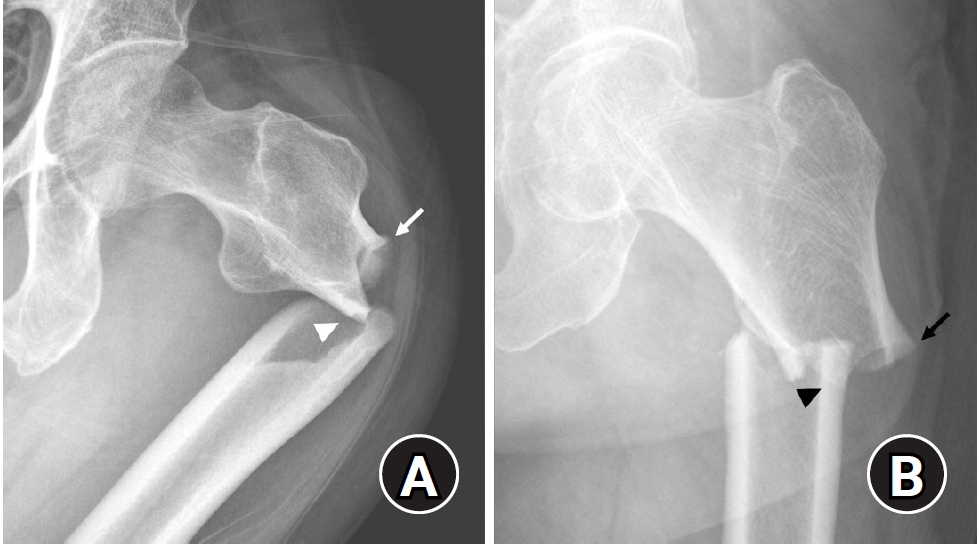
Progressive osteoporosis reduces the trabecular structures of the proximal femur, whereas the primary compression trabeculae (PCTs) are relatively preserved. We hypothesize that the loss of the vertically oriented PCTs in osteoporosis, which act as a mechanical barrier, affects fracture line propagation and influences the Pauwels angle. This study investigated the association between bone mineral density (BMD) and Pauwels angles in low-energy femoral neck fractures (FNFs).
Methods
This cross-sectional study included 150 patients (mean age, 75.3 years; range, 50–94 years) diagnosed with intracapsular FNFs between May 2019 and May 2023. BMD was measured within 1 month of the injury date using dual-energy X-ray absorptiometry, and modified Pauwels angles were assessed using a computed tomography-based multiplanar reconstruction program. Multiple linear regression analysis was performed to evaluate the factors influencing the Pauwels angles. The dependent variable was the Pauwels angle, while the independent variables included sex, age, height, body weight, body mass index, American Society of Anesthesiologists score, Charlson comorbidity index score, smoking status, alcohol use, preinjury walking ability, and femoral neck BMD T-scores.
Results
Higher femoral neck BMD T-scores were significantly associated with increased Pauwels angles (β=3.449, P<0.001). Greater body weight was independently associated with increased Pauwels angles (β=0.213, P=0.007).
Conclusions
The Pauwels angle demonstrated a significant association with BMD, with lower BMD associated with less steep Pauwels angles. In the absence of BMD measurement, the Pauwels angle may indicate osteoporosis severity in patients with low-energy FNFs. Level of evidence: III.
- 137 View
- 4 Download

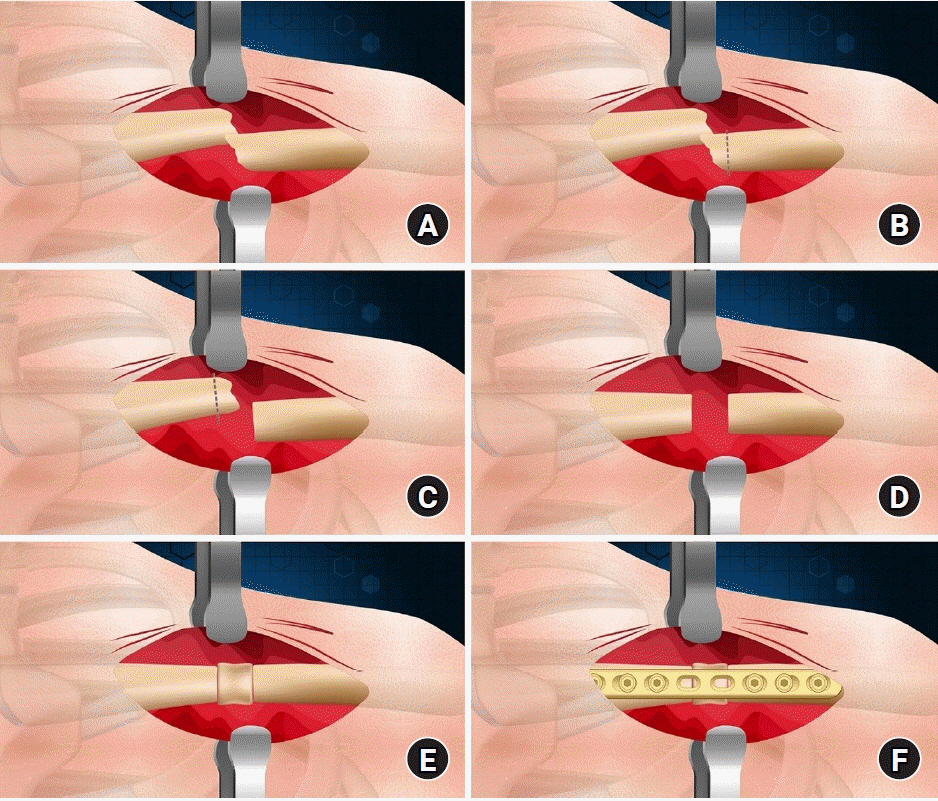
Technical Note
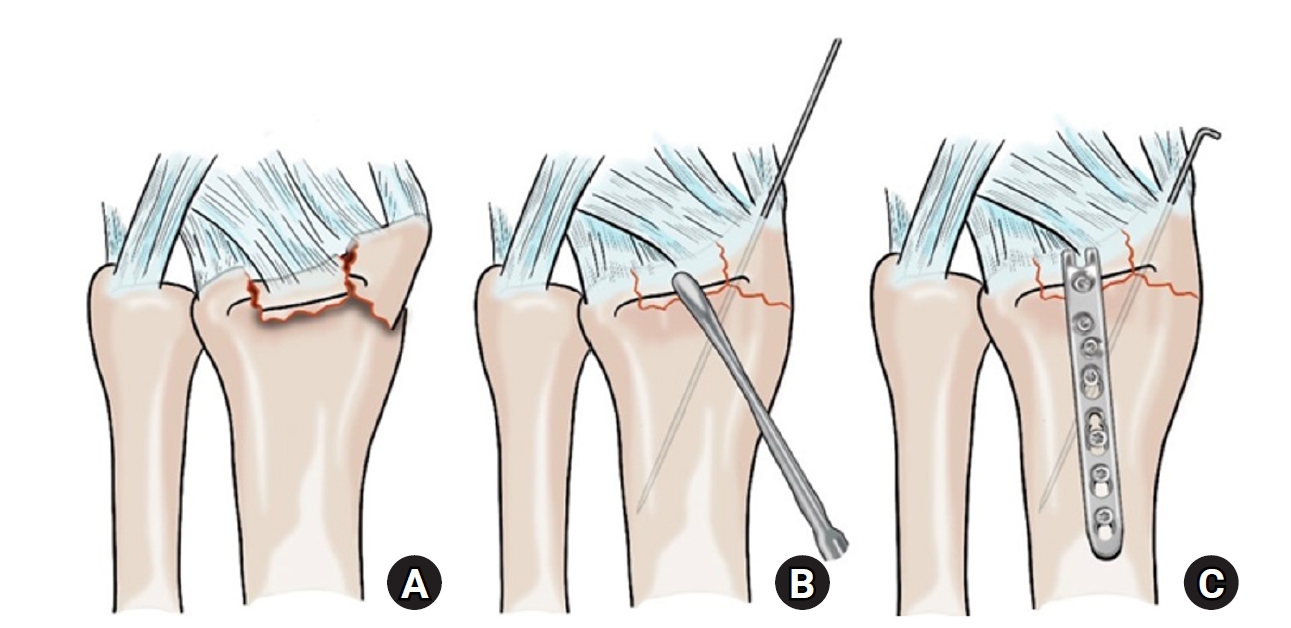
- Rim plate-assisted intramedullary nail and plate combination technique for complex tibial plateau-to-diaphysis fractures: a technical note and case series
- Whee Sung Son
- J Musculoskelet Trauma 2026;39(1):62-71. Published online December 4, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00290

-
 Abstract
Abstract
 PDF
PDF - Complex tibial plateau-to-diaphysis fractures present a significant surgical challenge due to their intricate fracture patterns and frequent association with severe soft tissue damage and concomitant injuries. This technical note introduces a novel fixation strategy: the rim plate-assisted intramedullary nail-plate combination (NPC) technique. In this approach, a rim plate simplifies the conventional NPC procedure by unifying the tibial plateau fracture into a single structural segment. This modification eliminates the need to address the articular and diaphyseal components simultaneously while enhancing articular stability. Furthermore, the technique preserves soft tissue integrity and promotes early rehabilitation. Clinical case examples demonstrate its successful application in managing complex tibial plateau-to-diaphysis injuries. Level of evidence: V.
- 521 View
- 22 Download

Review Article
- Current concepts and applications of bone graft substitutes in orthopedic surgery
- Jae Ho Cho, Hyung Keun Song
- J Musculoskelet Trauma 2025;38(4):169-177. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00248
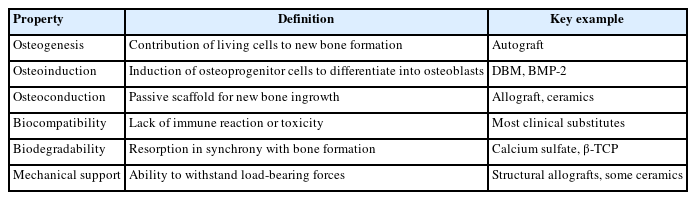
-
 Abstract
Abstract
 PDF
PDF - Bone defects, which often arise from high-energy injuries, infections, tumor resections, or nonunions, represent a persistent challenge in orthopedic trauma surgery. Autologous bone grafting remains the gold standard due to its unique combination of osteogenic, osteoinductive, and osteoconductive properties. However, issues such as donor site morbidity, limited graft volume, and increased surgical time have driven the development of bone graft substitutes. These substitutes vary widely in origin, composition, biological activity, and mechanical characteristics, encompassing allografts, xenografts, synthetic materials, and biologically enhanced constructs. This review outlines the fundamental biological principles underlying bone regeneration—including osteogenesis, osteoinduction, and osteoconduction—and addresses additional key factors such as biocompatibility, biodegradability, and mechanical strength. Current bone graft materials are classified by biological origin and functional characteristics, with an emphasis on their use in trauma surgery. Particular attention is given to the clinical applications, indications, and limitations of allograft-based solutions (such as structural allografts and demineralized bone matrix), synthetic ceramics (including calcium phosphate and bioactive glass), and biologically enhanced options, such as recombinant growth factors and stem cell therapies. In trauma settings, graft selection must be tailored to the characteristics of the defect, mechanical demands, the biological environment, and patient-specific factors. Integration with surgical technique and fixation is crucial for optimizing outcomes. Although modern substitutes show promise, none fully replicate the complex biology of autografts. Looking ahead, emerging technologies such as 3D printing, nanotechnology, and smart biomaterials offer exciting possibilities but face translational challenges. This review aims to provide practicing orthopedic surgeons with a concise, evidence-based overview of bone substitute options and their roles in trauma care. By applying core biological principles and clinical judgment, surgeons can better navigate the expanding array of graft materials to improve outcomes for patients with complex skeletal defects.
-
Citations
Citations to this article as recorded by- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
Seungyeob Sakong, Seokjun Hong, Wonseok Choi, Seonghyun Kang, Jae-Woo Cho, Whee Sung Son, Jeong-Seok Choi, Chang-Jin Yon, Won-Tae Cho, Jong-Keon Oh
Journal of Clinical Medicine.2026; 15(3): 1176. CrossRef
- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
- 4,317 View
- 100 Download
- 1 Crossref

Original Articles
- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- Hyun-Jae Park, Joo-Hak Kim
- J Musculoskelet Trauma 2025;38(4):221-228. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00241
-
 Abstract
Abstract
 PDF
PDF - Background
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures. Level of evidence: IV.
- 382 View
- 11 Download

- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
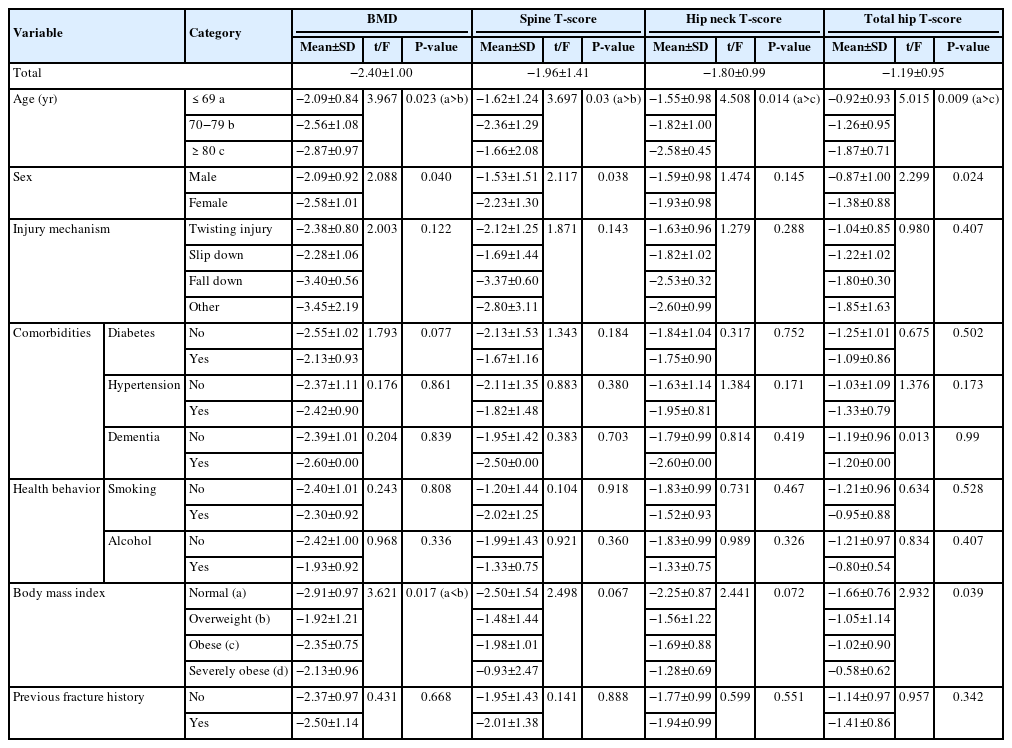
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 898 View
- 2,147,483,670 Download

Review Articles
- Atypical ulnar fractures: a narrative review of current concepts and a case of bilateral surgical management
- Chi-Hoon Oh, Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):124-132. Published online July 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00227
-
 Abstract
Abstract
 PDF
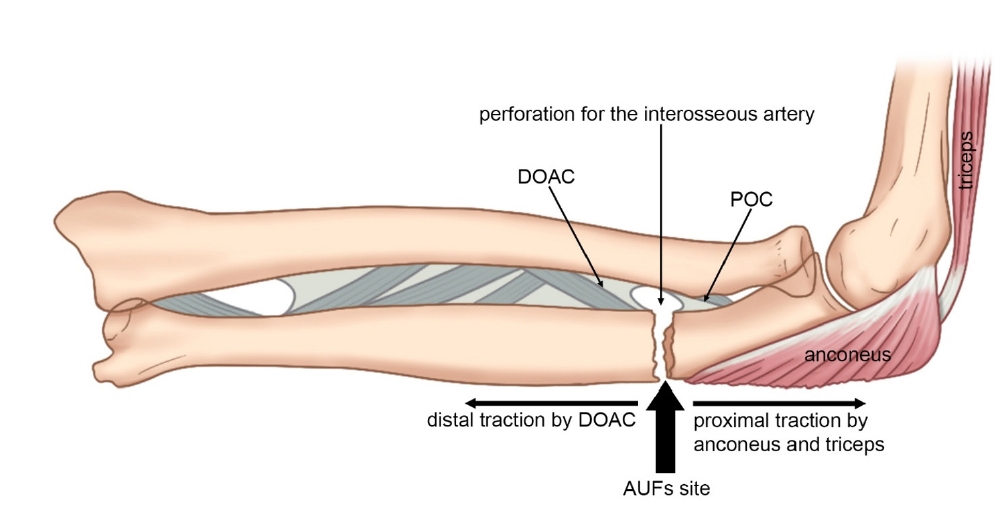
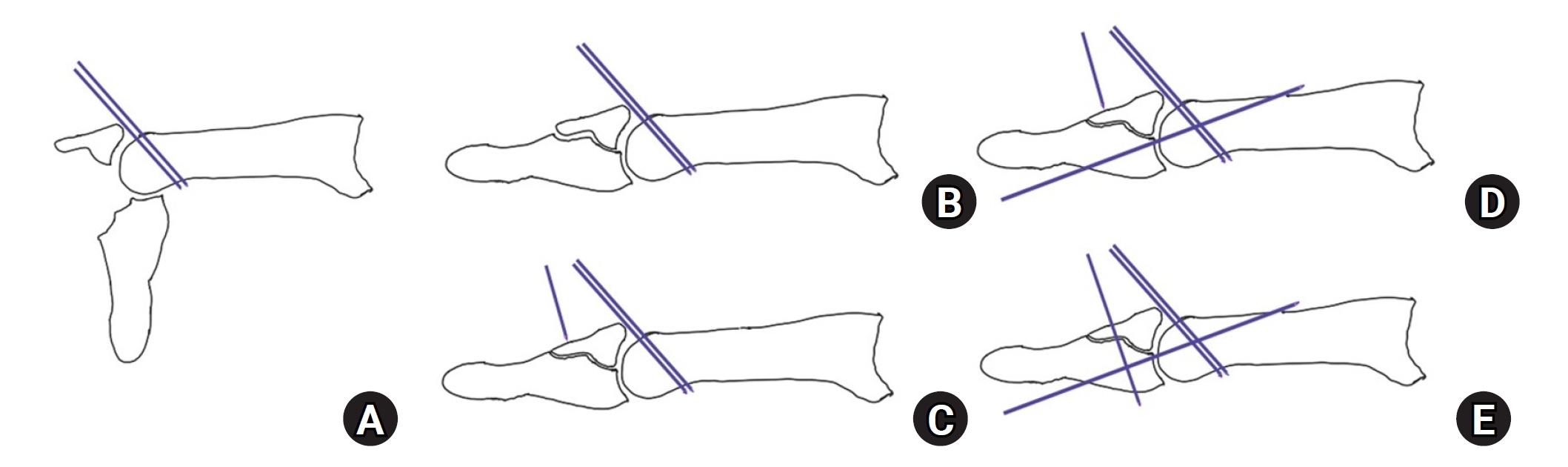
PDF - Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
- 1,522 View
- 47 Download

- Current concepts in the management of phalangeal fractures in the hand
- Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):109-123. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00136
-
 Abstract
Abstract
 PDF
PDF - This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra- articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
- 17,323 View
- 379 Download

Original Article
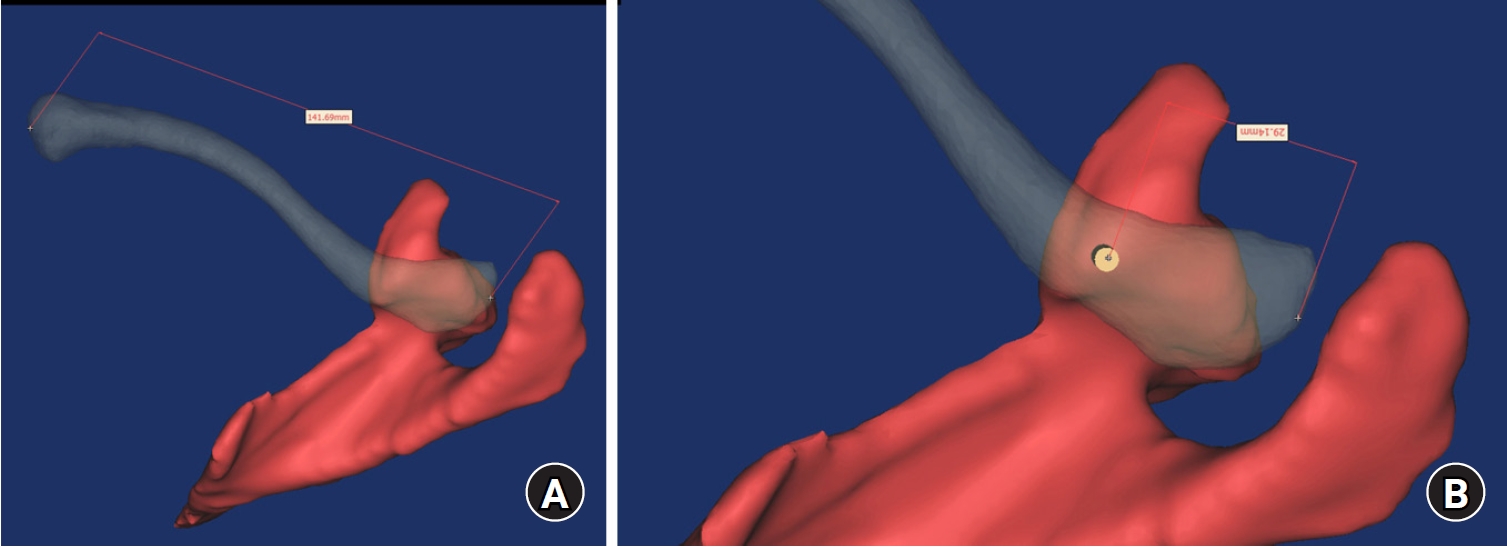
- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
-
 Abstract
Abstract
 PDF
PDF - Background
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 671 View
- 22 Download

Review Articles
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00024

-
 Abstract
Abstract
 PDF
PDF - Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Citations
Citations to this article as recorded by- Rigid intramedullary nailing with suprapatellar approach for tibial shaft fractures in adolescents with open physes
Jong Wha Lee, Jae Ho Cho, Tae Hun Kim, Hyung Keun Song, Won-Tae Cho, Seungyeob Sakong, Hyunil Choi, Sumin Lim
Injury.2026; : 113130. CrossRef - Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
Jungtae Ahn, Dae-Cheol Nam, Gu-Hee Jung
Clinics in Orthopedic Surgery.2025; 17(6): 1062. CrossRef
- Rigid intramedullary nailing with suprapatellar approach for tibial shaft fractures in adolescents with open physes
- 2,954 View
- 56 Download
- 2 Crossref

- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
-
Citations
Citations to this article as recorded by- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
Lorenzo Lucchetta, Carmelinda Ruggiero, Samuele Berardi, Alice Franceschi, Michele Bisaccia, Giuseppe Rinonapoli
Journal of Clinical Medicine.2025; 15(1): 25. CrossRef
- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
- 15,028 View
- 411 Download
- 1 Crossref

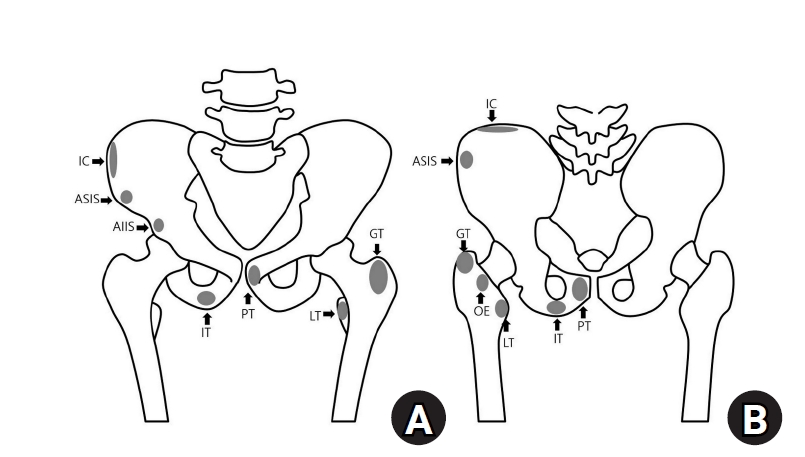
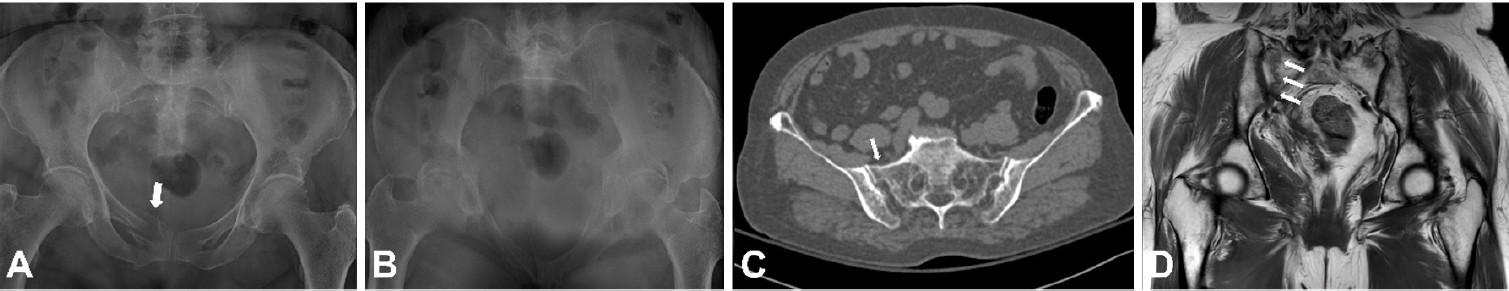
- Avulsion fractures around the hip joint and pelvis
- Won-Sik Choy, Yonghan Cha, Jung-Taek Kim, Jun-Il Yoo, Jin-Woo Kim
- J Musculoskelet Trauma 2025;38(2):53-62. Published online March 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00010
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures occur when tendons or ligaments are subjected to forces greater than they can withstand at the apophysis or enthesis, regardless of fusion status. The pelvis and hip joint are vulnerable to these injuries due to the diverse muscular structures in these structures, which serve as origins for multiple muscles leading to the lower extremities. Pelvic avulsion fractures commonly affect young athletes, but can also occur in adults. The diagnosis typically involves assessing trauma history, a clinical examination, and radiographic imaging. If the diagnosis is unclear, additional tests such as computed tomography and magnetic resonance imaging may assist in the diagnosis and provide useful information for treatment decisions. While most avulsion fractures respond well to conservative treatment, surgical intervention may be preferred in severe displacements, cases of significant retraction in active athletes, or when a faster recovery is necessary. Chronic or neglected injuries may lead to excessive osseous formation around the pelvis, causing impingement syndromes. Recognizing characteristic radiological findings based on pelvic anatomy helps to make an accurate diagnosis, as chronic injuries can mimic tumors or infectious conditions, necessitating a careful differential diagnosis.
-
Citations
Citations to this article as recorded by- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
Dawid Bartosik, Bartlomiej Cwikla, Anna Kowalczyk, Michalina Loson-Kawalec, Anna Palka-Szymaniec, Bartosz Starzynski, Alina Keska, Jakub Szkuta, Klaudia Wojcik
Cureus.2026;[Epub] CrossRef
- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
- 9,162 View
- 137 Download
- 1 Crossref

Original Article
- Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(2):96-101. Published online February 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059
- Correction in: J Musculoskelet Trauma 2025;38(3):168

-
 Abstract
Abstract
 PDF
PDF - Background
Mayo type IIIB olecranon fractures are characterized by significant displacement and comminution, presenting a challenge in selecting the appropriate fixation technique. This study compared the clinical and radiographic outcomes, complications, and reoperation rates of reinforced tension band wiring (TBW) and precontoured plate and screw fixation (PF) in the surgical treatment of Mayo type IIIB olecranon fractures.
Methods
This retrospective review analyzed 24 patients diagnosed with Mayo type IIIB olecranon fractures, who were treated between 2005 and 2023. Of these, 11 patients underwent reinforced TBW, and 13 received precontoured PF. Clinical outcomes were assessed using Disabilities of the Arm, Shoulder, and Hand (DASH) scores and the Mayo Elbow Performance Score (MEPS). Radiographic outcomes focused on fracture union. Operative times, complication rates, and reoperation rates were compared between the groups.
Results
Both the reinforced TBW and PF groups achieved satisfactory clinical outcomes, with no significant between-group differences in DASH and MEPS scores (P>0.05). Radiographic union was achieved in all patients. The reinforced TBW group demonstrated a significantly shorter operative time than the PF group (93.6±7.4 min vs. 132.3±13.7 min; P<0.001). Complication rates were similar between the two groups (reinforced TBW, 38.4%; PF, 36.3%), but hardware-related irritation occurred more frequently in the reinforced TBW group. Reoperations were required in 15.8% of the reinforced TBW group due to hardware irritation, whereas no reoperations were necessary in the PF group.
Conclusions
Reinforced TBW and PF are both effective surgical options for managing Mayo type IIIB olecranon fractures, yielding comparable clinical and radiographic outcomes. While reinforced TBW offers shorter operative times and lower costs, PF is associated with fewer hardware-related complications. Further prospective studies are needed to optimize treatment strategies for these complex fractures. Level of Evidence: Level III. -
Citations
Citations to this article as recorded by- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
Reva Qiu, Mallika Makkar, Richard Buckley
Injury.2025; 56(11): 112769. CrossRef
- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
- 2,292 View
- 51 Download
- 1 Crossref

Review Article
- Easily missed nondisplaced fractures accompanying complete fractures in the lower extremity and pelvis: a narrative review
- Young-Chang Park
- J Musculoskelet Trauma 2025;38(1):5-12. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00017
-
 Abstract
Abstract
 PDF
PDF - Nondisplaced fractures accompanying complete fractures are often difficult to detect on plain radiographs or computed tomography scans, posing a diagnostic challenge. The diagnosis of these frequently overlooked injuries can be delayed, potentially leading to suboptimal patient outcomes. This review discusses four commonly missed fracture patterns in the lower extremity and pelvis, including posterior involvement in fragility fractures of the pelvis, intertrochanteric extensions in isolated greater trochanter fractures, ipsilateral femoral neck fractures in high energy femoral shaft fractures, and posterior malleolar fractures in distal spiral tibial shaft fractures. An accurate diagnosis of these accompanying nondisplaced fractures is critical for optimizing surgical outcomes. Surgeons should incorporate thorough preoperative evaluations into their clinical practice to facilitate early detection and appropriate treatment strategies. Prompt identification and comprehensive management remain essential for improving patient outcomes.
- 1,376 View
- 47 Download

Original Articles
- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005

-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 2,047 View
- 59 Download

- Interpositional tricortical iliac bone graft in nonunion of midshaft clavicular fractures
- Eun-Seok Son, Bum-Soon Park, Chang-Jin Yon, Chul-Hyun Cho
- J Musculoskelet Trauma 2025;38(1):23-31. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00004
-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to investigate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures. Methods: Between 2007 and 2020, 17 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion combined with bone defect were investigated. The mean age was 53 years (range, 22–70 years). The mean follow-up period was 102.2 months (range, 18–193 months). Serial plain radiographs were used to evaluate radiological outcomes. The University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate clinical outcomes. Complications were also evaluated. Results: All cases achieved complete bony union with mean healing time of 17.6 weeks (range, 14–22 weeks). The mean clavicle length difference was significantly decreased from 9.1 mm preoperatively to 2.6 mm postoperatively (P<0.001). The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001), respectively. The mean final Quick-DASH score was 18.0. Three cases (17.6%) developed postoperative complications including two cases of shoulder stiffness and one case of screw irritation. Conclusions: Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length. Level of evidence: Level IV, case series.
- 2,026 View
- 44 Download

Review Article
- Avulsion Fractures in the Ankle and Foot
- Gyeong Hoon Lim, Jae Won Kim, Sung Hyun Lee
- J Korean Fract Soc 2024;37(2):102-116. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.102
-
 Abstract
Abstract
 PDF
PDF - An avulsion fracture occurs when a muscle-tendon unit attached to a bone produces sufficient force to tear a fragment of the bone. If not treated properly, this injury can lead to deformity, nonunion, malunion, pain, and disability. Although avulsion fractures around the foot and ankle can occur anywhere there are tendon and ligament attachments, they are common in the anterior talofibular ligament, anterior-inferior tibiotalar ligament, calcaneal tuberosity, the base of the fifth metatarsal, and navicular bone. The optimal treatment for each fracture depends on the location and severity of the fracture. Conservative treatment involves limiting weight bearing for a period, splint immobilization, and using various orthoses. Surgical treatment is usually reserved for cases of severe displacement or when nonsurgical treatment has failed. The goals of surgery include reduction of the fracture fragment, prevention of nonunion or malunion and soft tissue injury, and early return to function. The decision for each treatment modality may depend on the patient demographics or preferences and the surgeon experience. This review summarizes previous and current views on the pathogenesis, diagnosis, and treatment of common avulsion fractures to guide the treatment and diagnosis.
- 2,097 View
- 48 Download

Original Article
- Effect of Additional Medial Locking Plate Fixation and Autogenous Bone Graft for Distal Femur Nonunion after Lateral Locking Plate Fixation
- Ho Min Lee, Jong Pil Kim, In Hwa Baek, Han Sol Moon, Sun Kyo Nam
- J Korean Fract Soc 2024;37(1):30-38. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the outcomes of additional medial locking plate fixation and autogenous bone grafting in the treatment of nonunions that occurred after initial fixation for distal femoral fractures using lateral locking plates.
Materials and Methods
The study involved eleven patients who initially underwent minimally invasive lateral locking plate fixation for distal femoral fractures between January 2008 and December 2020. The initial procedure was followed by additional medial locking plate fixation and autogenous bone grafting for clinically and radiographically confirmed nonunions, while leaving the stable lateral locking plate in situ. A clinical evaluation of the bone union time, knee joint range of motion, visual analog scale (VAS) pain scores, presence of postoperative complications, and functional evaluations using the lower extremity functional scale (LEFS) were performed.
Results
In all cases, bone union was achieved in an average of 6.1 months after the secondary surgery. The range of knee joint motion, weight-bearing ability, and VAS and LEFS scores improved at the final follow-up compared to the preoperative conditions. All patients could walk without walking assistive devices and did not experience pain at the fracture site. On the other hand, three patients complained of pain in the lateral knee joint caused by irritation by the lateral locking plate; hence, lateral hardware removal was performed. One patient complained of mild paresthesia at the anteromedial incision site. Severe complications, such as deep infection or metal failure, were not observed.
Conclusion
For nonunion with stable lateral locking plates after minimally invasive lateral locking plate fixation of distal femur fractures, additional medial locking plate fixation and autogenous bone grafting, while leaving the lateral locking plate intact, can achieve successful bone union.
- 394 View
- 5 Download

Review Articles
- Fracture-Related Complication: Fat Embolism Syndrome
- Beom-Soo Kim
- J Korean Fract Soc 2023;36(3):95-102. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.95
-
 Abstract
Abstract
 PDF
PDF - Fat embolization is a common occurrence after trauma or during orthopedic procedures involving intramedullary manipulation. Although uncommon, fat embolism syndrome (FES) with respiratory failure, neurologic dysfunction, and petechial rash can be fatal to patients. Two theories are proposed for the manifestation of FES: in the mechanical theory, FES occurs when fat tissue in the bone marrow enters the bloodstream and mechanically blocks it; the biochemical theory proposes that FES occurs due to an inflammatory reaction caused by free fatty acids. There are currently no clear diagnostic criteria for FES, and symptoms and signs are typically nonspecific. For the treatment of FES, conservative and supportive management is performed for the specific symptoms, and close monitoring of the respiratory and neurologic systems is required in high-risk groups. Early fracture fixation of long bones helps prevent and reduce the severity of fat embolism.
- 945 View
- 11 Download

- Treatment of Scaphoid Fractures and Nonunions
- Wan-Sun Choi
- J Korean Fract Soc 2022;35(4):182-189. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.182
-
 Abstract
Abstract
 PDF
PDF - A scaphoid fracture is one of the most common types of wrist fractures, and if treatment is delayed, there is a high possibility of nonunion due to anatomical factors such as limited blood supply to the injured bone. Therefore, it is important to suspect a scaphoid fracture based on the mechanism of wrist injury and physical examination of the patient. A computed tomography scan or magnetic resonance imaging can also aid early diagnosis of the fracture. Stable acute fractures can be treated conservatively, but unstable fractures require surgical treatment, and percutaneous screw fixation is usually performed. Nonunions require bone grafts and are treated with non-vascularized bone grafts and screw fixation. However, if the nonunion is located at the proximal pole, a vascularized bone graft may be considered because there is a possibility of avascular necrosis. Pedicled vascularized and free vascularized medial femoral condyle bone grafts are mainly used in such cases. The treatment of a proximal pole nonunion with impaired blood flow remains controversial. There are conflicting opinions on whether a nonvascularized bone graft is sufficient or whether a vascularized bone graft is necessary.
- 695 View
- 6 Download

Original Article
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
- J Korean Fract Soc 2022;35(4):151-161. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.151
-
 Abstract
Abstract
 PDF
PDF - Purpose
Osteoporosis causes various fixation failures in patients with intertrochanteric fractures. This study aimed to investigate the effect of a demineralized bone matrix (DBM) for cancellous or cortical bone defects on internal fixation in older osteoporotic patients with intertrochanteric fractures.
Materials and Methods
Among patients with intertrochanteric fractures who underwent surgical treatment from January 2016 to December 2021 at a facility, 171 patients were AO/OTA type 31-A1 and type 2 fractures which are considered relatively stable. The patients were grouped based on DBM use (Group A: DBM use, Group B: DBM non-use), and their clinical and radiology results were analyzed retrospectively. The patients were then subdivided into Group A-a and -b after removing factors that could cause treatment failures, such as the reduction status and location of the helical blade, and then further subdivided (Group A-a-1/2/3/4 and Group B-b-1/2/3/4) according to cancellous or cortical bone defects that could accompany intertrochanteric fractures. The time to full weight-bearing (FWB) and Harris hip score (HSS) 3 months after surgery in these subgroups were investigated.
Results
There was no significant difference in the clinical radiology results and complications between Group A and Group B. However, the time to FWB (p<0.001) and HSS (p=0.029) were significantly superior in Group A. In Group A-a with DBM use, after removing the risk factors for intertrochanteric fracture failure, the time to FWB (p=0.055) was close to the significance level, and HSS (p=0.036) was significantly superior. In Group A-a-1 (cancellous defect only) and Group A-a-3 (cancellous and cortical defect), the time to FWB (p=0.088, 0.052) was close to the significance level, and the HSS (p=0.039, 0.018) was significantly superior when DBM was used.
Conclusion
In patients with intertrochanteric fractures of AO/OTA type 31-A2.3 or less, if stable reduction and firm fixation are achieved, selective DBM use may help early recovery after surgery.
- 469 View
- 2 Download

Review Articles
- Perilunate Dislocation and Perilunate Fracture-Dislocation
- Jung Il Lee
- J Korean Fract Soc 2022;35(3):114-119. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.114
-
 Abstract
Abstract
 PDF
PDF - Perilunate dislocations and perilunate fracture-dislocations are one of the most severe forms of wrist injuries and are generally caused by high-energy trauma such as falls from a height or traffic accidents. Prompt recognition and immediate, gentle closed reduction are critical, but diagnosis can often be missed at the initial presentation. The current standard management is open reduction, ligamentous and bony repair, and supplemental fixation for the protection of the repair. The pathomechanics of the injury, diagnosis by plain wrist radiographs, closed reduction techniques, current surgical treatments, and complications are presented in this review.
- 651 View
- 8 Download

- Lisfranc Joint Injury
- Bi O Jeong, Jungtae Ahn
- J Korean Fract Soc 2022;35(2):83-89. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.83
-
 Abstract
Abstract
 PDF
PDF - The Lisfranc joint complex is composed of complex bony structures, ligaments, and soft tissues and has a systematic interrelationship. Sufficient radiologic modalities should be considered for an accurate initial diagnosis. Based on an accurate understanding of normal anatomy and restoration of anatomical relationships, the diagnosis should be obtained, and more discussion is needed on detailed treatment strategies.
- 1,489 View
- 14 Download

Original Articles
- Minimal Invasive Fixation Methods for the Metacarpal Fracture
- Ki Youn Kwon, Jin Rok Oh, Ji Woong Kwak
- J Korean Fract Soc 2022;35(1):9-15. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.9
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the radiologic and clinical outcomes of metacarpal fractures treated with two minimally invasive surgical techniques: Kirschner wire (K-wire) fixation and headless screw fixation.
Materials and Methods
This study included 52 patients (46 males and 6 females; age 18-55 years) with distal metacarpal fractures (middle and distal shaft, including the neck) who had undergone K-wire fixation or headless screw fixation. All subjects were followed up for at least six months. The radiologic assessments were performed to evaluate the angular deformity and shortenings. The total active motion (TAM), grip strength, and patients’ subjective functional assessment were measured to evaluate the hand function. The time taken to return to work (RTW) and adverse events were analyzed.
Results
Of the 52 cases, metacarpal fractures treated with headless screw fixation and K-wire fixation showed a significant difference associated with early RTW (p<0.05). There were no significant differences between the subjects treated with K-wire fixation and those with headless screw fixation in terms of the radiologic measurement, hand function examinations, complications, and adverse events (p>0.05).
Conclusion
After a six-month follow-up, minimally invasive K-wire fixation and headless screw fixation produced similar clinical and radiologic outcomes in subjects with metacarpal fractures. Compared to K-wire fixation, however, headless screw fixation led to earlier functional recovery and might be a better option for treating metacarpal fractures in this regard.
- 560 View
- 5 Download

- Comparing Outcomes of Retrograde Intramedullary Nail and Locking Plate Fixation in Distal Femoral Fractures
- Byung-Ho Yoon, Bo Kwon Hwang, Hyoung-Keun Oh, Suk Kyu Choo, Jong Min Sohn, Yerl-Bo Sung
- J Korean Fract Soc 2021;34(4):131-136. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.131
-
 Abstract
Abstract
 PDF
PDF - Purpose
We compared the radiological and clinical results of fixation for distal femoral fracture (DFF) using a locking compression plate (LCP) or a retrograde intramedullary nail (RIN).
Materials and Methods
From October 2003 to February 2020, 52 cases of DFF with a minimum 1-year follow-up (with a mean follow-up of 19.1 months) were included: 31 were treated with LCP and 21 with RIN. The operation time, blood loss, and hospitalization period were compared, and the incidence of postoperative nonunion, malunion, delayed union and metal failure and other post-operative complications were evaluated and compared.
Results
There was no significant difference in the operating time between the two groups, but the mean blood loss was significantly higher in the LCP group (LCP 683.5 ml vs RIN; 134.9 ml; p=0.015). In 49 out of 52 cases, bone union was achieved without additional surgery in an average of 6.8 months, and a complete union was achieved after additional surgery in three cases of nonunion (LCP 2 cases vs RIN 1 case; p=0.065). One case of malunion and superficial infection was confirmed in each group.
Conclusion
Internal fixation using LCP and RIN give good outcomes with a low complication rate and can therefore be considered useful surgical treatments for DFF.
- 480 View
- 6 Download

Review Articles
- Bone Substitutes: From Basic to Current Update
- Jong Seong Han, Hyung Keun Song
- J Korean Fract Soc 2020;33(4):238-244. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.238
-
 Abstract
Abstract
 PDF
PDF - Bone substitutes are being used increasingly in bony surgery as more than two million bone grafts are performed worldwide per year. Autobone grafts represent the gold standard for bone grafting, but morbidity and limited availability are the main problems. Allobone grafts are osteoconductive, but there are still concerns regarding the infection risks, costs, and donor availability issues. As an alternative, widely used ceramic-based synthetic bone substitutes are based alternatively on calcium (hydroxyapatite, tricalcium phosphate, calcium sulfate, calcium phosphate). Ceramic-based bone substitutes are osteoconductive, but they are weaker than cortical bone and are not osteoinductive. Bone morphogenic protein, demineralized bone matrix, and platelet-rich plasma are used to obtain an osteoinductive function. Recently, cell-based and gen-based bone substitutes were developed and studied. This paper reviews the basic information and the latest concepts on bone grafts and bone substitutes.
-
Citations
Citations to this article as recorded by- Tannic acid-modified magnesium oxychloride bone cement with high water resistance and osteogenic properties
Junying Chen, Yijia Guan, Yue Yang, Tingting Ma, Jinlun Feng, Wenjie Guo, Qifang Wang, Yanru Zhang, Jianguo Liao
Ceramics International.2024; 50(24): 53407. CrossRef - Surface modification of magnesium with a novel composite coating for application in bone tissue engineering
Jorgimara de O. Braga, Diogo M.M. dos Santos, Fernando Cotting, Vanessa F.C. Lins, Nádia M. Leão, Daniel C.F. Soares, Eric M. Mazzer, Manuel Houmard, Roberto B. Figueiredo, Eduardo H.M. Nunes
Surface and Coatings Technology.2022; 433: 128078. CrossRef
- Tannic acid-modified magnesium oxychloride bone cement with high water resistance and osteogenic properties
- 1,144 View
- 12 Download
- 2 Crossref

- Current Concepts of Bone Healing
- Dong Hun Suh, Bong Mo Koo, Jong Woo Kang
- J Korean Fract Soc 2020;33(3):171-177. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.171
-
 Abstract
Abstract
 PDF
PDF - Bone injuries induce an inflammatory response that promotes bone healing. On the other hand, an aberrant process, where inflammation becomes chronic, can inhibit the healing of injured bone. At the first stage of the bone healing process, inflammatory cells, such as neutrophils and macrophages, are assembled and secrete various cytokines, chemokines, and growth factors. During callus formation, cells differentiated from mesenchymal stem cells, such as osteoblasts and chondrocytes, play leading roles in bone healing. Currently, various treatment modalities have been developed through the known mechanism of bone healing, and the clinical outcomes of bone defect and fracture nonunion have been good.
- 2,308 View
- 91 Download

Case Report
- Treatment of Atypical Ulnar Fracture Associated with Bisphosphonate Therapy - A Case Report -
- Dong-Soo Kim, Ji-Kang Park, Eui-Sung Choi, Ho-Seung Jeong, Seok-Hyun Hong, Byung-Hyun Ahn
- J Korean Fract Soc 2020;33(2):101-104. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.101
-
 Abstract
Abstract
 PDF
PDF - Bisphosphonates can cause atypical fractures when taken for a long time. Atypical fractures appear mainly as femoral subtrochanteric or shaft fractures. On the other hand, reports of atypical fractures in the proximal ulna are relatively rare, with a high proportion of nonunion cases. This paper reports a case of nonunion after fixation for atypical fractures of the proximal ulna.
- 487 View
- 2 Download

Original Articles
- Failure of Intramedullary Nailing for Subtrochanteric Atypical Femoral Fractures Caused by Endosteal Cortical Thickening
- Young Ho Roh, Kimoon Kang, Hee Joong Kim, Kwang Woo Nam
- J Korean Fract Soc 2019;32(4):211-221. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.211
- Correction in: J Musculoskelet Trauma 2020;33(1):63
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Recent literature has noted incidences of subtrochanteric atypical femoral fractures (AFFs) in patients who have taken long-term bisphosphonates (BPs). Most cases of subtrochanteric AFFs have been treated with intramedullary nailing and cases of delayed union have been reported. On the other hand, there is no data available on the complications associated with endosteal thickening or cortical thickening. This study evaluated the results of surgical treatment according to the endosteal thickening of the lateral cortex in subtrochanteric AFFs.
MATERIALS AND METHODS
Investigation was performed at the Department of Orthopaedic Surgery, Jeju National University Hospital. The study consisted of patients with subtrochanteric AFFs, defined by the American Society for Bone and Mineral Research (ASBMR) major criteria, who underwent intramedullary nailing from March 2012 to October 2014. The cases were categorized into two groups based on the presence of endosteal thickening. The evaluation included the demographic data, radiographic data of initial reduction state, and duration of BPs.
RESULTS
The demographic data and duration of BPs were similar in the two groups. On the other hand, varus reduction (Group I: 12.5% vs. Group II: 78.9%; p=0.001), delayed union (Group I: 0% vs. Group II: 70.0%; p=0.003), nonunion (Group I: 0% vs. Group II: 47.4%; p=0.017), and union time (Group I: 5.5 months vs. Group II: 8.3 months; p<0.001) were significantly different in the two groups.
CONCLUSION
Endosteal thickening of the lateral cortex in subtrochanteric AFFs was identified as an independent factor that decides the reduction of the fracture and nonunion. The endosteal thickening should be removed to obtain anatomical alignment for successful surgical results. -
Citations
Citations to this article as recorded by- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
Hong Moon Sohn, Suenghwan Jo
Medical Biological Science and Engineering.2022; 5(2): 63. CrossRef
- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
- 1,156 View
- 5 Download
- 1 Crossref

- Simulation for Reduction of Transverse Acetabular Fractures in Sawbones Models
- Seongeun Byun, Cyril Mauffrey, Jehyun Yoo, Changwon Park, Jihyo Hwang
- J Korean Fract Soc 2019;32(4):196-203. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.196
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The transversely oriented fracture lines are very difficult to reduce during operations, even after clear exposure of the fracture site, in acetabular fractures. The purpose of this study is to verify the quality of reduction between the different subtypes (transtectal, juxtatectal, and infratectal) of transverse fractures. This study also determined the proper type of clamps to use and the proper zone for achieving accurate reductions in Sawbones models.
MATERIALS AND METHODS
Six fractures in 3 different subtypes of transverse fractures were artificially created. Ten different reduction clamps were applied for reduction of the fractures. Twelve holes around the fracture were drilled for the maintenance of the clamps. The fracture displacements were measured at the extra-articular area and the intra-articular joint portion. The pictures of the intra-articular fracture displacements were taken by a camera and these were uploaded and analyzed by the TraumaCad® computer program (Brainlab).
RESULTS
The reduction quality was poor in order of transtectal, juxtatectal and infratectal. The intraarticular opening was more prominent in the transtectal subtype. The safe zone, when giving consideration of the neurovascular bundles, was a quadrilateral surface of the ilium. Drill holes are useful for maintenance of the reduction clamps. Reduction clamps with points (Weber clamp) were the best for maintenance and accurate reduction. Regarding the concerns of placement of clamps, the middle to posterior combination was the best. The upper hole among the posterior holes in the ilium was the most likely to well reduce the intra-articular opening.
CONCLUSION
Transtectal was the more complicated subtype in the aspect of reduction quality. The Weber type reduction clamp was the best for reduction by centrally located holes in the quadrilateral surface and posteriorly located iliac holes in transverse acetabular fractures. The upper hole, among the posterior holes in the ilium, was the best for reduction of the fracture displacements in the intraarticular portion of acetabulum. -
Citations
Citations to this article as recorded by- Surgical outcomes of transverse acetabular fractures and risk factors for poor outcomes
Jae Hoon Jang, Nam Hoon Moon, Seung Joon Rhee, Seok Jin Jung, Tae Young Ahn
BMC Musculoskeletal Disorders.2021;[Epub] CrossRef
- Surgical outcomes of transverse acetabular fractures and risk factors for poor outcomes
- 1,359 View
- 8 Download
- 1 Crossref

- Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Osteoporotic Sacral Fracture
- Cheol hwan Kim, Young yool Chung, Seung woo Shim, Sung nyun Baek, Choong young Kim
- J Korean Fract Soc 2019;32(4):165-172. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.165
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The prevalence of osteoporotic sacral fractures is increasing. Traditionally, conservative treatment is the 1st option, but it can increase the risk of comorbidity in the elderly. To reduce the complications and allow early mobility, iliosacral screw fixation with cement augmentation will be one of the treatment options for patients with osteoporotic sacral fractures.
MATERIALS AND METHODS
This study reviewed 25 patients (30 cases) who had undergone percutaneous iliosacral screw fixation with cement augmentation for osteoporotic sacral fractures from July 2012 to December 2018 with a minimum follow up of six months. The clinical outcomes were assessed using the measures of pain (visual analogue scale [VAS] score), hospital stay and the date when weight-bearing started. All patients were evaluated radiologically for pull-out of screw, bone-union, and cement-leakage.
RESULTS
Bone union was achieved in 30 cases (100%). The mean duration of the hospital stay was 24 days (4–66 days); weight-bearing was performed on an average nine days after surgery. The VAS scores immediately (3.16) and three months after surgery (2.63) were lower than that of the preoperative VAS score (8.3) (p<0.05). No cases of cement-leakage or neurologic symptoms were encountered. Two patients (6.7%) experienced a pulling-out of the screw, but bone-union was accomplished without any additional procedures.
CONCLUSION
Percutaneous iliosacral fixation with cement augmentation will be an appropriate and safe surgical option for osteoporotic sacral fractures in the elderly in terms of early weight-bearing, pain reduction, and bone-union. -
Citations
Citations to this article as recorded by- Role of Augmentation in the Fixation of Osteoporotic Fractures
Chinmoy Das, Partha Pratim Das
Indian Journal of Orthopaedics.2025; 59(3): 294. CrossRef
- Role of Augmentation in the Fixation of Osteoporotic Fractures
- 989 View
- 4 Download
- 1 Crossref

- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
- So Young Kim
- J Korean Fract Soc 2019;32(2):89-96. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.89
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This paper reviewed the safety and effectiveness of anchor augmentation with bone cement in osteoporotic femoral fractures.
MATERIALS AND METHODS
A systematic review was conducted by searching multiple databases including five Korean databases, Ovid-MEDLINE, Ovid-EMBASE, and Cochrane Library. Safety was assessed through the incidence of complication. The effectiveness was assessed through the failure rate of anchor fixation, improvement of function and radiological assessment (sliding distance of lag screw and cutout). The safety and effectiveness of anchor augmentation with bone cement were assessed by reviewing all articles reporting on the treatment. Two researchers carried out independently each stage from the literature search to data extraction. The tools of Scottish Intercollegiate Guidelines Networks were used to assess the quality of studies.
RESULTS
Six studies were considered eligible. The safety results revealed a small amount of cement leakage (1 case), but no other severe complications were encountered. Regarding the effectiveness, the failure rate of anchor fixation was 16.7% and the Harris's hip score showed no significant improvement. The sliding distance of the anchor was similar in the cement augmentation group and non-cement group but there was no cutout.
CONCLUSION
The results of the assessment suggest that the safety is acceptable, but further research will be needed to verify the effectiveness of the treatment.
- 719 View
- 5 Download

Case Report
- Cortical Perforation Misidentified with Medial Condylar Fracture of Femur in Total Knee Arthroplasty: Case Report
- Seung Suk Seo, Sang Won Moon
- J Korean Fract Soc 2019;32(1):52-55. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.52
-
 Abstract
Abstract
 PDF
PDF - Intraoperative fracture in total knee arthroplasty (TKA) is a rare complication. However, when it happens, additional surgery to fix the fracture site is needed. Therefore, it is important to diagnose intraoperative fractures in TKA exactly. The authors experienced two cases of cortical perforation of medial femoral condyle misidentified as the fracture in TKA. Cortical perforation could be misdiagnosed as the fracture, which could lead to unnecessary surgery. This is the first report about cortical perforation in TKA. We report two cases of intraoperative cortical perforations and describe the radiological characteristics.
- 666 View
- 1 Download

Original Article
- Risk Factors for Knee Stiffness in Distal Femoral Fractures
- Dong Wook Son, Hyoung Soo Kim, Woo Young Choi
- J Korean Fract Soc 2018;31(4):123-131. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.123
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aims of this study were to evaluate risk factors for knee stiffness after the fixation of distal femoral fractures, and to analyze the clinical and radiologic outcomes.
MATERIALS AND METHODS
This is a retrospective case control study of 104 consecutive patients who have a distal femoral fracture and were treated with a submuscular locking plate. The case group comprised of patients with 12-month postoperative range of motion (ROM) ≤90° or a history of manipulation under anesthesia. The case group was compared with the control group of patients with a 12-month postoperative ROM >90°. The possible risk factors were evaluated by univariate and logistic regression analysis. The postoperative ROM and Knee Society clinical rating system was evaluated for the clinical assessment and the distal femoral angle on a whole-extremity scanogram was measured for radiologic assessments.
RESULTS
Fifty-four patients were included in the study (14 in the case group, 40 in the control group). Univariate analysis showed that comminuted fracture, intra-articular fracture, open fracture, temporary external fixation, severe osteoarthritis, and prolonged immobilization placed patients at an increased risk for knee stiffness. On the other hand, multivariate logistic regression showed that an extensor mechanism injury was the only significant predictor (p=0.001; odds ratio, 42.0; 95% confidence interval, 5.0–350.7). The ROM and Knee Society score were significantly lower in the case group; however, the coronal alignment was similar in the case and control group.
CONCLUSION
Various factors that delay postoperative knee motion place patients at increased risk of knee stiffness. Understanding these risk factors may help surgeons prevent postoperative knee stiffness after distal femoral fractures. In particular, extensor mechanism injury, such as patella fracture or open quadriceps injury, was found to be an independent predictable factor associated with knee stiffness. -
Citations
Citations to this article as recorded by- A Comprehensive Approach to Stiffness in Total Knee Arthroplasty
Brian P. Chalmers, Linda I. Suleiman, Peter K. Sculco, Matthew P. Abdel
The Journal of Arthroplasty.2025; 40(9): S59. CrossRef - Staged Management for Distal Femur Fractures: Impacts on Reoperation, Stiffness, and Overall Outcomes
Matthew T. Yeager, Robert W. Rutz, Alex Roszman, Gerald McGwin, James E. Darnley, Joseph P. Johnson, Clay A. Spitler
Journal of Orthopaedic Trauma.2024; 38(11): 577. CrossRef - Outcome of the Masquelet Technique for Complex Bilateral Distal Femoral Bone Defects
Ziad A Aljaafri, Abdullah Alzahrani, Ali Alshehri, Ahmed AlHussain, Faisal Alzahrani, Khalid Alsheikh
Cureus.2023;[Epub] CrossRef - Efficacy of non-operative treatment of patients with knee arthrofibrosis using high-intensity home mechanical therapy: a retrospective review of 11,000+ patients
Shaun K. Stinton, Samantha J. Beckley, Thomas P. Branch
Journal of Orthopaedic Surgery and Research.2022;[Epub] CrossRef - Distal Femoral Replacement and Extensor Mechanism Repair Reinforced With Synthetic Mesh for Distal Femur Fracture With Patellar Ligament Avulsion
Charles Powell, Kristopher Sanders, Neal Huang, Luis Felipe Colón, Colton Norton
Arthroplasty Today.2022; 16: 31. CrossRef - The fragility of statistical significance in distal femur fractures: systematic review of randomized controlled trials
Michael Megafu, Hassan Mian, Emmanuel Megafu, Sulabh Singhal, Alexander Lee, Richawna Cassie, Paul Tornetta, Robert Parisien
European Journal of Orthopaedic Surgery & Traumatology.2022; 33(6): 2411. CrossRef - Association Between Femoral “Spike” Size After Intramedullary Nailing and Subsequent Knee Motion Surgery
Michael G. Schloss, Nathan N. O'Hara, Syed M. R. Zaidi, Zachary D. Hannan, Dimitrius Marinos, Jared Atchison, Alexandra Mulliken, Jason W. Nascone, Robert V. O'Toole
Journal of Orthopaedic Trauma.2021; 35(2): 100. CrossRef - Distal Femur Replacement Versus Surgical Fixation for the Treatment of Geriatric Distal Femur Fractures: A Systematic Review
Brett P. Salazar, Aaron R. Babian, Malcolm R. DeBaun, Michael F. Githens, Gustavo A. Chavez, L. Henry Goodnough, Michael J. Gardner, Julius A. Bishop
Journal of Orthopaedic Trauma.2021; 35(1): 2. CrossRef
- A Comprehensive Approach to Stiffness in Total Knee Arthroplasty
- 687 View
- 10 Download
- 8 Crossref

Review Articles
- Hand Fractures
- Seokwon Yang, Jong Pil Kim
- J Korean Fract Soc 2018;31(2):61-70. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.61
-
 Abstract
Abstract
 PDF
PDF - Hand fractures are the second most common fracture in the upper extremities after the distal radius, and patients with these injuries may be experienced in hand surgery clinics. On the other hand, during the treatment of hand fractures, complications can occur due to complex functions of the hand and small-sized injuries to the bone and soft tissues. This review focused on the principles of management of these fractures, including injury mechanism, evaluations and recent treatment options. Minimally invasive surgery in various types of hand fractures, including the phalanx and metacarpal bone, is preferred because early mobilization after surgery has been emphasized to reduce complications, such as stiffness.
-
Citations
Citations to this article as recorded by- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
Dae-Geun Kim, Hyo Jun Park
Archives of Hand and Microsurgery.2023; 28(4): 239. CrossRef
- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
- 603 View
- 2 Download
- 1 Crossref

- Treatment Options for the Nonunions with Critical Sized Bone Loss
- Jin Kak Kim, Soo Hyun Kim, Jae Woo Cho, Jong Keon Oh
- J Korean Fract Soc 2017;30(2):89-101. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.89
-
 Abstract
Abstract
 PDF
PDF - The management of nonunion with severe bone loss is a challenging task to both surgeons and patients. It often requires prolonged and potentially painful treatments. Moreover, it also represents serious socioeconomic issues for patients. Inadequate fracture stability, disrupted biology, such as blood supply and soft tissue, as well as severe bone loss or presence of infection are possible reasons for nonunion. Several different treatment modalities are available, including nail dynamization, plate osteosynthesis, exchange nailing, and adjuvant alternatives, such as electrical or ultrasound stimulation. Autogenous bone graft remains the standard method to reconstruct small defects. Distraction osteogenesis and induced membrane techniques are contemporary strategies of choice for the reconstruction of larger bony defects. Herein, we attempt to describe the key techniques that may be employed in treating nonunion with severe bone loss.
-
Citations
Citations to this article as recorded by- Individualized herbal prescriptions for delayed union: A case series
Jiyoon Won, Youngjin Choi, Lyang Sook Yoon, Jun-Hwan Lee, Keunsun Choi, Hyangsook Lee
EXPLORE.2023; 19(2): 260. CrossRef
- Individualized herbal prescriptions for delayed union: A case series
- 656 View
- 3 Download
- 1 Crossref

- Bone Substitutes and the Advancement for Enhancing Bone Healing
- Dong Hyun Lee, Ji Wan Kim
- J Korean Fract Soc 2017;30(2):102-109. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.102
-
 Abstract
Abstract
 PDF
PDF - With an aging population and the development of surgical techniques, there is a growing demand for bone reconstruction in areas of trauma, arthroplasty, and spinal fusion Although autogenous bone grafting may be the best method for stimulating bone repair and regeneration, there are still problems and complications, including morbidity related to bone harvesting and limitation of harvest amount. Allogeneic bone grafts have a limited supply and risk of transmission of infectious diseases. Over the past several decades, the use of bone substitutes, such as calcium phosphate, has increased; however, they have limited indications. Biomedical research has suggested a possibility of stimulating the self-healing mechanism by locally transmitting the external growth factors or stimulating local production through a gene transfer. In this review, we evaluate recent advances, including bone graft, bone substitutes, and tissue engineering.
-
Citations
Citations to this article as recorded by- Calcium phosphate injection technique for treatment of distal radius fracture
Dae-Geun Kim, Byung Hoon Kwack
Medicine: Case Reports and Study Protocols.2021; 2(9): e0117. CrossRef - Experimental Study ofDohongsamul-tang(Taohongsiwu-tang) on Fracture Healing
Hyun Ju Ha, Min-Seok Oh
Journal of Korean Medicine Rehabilitation.2020; 30(2): 47. CrossRef
- Calcium phosphate injection technique for treatment of distal radius fracture
- 664 View
- 0 Download
- 2 Crossref

- Treatment Strategy of Infected Nonunion
- Hyoung Keun Oh
- J Korean Fract Soc 2017;30(1):52-62. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.52
-
 Abstract
Abstract
 PDF
PDF - The management of infected nonunion is based on a detailed evaluation of patients, the involved bone and soft tissues, stability of fixation, and type of bacterial pathogens. Preoperative surgical planning and strategies for each step is mandatory for the successful treatment of infected nonunion. The radical debridement of infected tissues, including the unstable implant, is one of the most important procedures. Adequate soft tissue coverage should be considered for the appropriate management of infection; a reconstructive procedure and stable skeletal stabilization by internal or external fixation is also necessary later. A restoration of bone defects and bony union can be accomplished with bone grafting, distraction osteogenesis, vascularized fibular grafting, and induced membrane technique.
-
Citations
Citations to this article as recorded by- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
Journal of the Korean Fracture Society.2023; 36(4): 148. CrossRef - The Antibiotic Cement Coated Nail and Masquelet Technique for the Treatment of Infected Nonunion of Tibia with Bone Defect and Varus Deformity: A Case Report
Min Gu Jang, Jae Hwang Song, Dae Yeung Kim, Woo Jin Shin
Journal of the Korean Fracture Society.2022; 35(1): 26. CrossRef
- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
- 1,591 View
- 31 Download
- 2 Crossref

Case Report
- Decompressive Sacral Foraminotomy for Nerve Root Injury during Conservative Treatment of Sacral Fracture: A Case Report
- Jung Gil Lee, Jae Hyuk Shin, Kwon Kim, Sang Min Choi, Moon Soo Park, Ho Guen Chang
- J Korean Fract Soc 2017;30(1):24-28. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.24
-
 Abstract
Abstract
 PDF
PDF - A 35-year-old woman visited the emergency department for a pedestrian traffic accident. Severe tenderness was noted at the posterior sacrum area, without open wound or initial neurologic deficit. Fracture of the left sacral ala extended to the S1 foramen, anterior acetabulum, and pubic ramus. Two weeks after the injury, she presented aggravating radiculopathy with the weakness of the left great toe plantar flexion. The S1 nerve root was compressed by the fracture fragments in the left S1 foramen. Decompressive S1 foraminotomy was performed. The postoperative follow-up computed tomography scan showed successful decompression of the encroachment, and the patient recovered well from the radiculopathy with motor weakness. She was able to resume her daily routine activity. We suggest that early decompressive sacral foraminotomy could be a useful additional procedure in selective sacral zone II fractures that are accompanied by radiculopathy with a motor deficit.
- 481 View
- 5 Download

Original Article
- Treatment of Wide Gap Non-Unions in Lower Extremities
- Doohoon Sun, Byeong Seop Park, Taehyeon Jeon, Seung Koo Rhee
- J Korean Fract Soc 2017;30(1):1-8. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the end results of the treatment for patients with wide gap non-unions of the long bones in the lower extremities.
MATERIALS AND METHODS
A total of 62 cases of wide gap unions, with a mean age of 38 years, were included for analysis. Study cohort included six children under the age of seven years. The average size of established bone defect was 7 cm (4-23 cm). Bone defects under 7 cm were treated with plating and various bone grafts, and those over 7 cm were managed with vascularized fibular graft (VFG), distraction-osteogenesis, tibial strut, plating and etc. Two boys with a defect of the whole tibia but with an intact fibula were treated with tibialization of intact fibula and with rotation-plasty of the leg. Their end results were evaluated by the time of bony union in accordance with the treatment of defect size of the long bone as well as their age.
RESULTS
Bony unions were obtained for an average period of at least 27 months. Fifty-one cases showed an average leg-length discrepancy of 2.8 cm, and 11 cases showed no leg-length discrepancy. The VFG, distraction-osteogenesis, and tibial cortical-strut graft and plating were the most effective methods for non-unions of wide, long bone defections (>7 cm). The prognosis was more favorable in children, muscular femur, and in cases with tibial defect but intact fà bula.
CONCLUSION
Various bone union techniques should be considered carefully, considering the ages of patients and the size of bone defects. Due to severe physical and mental disabilities of patients during the long-treatment period, specialized orthopedic doctors for trauma and mental care were necessary.
- 432 View
- 5 Download

Review Articles
- Fractures of the Tarsal Bone
- Young Hwan Park, Hak Jun Kim, Soo Hyun Kim
- J Korean Fract Soc 2016;29(4):276-282. Published online October 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.4.276
-
 Abstract
Abstract
 PDF
PDF - Fractures of the tarsal bone, such as the navicular, cuboid, and cuneiform, are very rare. These injuries can lead to serious walking difficulties due to pain and deformity of the foot with delayed diagnosis of tarsal bone fractures during an injury to multiple lower extremities. The diagnosis can be done on simple radiographs. Sometime weight bearing radiographs or stress radiographs may be needed for further evaluation. Computed tomography is the most widely available diagnostic tool. Navicular and cuneiform account for the medial column of the foot, whereas cuboid for the lateral column. The treatment of tarsal bone fractures is primarily conservative management, but operative treatment is recommended for intra-articular displacement, dislocation, or shortening of the medial or lateral column of the foot. The operative treatments include screw fixation, plate fixation, or external fixation. Complications include malunion, nonunion, posttraumatic arthritis, avascular necrosis, and deformity of the foot. Tarsal bone fracture has to be evaluated carefully to prevent serious complications.
-
Citations
Citations to this article as recorded by- Effects of Acupuncture Treatment and Taping Therapy After Lisfranc Joint Injuries: A Case Report
Shin-Ae Kim, Su-Woo Kang, Eun-Ji Lee, Min-Kyung Kwak, Hui-Gyeong Jeong, Jae-Uk Sul
Journal of Acupuncture Research.2017; 34(4): 197. CrossRef
- Effects of Acupuncture Treatment and Taping Therapy After Lisfranc Joint Injuries: A Case Report
- 2,211 View
- 27 Download
- 1 Crossref

- Biomechanics of the Wrist
- Young Ho Shin, Young Ho Lee
- J Korean Fract Soc 2016;29(1):93-100. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.93
-
 Abstract
Abstract
 PDF
PDF - The wrist joint is a complicated structure composed of many bones and ligaments. Therefore, understanding the anatomy and the biomechanics of the wrist is important in order to administer proper treatment for patients. To easily understand the complicated structure, there were many trials to unite the complicated structure with a simple group such as the carpal row concept and the carpal column concept. Movement and load transfer along the wrist joint occurs with balanced action between carpal bones. To evaluate this static equilibrium, measuring tools such as carpal height ratio are used. When wrist flexion/extension occurs, each carpal row moves synchronously with action of the scaphoid. In contrast with flexion/extension, when wrist radial deviation/ulnar deviation occurs, the proximal carpal row moves in the sagittal plane, instead of the coronal plane. Recently, the dart throwing motion which occurred from the position of dorsiflexion with radial deviation to volar flexion with ulnar deviation is considered the main movement of the wrist joint.
-
Citations
Citations to this article as recorded by- Fractal geometry in wrist biomechanics: A preliminary study with implications for arthroplasty and surgery
Lauren Gorelick, Amir Oron, Gil Gannot, Raphael Israeli
Hand Surgery and Rehabilitation.2025; 44(4): 102203. CrossRef - Association between carpal height ratio and ulnar variance in normal wrist radiography
Anas AR Altamimi, Monther A. Gharaibeh, Muntaser Abu Shokor, Moh’d S. Dawod, Mohammad N. Alswerki, Omar M. Al-Odat, Raghda H. Elkhaldi
BMC Musculoskeletal Disorders.2024;[Epub] CrossRef - Reliability and concurrent validity of a new iPhone® goniometric application for measuring active wrist range of motion: a cross‐sectional study in asymptomatic subjects
Mohammad Reza Pourahmadi, Ismail Ebrahimi Takamjani, Javad Sarrafzadeh, Mehrdad Bahramian, Mohammad Ali Mohseni‐Bandpei, Fatemeh Rajabzadeh, Morteza Taghipour
Journal of Anatomy.2017; 230(3): 484. CrossRef
- Fractal geometry in wrist biomechanics: A preliminary study with implications for arthroplasty and surgery
- 3,476 View
- 123 Download
- 3 Crossref

Original Articles
- Operative Treatment of Pediatric Distal Forearm Bothbone Fracture
- Sang Uk Lee, Changhoon Jeong, Il Jung Park, Jaeyoung Lee, Seman Oh, Kyung Hoon Lee, Sanghyun Jeon
- J Korean Fract Soc 2015;28(4):237-244. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.237
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Pediatric patients with distal forearm bothbone fractures of surgical indication were treated with the Kapandji reduction technique for radius and flexible intramedullary nail for ulna at our institution. The purpose of this study is to evaluate clinical and radiological results.
MATERIALS AND METHODS
From February 2012 to June 2014, we retrospectively evaluated 16 out of 18 cases with distal forearm bothbone fractures treated with the Kapandji reduction technique for radius and flexible intramedullary nail for ulna with at least 1-year follow-up. The average age at operation was 9.1 years (7-13 years).
RESULTS
Adequate reduction for both radius and ulna was achieved for all cases, and none of the cases showed re-displacement until the last follow-up. Mean 6.6 weeks lapsed until bony union was observed for the radius. For the ulna, the mean was 6.5 weeks. All patients gained full wrist range of motion at the last visit.
CONCLUSION
For pediatric distal forearm bothbone fractures, intrafocal Kapandji reduction and internal fixation with Kirschner wire for radius and reduction and internal fixation with a flexible intramedullary nail for ulna is the technique for handy reduction. Use of this technique can prevent re-displacement during the union process and achieve excellent clinical and radiologic results.
- 431 View
- 1 Download

- Treatment of the Communited Distal Radius Fracture Using Volar Locking Plate Fixation with Allogenic Cancellous Bone Graft in the Elderly
- Je Kang Hong, Chang Hyun Shin
- J Korean Fract Soc 2015;28(1):8-16. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.8
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We studied results of the communited distal radius fracture treated with allogenic cancellous bone graft and volar locking plate in the elderly.
MATERIALS AND METHODS
We studied 29 cases of communited distal radius fracture treated with allogenic cancellous bone graft and volar locking plate from April 2009 to April 2013. Fracture was classified according to AO/OTA classification. Postoperative clinical evaluation was performed with measurement of wrist range of motion (ROM) at last follow-up, modified Mayo wrist scoring system (MMWS), and visual analogue pain scale (VAS). Radiologic evaluation was performed with measurement of radial length on immediate postoperation and last follow-up, radial inclination, volar tilt and ulnar variance checked at the last follow-up using Sarmiento criteria.
RESULTS
Using the MMWS, 13 cases were classified as 'good', 10 'fair', and 5 'normal'. The average wrist ROM was 88.5% for flexion, 92.2% for extension, 90.5% for adduction, and 94.0% for abduction. The average VAS was 1.7. On the last follow-up, average radius length, radial inclination and volar tilt did not show statistically significant improvement (p>0.05) compared to immediate post operation measurements, and according to Sarmiento criteria, 5 cases were classified as 'good', 14 'fair', and 7 'normal'.
CONCLUSION
Treatment of severe communited distal radius fracture accompanied by bone defect with volar locking plate and allogenic cancellous bone graft is a satisfying and effective treatment method in the elderly.
- 863 View
- 3 Download

Case Report
- Infected Nonunion of Clavicle Shaft after Operation: A Case Report
- Ho Su Jang, Suk Hwan Jang
- J Korean Fract Soc 2015;28(1):77-81. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.77
-
 Abstract
Abstract
 PDF
PDF - The infected nonunion of clavicle with bone defect is an uncommon complication following clavicle shaft fracture. There were a few reports regarding treatment of the infected nonunion after clavicle fracture. We report on a case of infected clavicle nonunion successfully treated with autologous bone graft and dual plate fixation.
- 713 View
- 3 Download

Original Articles
- Concomitant Carpal Injuries in Distal Radius Fractures: Retrospective Analysis by Plain Radiographs and Computed Tomography
- Chul Hyun Cho, Eun Seok Son
- J Korean Fract Soc 2015;28(1):1-7. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the incidence and characteristics of concomitant carpal bone fractures and ligament injuries and to analyze risk factors for carpal injuries in patients with distal radius fractures.
MATERIALS AND METHODS
A total of 362 patients with 379 distal radius fractures were reviewed retrospectively. Associated carpal bone fractures and ligament injuries were evaluated by plain radiographs and computed tomography at the time of initial trauma. Correlation between associated carpal injuries and various parameters was also analyzed.
RESULTS
Of 379 distal radius fractures, 39 cases (10.3%) had one or more carpal bone fracture and 40 cases (10.6%) had carpal ligament injuries. Overall, carpal injuries occurred in 59 cases (15.6%) distal radius fractures. Associated carpal ligament injuries showed correlation with young age and associated carpal bone fractures showed correlation with AO type B distal radius fractures. Carpal injuries including fracture and ligament injury showed correlation with male, high energy trauma, or associated injuries beyond wrist.
CONCLUSION
The incidence of concomitant carpal injuries in patients with distal radius fractures is relatively high. Concomitant carpal injuries were more common in young age, male, high energy trauma, AO type B distal radius fractures, or associated injuries beyond wrist. -
Citations
Citations to this article as recorded by- Korean Medicine Treatments for the Angular Deformity of Wrist Fracture with Disuse Osteopenia: A Case Report
Myung Jin Oh
Korean Journal of Acupuncture.2018; 35(4): 234. CrossRef - Comparison of Distal Radius Fractures with or without Scaphoid Fractures
Jin Rok Oh, Dong Woo Lee, Jun Pyo Lee
Journal of the Korean Society for Surgery of the Hand.2016; 21(1): 23. CrossRef
- Korean Medicine Treatments for the Angular Deformity of Wrist Fracture with Disuse Osteopenia: A Case Report
- 965 View
- 18 Download
- 2 Crossref

- A Retrospective Comparative Study of Internal Fixation with Reconstruction Plate Versus Anatomical Locking Compression Plate in Displaced Intercondylar Fractures of Humerus
- Tong Joo Lee, Young Tae Kim, Dae Gyu Kwon, Ju Yong Park
- J Korean Fract Soc 2014;27(4):294-300. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.294
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the clinical result of a conventional reconstruction plate (CRP) fixation and locking compressive plate (LCP) fixation on the surgical treatment of an adult's displaced intercondylar fracture of humerus.
MATERIALS AND METHODS
A total of 40 patients enrolled in the study were treated between August 2002 and May 2012. Fixation with a CRP was performed in 20 patients (group A) and anatomical locking compression plate fixation was performed in 20 patients (group B). The clinical and functional evaluation was performed according to the Mayo elbow performance score and Cassebaum classification of elbow range of motion (ROM), disabilities of the arm, shoulder and hand score.
RESULTS
The Mayo elbow functional evaluation scores, eight cases were excellent, 10 cases were good, and two cases were fair in group A, and 12 cases were excellent, seven cases good, and one case fair in group B; both groups showed satisfactory results. The durations of attaining 90 to 120 degrees of the ROM of joints postoperatively were 8.3 days on average (6 to 15 days) in group A and 5.5 days on average (5 to 9 days) in group B, demonstrating a significant difference between the two groups (p=0.04). Although the correlations of clinical results according to the difference of bone mineral densities (BMDs) were not statistically significant between the two groups (p=0.35), loss of fixation occurred due to loosening of screws in two patients with low BMDs in whose operations reconstruction plates were used.
CONCLUSION
The use of locking compressive plate on the surgical treatment of an diaplaced intercondylar fracture of humerus have a good clinical results because that permits early rehabilitation through good fixation and reduces the complications such as loosening of screws.
- 413 View
- 0 Download

- Analysis of Missed Fractures in Polytrauma Patients
- Ki Chul Park, Hyun Uk Kim
- J Korean Fract Soc 2014;27(4):281-286. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.281
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to determine the frequency of missed fractures in severe multiple trauma patients and to analyze any differences in treatment plan, after whole body bone scan.
MATERIALS AND METHODS
From September 2012 to December 2013, 49 patients were confirmed to have multiple trauma with an injury severity score (ISS) of 16 or higher. Whole body bone scan was performed at an average of 15.7 days (7-25) after injury. Missed fractures were diagnosed according to physical examination and additional radiologic reports. Locations and patterns of missed fractures were analyzed. We evaluated any differences in treatment plan after the diagnosis of missed fractures.
RESULTS
Missed fractures were diagnosed in 14 patients (16 cases) on the whole body bone scan. The most frequent location was the knee (three cases), followed by rib, clavicle, carpal bone, and foot. Seven cases were occult fractures, five cases were undisplaced fractures and four cases were displaced fractures. Conservative treatment was administered in 15 patients and surgery was necessary in one patient.
CONCLUSION
Delayed or missed diagnosis of fractures occurred frequently in patients of multiple trauma with a high ISS. Whole body bone scan appears to be effective in finding missed fractures in the whole body. Definitive assessment should be supplemented after initial trauma care in order to reduce the rate of missed fractures.
- 657 View
- 4 Download

Case Reports
- Granulation Tissue Formed by Stimulating K-Wire Mimicking Tuberculous Cervical Lymphadenopathy: A Case Report
- Gu Hee Jung, Tae Hun Kim, Hyun Ik Cho
- J Korean Fract Soc 2014;27(3):227-231. Published online July 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.3.227
-
 Abstract
Abstract
 PDF
PDF - Pins and wires are still used frequently in surgeries of the shoulder; however, these can cause breakage or migration to surrounding tissues, leading to complications. We report on case of a patient with a neck mass who had a past history of pulmonary tuberculosis and distal clavicle fracture with internally fixated state. She was misdiagnosed as tuberculous cervical lymphadenopathy and treated for approximately one year, but was finally revealed as granulation tissue around the internally fixated distal clavicle fracture site, thus, mass excision and metal removal was performed. This case shows the importance of a proper selection device, internal fixation technique, duration, and close follow-up after the operation.
-
Citations
Citations to this article as recorded by- Kirschner Wire Migration into SpinaL Canal after Acromioclavicular Joint Fixation (Literature Review and Clinical Case)
D. A. Gulyaev, D. S. Godanyuk, T. A. Kaurova, P. V. Krasnoshlyk, S. V. Maikov
Traumatology and Orthopedics of Russia.2018; 24(4): 121. CrossRef
- Kirschner Wire Migration into SpinaL Canal after Acromioclavicular Joint Fixation (Literature Review and Clinical Case)
- 560 View
- 0 Download
- 1 Crossref

- Surgical Correction and Osteosynthesis for Cranial Displaced Pelvic Nonunion: Technical Note and Two Cases Report Regarding Anterior Correction and Osteosynthesis Following Posterior Release
- Kwang Cheon Choi, Ji Yoon Ha, Weon Yoo Kim
- J Korean Fract Soc 2014;27(2):151-156. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.151
-
 Abstract
Abstract
 PDF
PDF - Nonunion of an unstable pelvic fracture with cranial displacement pelvic surgery is technically difficult due to a large amount of bleeding and the risk of nerve damage. In addition, surgical correction of leg length discrepancy by reduction of a dislocated sacroiliac joint is in high demand. Nevertheless, when a patient is strongly disabled by a pelvic deformity, surgical correction may be necessary. Two patients with pelvic deformity were treated successfully by surgical correction and osteosynthesis.
- 441 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev