Abstract
This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra-articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
-
Keywords: Bone fractures, Hand, Finger phalanges, Treatment
Introduction
Hand fractures are common, with an incidence of 3.7 cases per 1,000 males and 1.3 cases per 1,000 females, accounting for 10%–30% of all fractures [
1,
2]. Compared to the metacarpals, the fingers are more exposed to external forces, making them more susceptible to injury. Consequently, they constitute over 50% of hand fractures, with distal phalanx fractures, including tuft fractures, being the most prevalent [
3].
Hand fractures occur due to various causes. Sports-related injuries are more common in younger individuals, whereas work-related injuries tend to increase with age and are more frequently observed in adult males. Among the elderly, falls and traffic accidents are the most common causes of injury and occur more often in females [
4,
5]. However, there is ongoing debate regarding which digit is most susceptible to fracture. Some studies suggest that the fifth digit may be more vulnerable because of its anatomical structure and position, while other research indicates that the index or middle fingers may be more prone to fracture depending on the mechanism of injury and exposure factors [
5-
7]. Approximately 70% of finger fractures are reported to occur in individuals between the ages of 11 and 45 [
6].
Finger fractures are classified based on several factors, including the specific digit involved, the anatomical location of the fracture (proximal phalanx, middle phalanx, or distal phalanx), the fracture pattern (oblique, transverse, spiral, impacted, comminuted), the degree of displacement, the presence of joint involvement (fractures or dislocations), and the extent of soft tissue damage, including open fractures.
Despite the diverse and frequent patterns of finger fractures, they are often overlooked due to the small size of the bone fragments and their generally favorable healing process. However, finger fractures frequently involve complex injuries, including damage to tendons, nerves, and blood vessels, which may result in complications such as joint stiffness, weakness, malunion, traumatic arthritis, and functional sequelae of the hand. Therefore, accurate diagnosis and appropriate treatment are essential.
The goals of finger fracture treatment include achieving proper alignment, maintaining pain-free joints free from arthrosis, and ensuring a stable digit with a good range of motion (ROM) for functional movement [
8]. Nevertheless, the majority of finger fractures do not require surgical intervention [
5,
9,
10]. The three critical factors in determining the need for surgical treatment are the presence of an intraarticular fracture, the stability of the fracture, and the extent of soft tissue damage [
11,
12]. Stable extraarticular fractures can typically be managed conservatively. However, because of the wide variation in the location and pattern of finger fractures, establishing universal indications for surgical treatment is challenging [
7]. Ultimately, the decision to perform surgical intervention rests with the treating surgeon. The choice of surgical technique also varies and includes options such as metal wires, screws, plates, and external fixation devices.
This review aims to evaluate recently published studies on the treatment of fractures according to the anatomical location of the finger bones, excluding thumb fractures.
Distal Phalangeal Fracture
Distal phalangeal fractures are the most common fractures of the hand, accounting for approximately 50% of all finger fractures, according to some studies [
7,
13]. The distal phalanx is anatomically divided into the tuft, shaft, and base. In the case of distal phalangeal fractures, the surrounding soft tissue damage and its management are often more critical than the fracture itself [
14].
The tuft fracture is the most prevalent type of distal phalanx fracture and occurs at the tip, distal to the tendon attachment site. It is primarily caused by crush injuries and often presents as a comminuted fracture. Tuft fractures are typically stable and can be treated conservatively due to the protection offered by the volar pulp and the fibrous soft tissue of the nail complex on the dorsal side. Stable pin fixation may be difficult to achieve due to the frequent comminuted nature of tuft fractures, and it may actually increase the risk of infection. Even when a fragment of the fractured tuft does not unite and remains a free bone fragment, it rarely results in symptoms. In symptomatic cases involving free bone fragments, removal of the fragment is performed, or, in very limited cases, osteosynthesis may be attempted [
15]. A finger splint is applied to the distal interphalangeal (DIP) joint for 2 to 4 weeks to prevent stiffness, ensuring that the proximal interphalangeal (PIP) joint remains unaffected.
Tuft fractures are more likely to require attention to the damage to the perionychium surrounding the tuft rather than the fracture itself. Even in open fractures, the fracture can often be reduced simply by suturing the surrounding soft tissue [
16]. In particular, when the nail (nail plate) is detached and the nail bed is torn or pulled away, the nail matrix should be examined and sutured to minimize deformation of the regenerating nail. In cases of subungual hematoma without nail detachment, surgical exploration is recommended if the hematoma exceeds 50% of the total nail area [
17]. However, recent recommendations suggest that, in cases without fracture or with minimal displacement, observation or decompression via trephination is sufficient [
18]. In cases where the nail displacement is significant, damage to the adjacent nail bed may occur. Even if the fracture fragment is connected externally, if it remains covered by the nail, there is a risk of future nail deformation or infection. Therefore, the surgeon may choose to remove the nail in order to examine the nail bed and, if necessary, perform the nail bed repair [
19]. The removed nail may be sutured back to the surrounding tissue after reduction to act as a splint until a new nail grows. In cases of secondary infection due to blood or fluid accumulation beneath the reduced nail plate, moist disinfection is maintained until the sutured nail bed dries, after which the new nail can be expected to regenerate [
19].
Fractures of the shaft of the distal phalanx are commonly transverse or longitudinal in nature [
20]. When the fracture occurs at the distal attachment of the flexor tendon, a palmar flexion deformity may develop. However, in many cases of shaft fractures, the nail provides anatomical support, resulting in a stable fracture. If there is minimal displacement, surgery is typically not necessary, and a finger splint is applied for 3 to 6 weeks for immobilization. In cases of severe displacement or associated soft tissue injuries, such as damage to the nail bed, surgical intervention may be required. In such instances, the nail is removed, and the nail bed injury is assessed and repaired. The fracture can be stabilized using Kirschner-wires (K-wire). If the fixation provided by the metal pins in the distal phalanx is insufficient, K-wires may be temporarily inserted through the DIP joint for transarticular fixation to stabilize the fracture. In such situations, using relatively small K-wires measuring less than 1.1 inch is recommended to minimize cartilage damage. Once the fracture site has stabilized, the wires can be removed.
Fractures of the base of the distal phalanx most commonly present as bony mallet finger, where the proximal fragment displaces dorsally. Bony mallet finger occurs when strong axial compression or flexion forces act on the DIP joint while the PIP joint remains extended, causing the proximal fragment, where the extensor tendon inserts, to displace dorsally [
21]. A relatively rare mechanism of injury involves hyperextension of the DIP joint, leading to a dorsal impaction of the distal phalanx articular surface against the head of the middle phalanx. In such cases, the remaining distal phalanx may easily dislocate palmarly, often requiring surgical treatment. If left untreated, a bony mallet finger may progress to compensatory hyperextension of the PIP joint, resulting in a swan-neck deformity, or cause joint stiffness or posttraumatic arthritis due to intraarticular fractures. Conservative treatment may be considered when there is no displacement of the bone fragment, less than 30% involvement of the articular surface, and no subluxation of the joint. If the fracture involves 30%‒50% or more of the articular surface, instability may occur [
22]. Okafor et al. [
23] reported on 31 patients with bony mallet fingers treated conservatively, and found that 48% developed arthritis, 29% developed a swan-neck deformity, and an average of 8.3° of DIP joint drooping; however, most patients had satisfactory outcomes. The Cochrane Review also found no significant difference between conservative treatment and K-wire fixation [
24]. However, Niechajev [
25] recommended surgical treatment when the bone fragment exceeds 3 mm or there is subluxation of the DIP joint. Surgical treatment is most commonly performed using extension block K-wire fixation, first proposed by Ishiguro et al. [
26] in 1988 and later modified by various surgeons. Modified techniques include using two extension block pins to equally prevent the extension of the fractured bone fragments [
27], or passing a pin through the DIP joint in a diagonal direction or from the palmar side rather than from the fingertip to facilitate fixation [
28]. Direct fixation of the bone fragment has also been attempted [
29], and methods using dorsal metal pins for fracture reduction and fixation have been introduced (
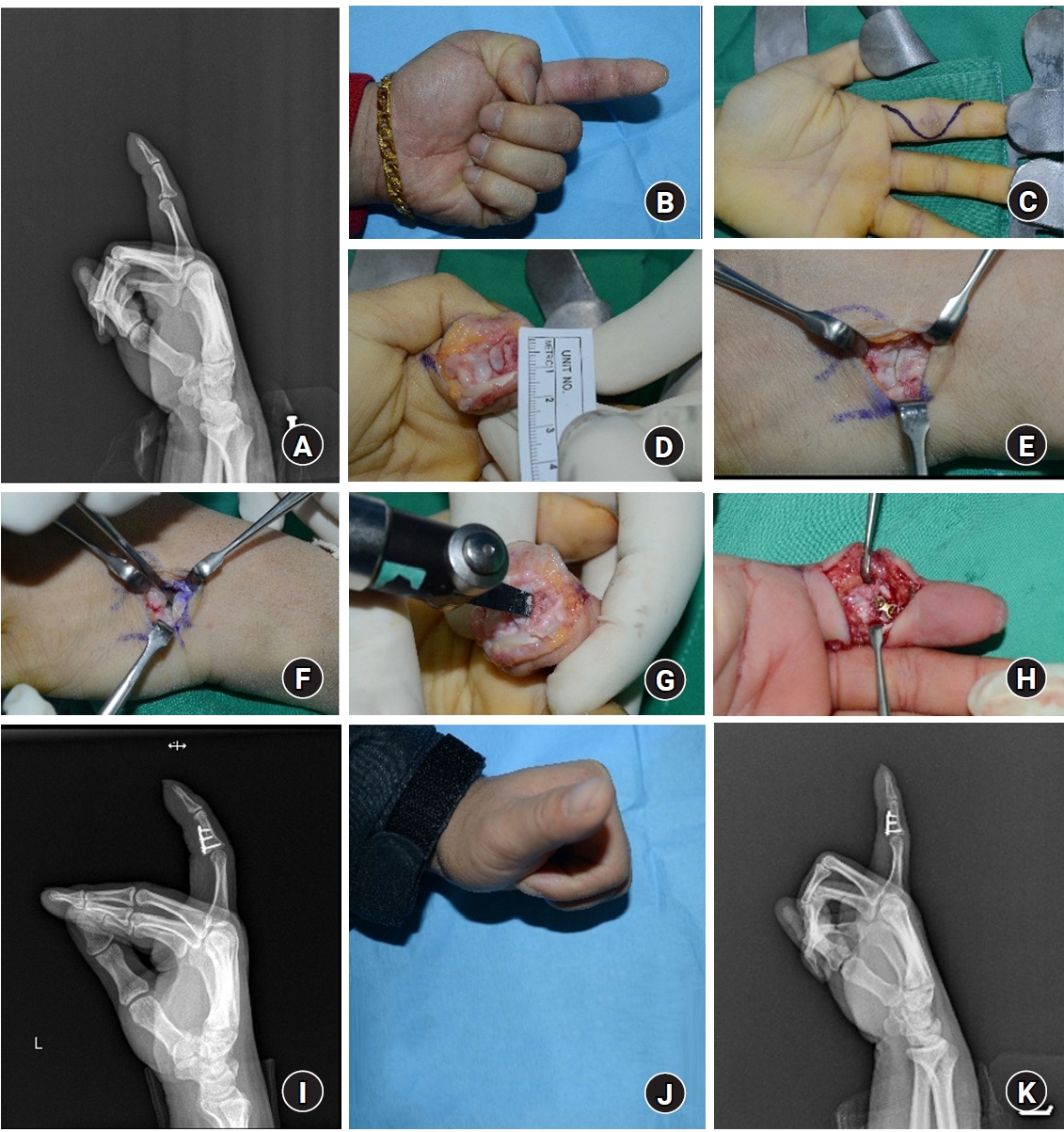
Fig. 1) [
30]. While open reduction and other devices, such as small screws, hook plates, or pull-out sutures, have been explored, these techniques are still used sparingly, and there is limited evidence to support their primary use [
31].
Jersey fractures, in contrast to bony mallet fingers, are avulsion fractures of the palmarly located base of the distal phalanx caused by the flexor tendon [
32]. These injuries typically occur due to sudden hyperextension forces while the DIP joint is actively flexed. The exact mechanism remains debated, but they are common in the fourth finger and often seen in rugby players, hence the name "Jersey" fracture (named after the sports jerseys worn by rugby players) [
21]. Unlike bony mallet fingers, which have a contentious indication for surgical treatment, Jersey fractures almost always require surgery. They are classified into five types according to the Modified Leddy and Packer system, based on the degree of displacement of the flexor tendon and the associated distal phalanx fracture [
33,
34]. In cases with small fragments or no fracture but a true flexor tendon avulsion, proximal migration can occur, even reaching the palm in severe cases (type I). Generally, the dislocation does not extend beyond the palm, from the origin of the palmar lumbricals to the proximal palm. However, if the vincular blood supply is damaged and displacement occurs to the palm (type I), contracture progresses rapidly, and diagnosis and surgery within 7 to 10 days are recommended [
21]. Type II, the most common, involves displacement to the PIP joint and is limited by the vincula longus, preventing further displacement. Larger bone fragments may become trapped at the A4 pulley (type III), further limiting displacement.
While rare, Jersey fractures can yield good outcomes with rapid diagnosis, accurate reduction of the flexor tendon or bone fragments, and secure fixation. Preoperative considerations include the degree of proximal tendon displacement, time to diagnosis, and the size of the bone fragment attached to the tendon. Depending on the fragment size, fixation may be performed using screws or pull-out sutures. Recent advances include the use of suture anchors to facilitate tendon attachment repair [
35,
36]. During active flexion of the DIP joint, forces of up to 28 N are applied, and the load-to-failure strength of pull-out suture fixation is 43 N, while a fine suture anchor can resist up to 69 N [
37]. However, the small diameter of the distal phalanx may cause the screw’s tip to penetrate the dorsal cortex, potentially irritating surrounding soft tissues such as the nail matrix [
38].
In cases where diagnosis is delayed and primary suture repair is no longer feasible, the treatment approach should be discussed with the patient based on their current condition. For injuries involving the fourth or fifth finger, where only limited flexion of the DIP joint is restricted, observation may be sufficient without further treatment. If patients complain of instability in the DIP joint, arthrodesis may be considered. In the second finger, where DIP joint flexion is crucial, tendon grafting or arthrodesis may be considered. However, these options depend on the surgeon’s experience, and the results may not always be satisfactory, which should be explained to the patient preoperatively [
21,
39].
Fractures of the Middle Phalanx and Proximal Phalanx
Head and Neck Fracture
The head of the middle and proximal phalanges are composed of two condyles that form the joint surface at the base of the distal or middle phalanx. The stability of the joint is contributed by the thick palmar plate on the palmar side, the relatively thin joint capsule and extensor tendons on the dorsal side, and collateral ligaments on both sides. Three main types of classification are commonly used based on whether fractures involve the joints and whether displacement occurs [
40]. Type I fractures are stable, nondisplaced intraarticular fractures, while type II (unilateral) and type III (bilateral) fractures, which are unstable, require surgical treatment. Depending on the degree of displacement or the size of the fracture fragment, closed or open reduction may be required, and fixation can be achieved using metal pins, mini screws, or headless screws. However, it can be difficult to achieve stable fixation when the fragment size is small, and external fixation may be applied in cases of comminuted fractures or joint instability (
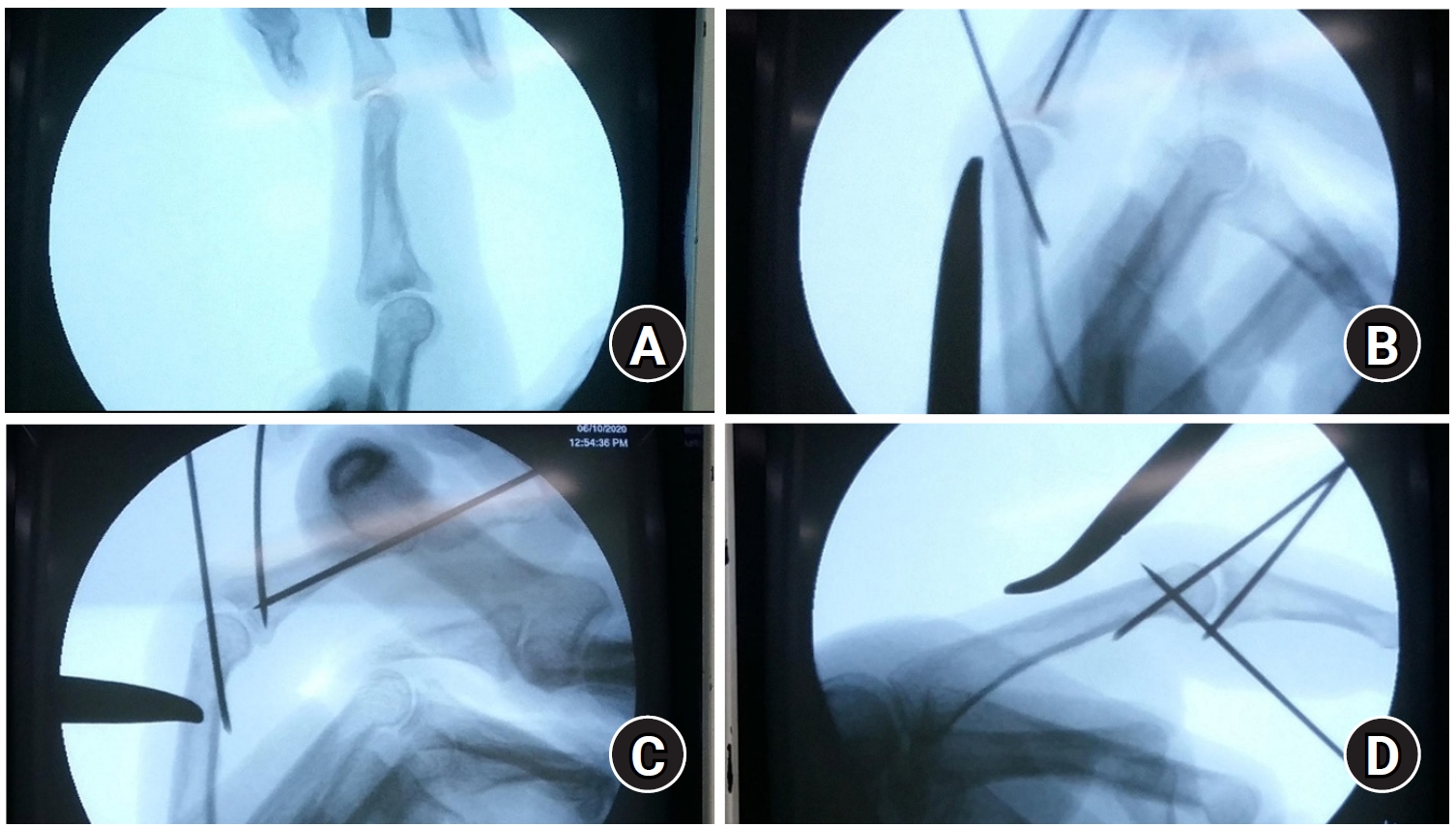
Fig. 2).
Shaft fractures can occur in various patterns, including transverse, oblique, spiral, and comminuted, depending on the type of external force applied. Nonunion is rare, as long as there is no disruption of blood circulation due to soft tissue injury. In the middle phalanx, transverse or short oblique fractures (with fracture lengths less than 2‒3 times the diameter of the phalanx) are common, while in the proximal phalanx, oblique or spiral fractures are more frequent [
41]. The location of the fracture influences the sagittal finger deformity. In the middle phalanx, fractures occurring distal to the flexor digitorum superficialis insertion lead to apex volar angulation, while those in the proximal region tend to result in apex dorsal angulation. In the proximal phalanx, apex volar angulation is caused by the central tendon on the dorsal side and the intrinsic muscles on the volar side. These deformities are crucial for the surgeon to understand when performing fracture reduction. A shortening of the bone by more than 6 mm or angulation greater than 15° may be considered an indication for surgical treatment, although this is not consistently accepted due to the complexity of the fractures [
41]. Furthermore, rotational deformity is considered more important than angulation in the sagittal plane. Rotational deformity is often difficult to assess with X-rays alone, and physical examination is necessary to evaluate whether a rotational deformity is present, helping guide the decision for surgical intervention when needed. The pattern of rotational deformity varies based on the location of the fracture, with fractures in the proximal phalanx having a longer distance to the fingertip compared to the middle phalanx, meaning even a small rotational deformity can have a significant impact at the fingertip.
A base fracture may present as a transverse fracture occurring outside of the joint, though the fracture line originating from the base can extend to an intraarticular fracture or propagate from a shaft fracture, extending to the proximal base. In intraarticular fractures, joint incongruity is a key criterion for surgical treatment decisions, as it can lead to complications such as limited joint ROM and posttraumatic osteoarthritis. These fractures are among the most difficult to treat in hand fractures.
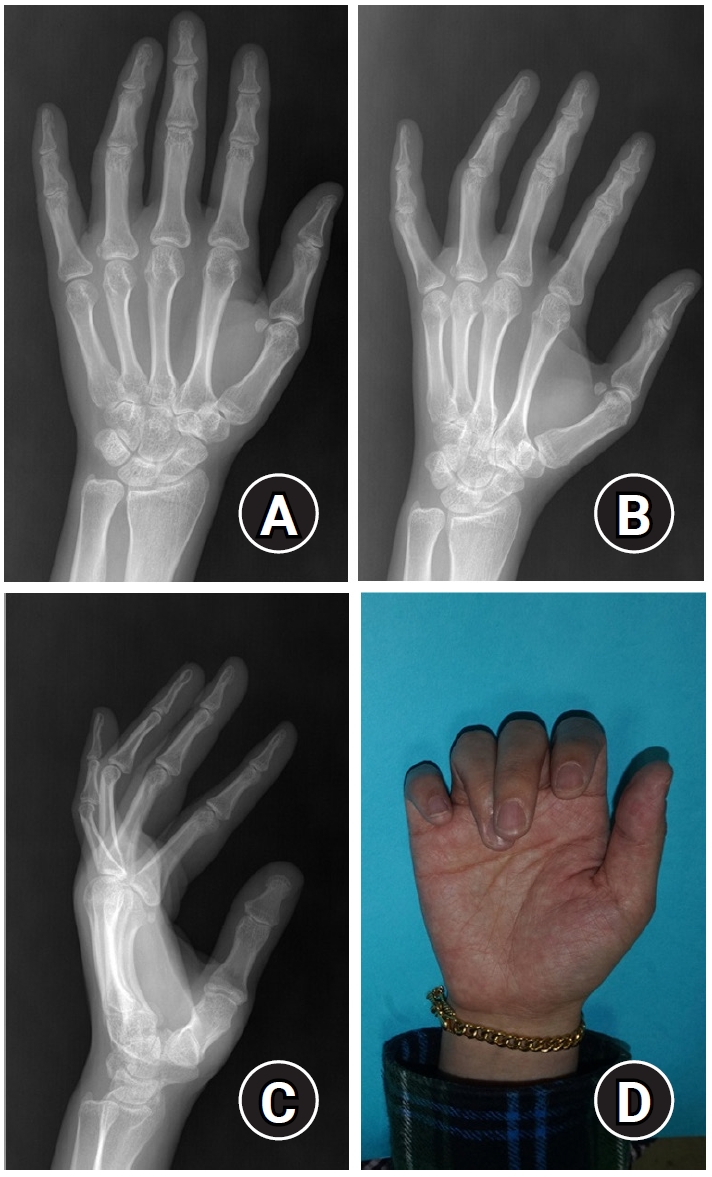
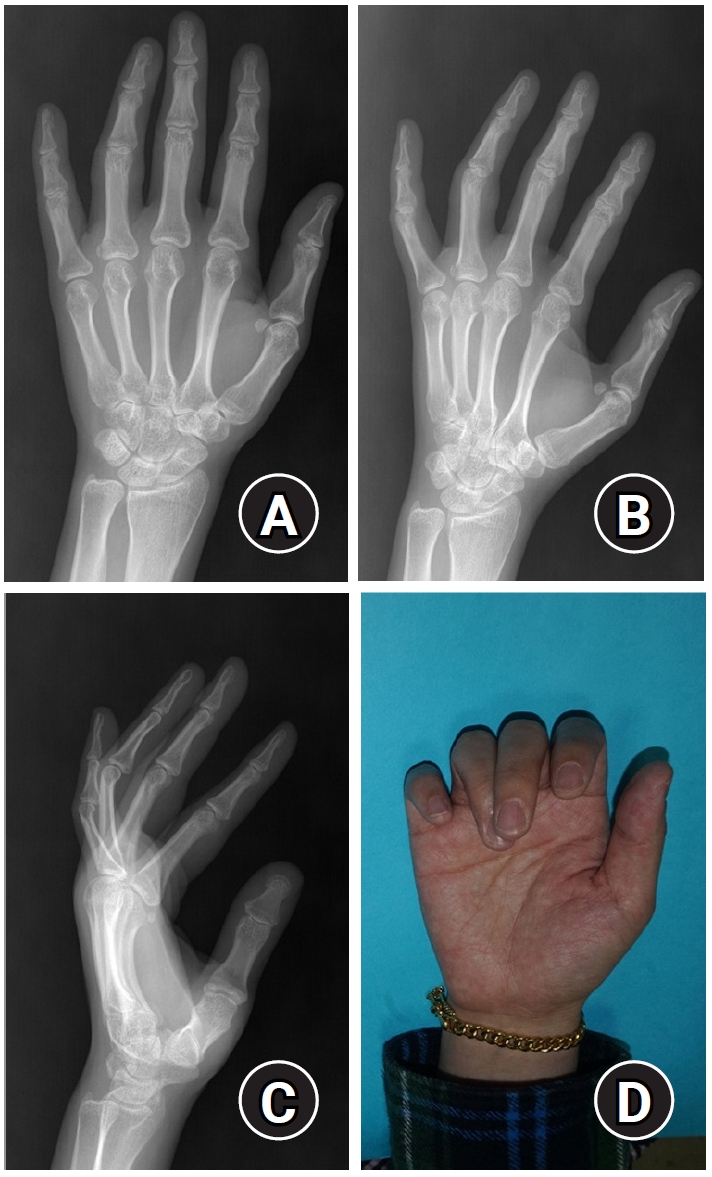
In the case of extraarticular transverse fractures of the proximal phalanx, even if the fracture does not appear severe on X-ray alone, rotational deformity may still be present. Therefore, a diagnosis should not be based solely on X-ray findings, and a thorough physical examination should be performed before surgery to prevent the complication of rotational malunion [
9] (
Fig. 3).
A common type of base fracture that typically heals without surgical intervention is the avulsion fracture. These fractures are often caused by hyperextension and occur at the base of the middle phalanx, frequently resulting in pain at the PIP joint. Unless there is additional rupture of the collateral ligaments, these fractures typically do not cause joint instability due to the small size of the bone fragments. After pain is controlled with splint fixation, good results can often be achieved with early joint movement [
42,
43].
The metacarpophalangeal (MCP) joint and PIP joints have collateral ligaments on both sides, providing stability in the coronal plane. When excessive external force is applied, collateral ligament injury may occur. However, avulsion fractures involving the middle or proximal phalanx, including the bone fragments caused by collateral ligament, are common. If the displacement of the bone fragment is less than 2 mm, conservative treatment can be pursued. However, it is more important to assess the joint instability in the coronal plane caused by functional failure of the collateral ligaments than to focus on bone fragment displacement. If instability is not present, conservative treatment using buddy taping or splint fixation is possible [
41].
In the case of an intraarticular fractures, subluxation or dislocation may occur simultaneously with displacement of bone fragments. The clinically high incidence and varied treatment outcomes of PIP joint dislocations will be discussed further.
Fractures and Dislocations of the PIP Joint
Compared to the DIP joint, which contributes less to overall finger movement, the PIP joint is a crucial component of finger function. It accounts for approximately 85% of the total ROM, about 100° of flexion and extension [
44].
Intra-articular fractures of PIP joint are classified based on the location and characteristics of the bone fragments, such as volar, dorsal, or pilon fractures, as well as direction of dislocation including dorsal, volar, or lateral dislocations. When the size of the intraarticular bone fragments is less than 30% of the joint surface, the fracture is generally considered stable. However, stability decreases as the fragment size increases. If the bone fragment covers more than 50% of the joint surface, instability may occur, requiring surgical intervention [
20,
43]. If the fracture is stable and the joint surfaces are congruent without signs of subluxation, conservative treatment, such as splint immobilization or buddy taping for 3 to 4 weeks, may be considered. Depending on the direction of instability, the immobilization position can be adjusted to limit either extension or flexion. Regular outpatient follow-up is necessary to monitor potential dislocations or further fragment displacement [
43].
The decision to pursue surgical treatment, including the choice of surgical method, should consider factors such as the location and comminution of the bone fragments, as well as the degree of dislocation. Additionally, patient factors such as age and functional needs, and the surgeon's experience, preference, and confidence must also be considered. Several surgical techniques have been reported, including closed reduction with K-wire fixation [
45], extension block pinning [
46], open reduction and internal fixation [
47], external fixation [
48], volar plate arthroplasty [
49], and hemi-hamate arthroplasty [
50]. The precise reduction of intraarticular fragment and secure fixation can promote faster recovery of joint motion and cartilage remodeling, leading to favorable results [
43,
47,
51].
However, prior studies have shown that surgical outcomes vary, with some reporting poor results. Finsen [
52] reported three cases of postoperative infection, one case of arthrodesis, and one case of amputation among 18 patients treated with Suzuki’s pins and rubber traction.
Fracture-dislocations of the PIP joint are most commonly associated with dorsal dislocations following volar fractures [
43,
47]. Even in the absence of complete dislocation, subluxation can lead to subsequent joint stiffness, emphasizing the importance of accurate diagnosis and appropriate treatment. The "V" sign, observed on lateral radiographs of the middle phalanx, can indicate subluxation when there is widening of the dorsal joint surface. In cases of subluxation, approximately 30° of flexion is possible, however as flexion progresses, instability increases, leading to further dislocation and difficulty in achieving additional flexion, which may require surgical intervention [
43]. The author’s group has reported favorable outcomes with internal fixation using small-sized plates or screws following fracture reduction via a volar approach in PIP joint dorsal fracture-dislocations (
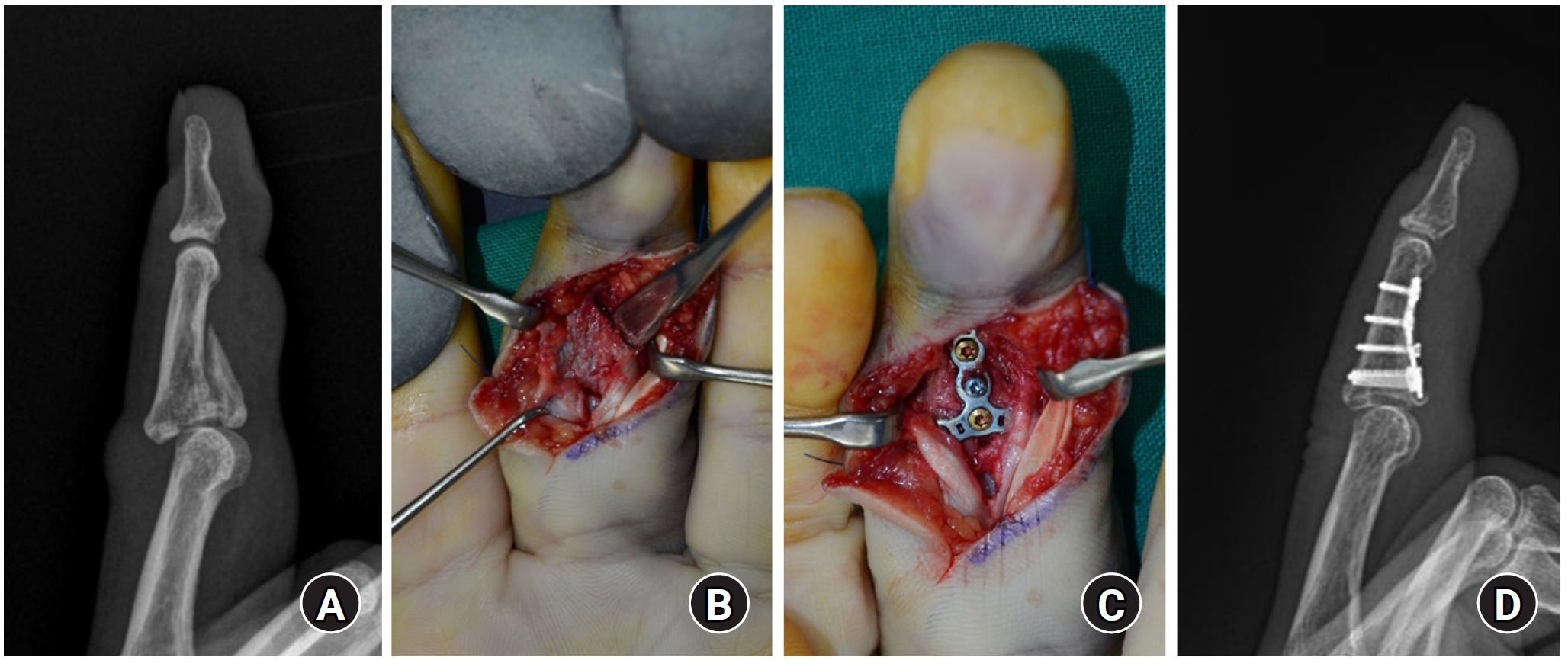
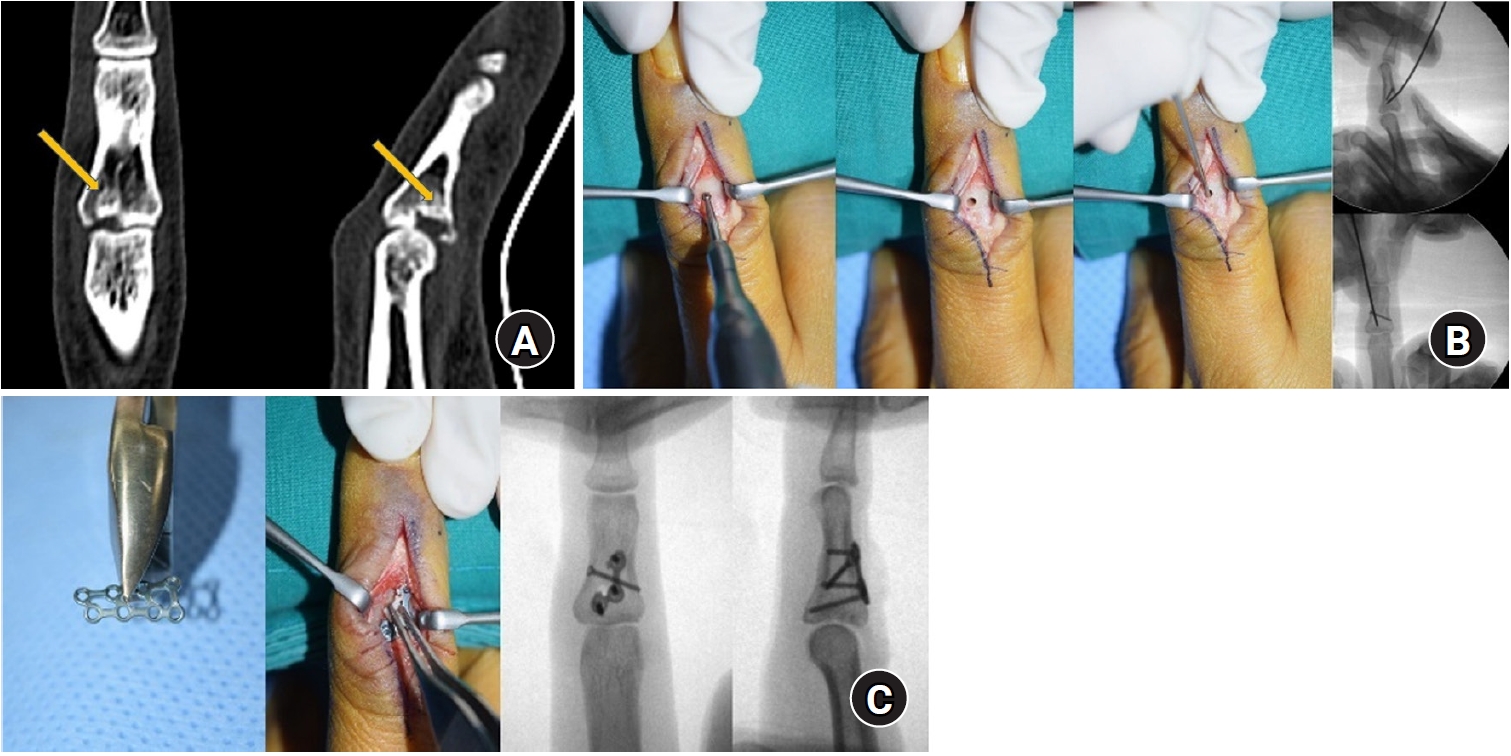
Fig. 4) [
44]. If there is significant comminution that makes joint surface preservation difficult, hemi-hamate arthroplasty using the distal hamate articular ridge may be considered (
Fig. 5) [
50].
Pilon-type fractures occur due to axial compression, leading to intraarticular fragment depression and, additionally, the separation and displacement of volar or dorsal fragments. Instability primarily increases during extension. Given the comminuted nature and displacement of intraarticular fragments, many of these fractures require surgical treatment, which is generally more challenging than other types of fracture displacement [
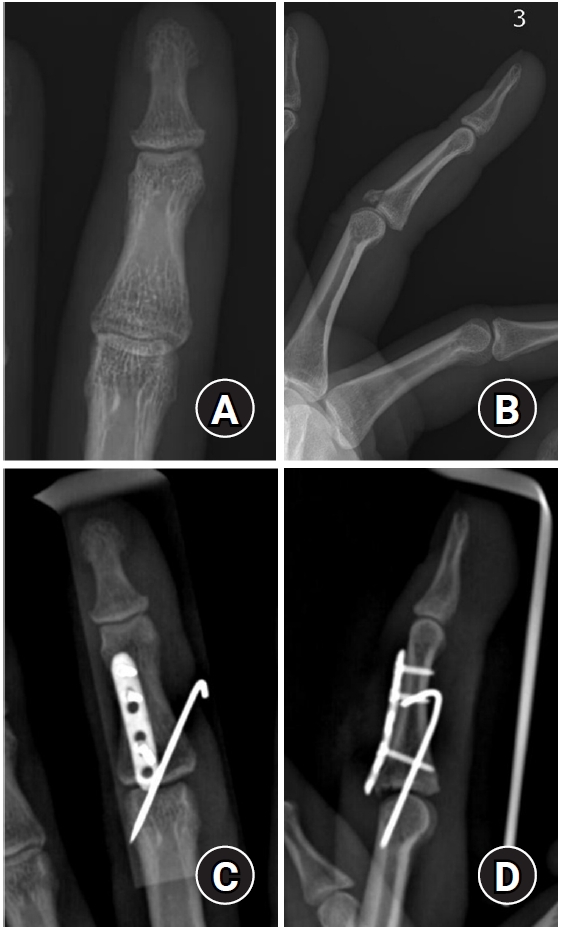
9]. A surgical approach often involves a volar approach to expose the entire base of the proximal phalanx by opening the joint capsule and fully hyperextending the PIP joint to 180° (shotgun approach), though this may result in increased soft tissue dissection. In cases where fracture displacement is not severe, closed reduction and K-wire fixation may be attempted. The depressed articular fragments can be reduced into the proximal phalanx and secured with subsequent K-wires (
Fig. 6). Recently, Park et al. [
53] reported good outcomes with a technique that does not require joint exposure, in which an extraarticular cortical window is created to perform trans-osseous reduction of the depressed intraarticular fragments, followed by fixation with low-profile locking plates (
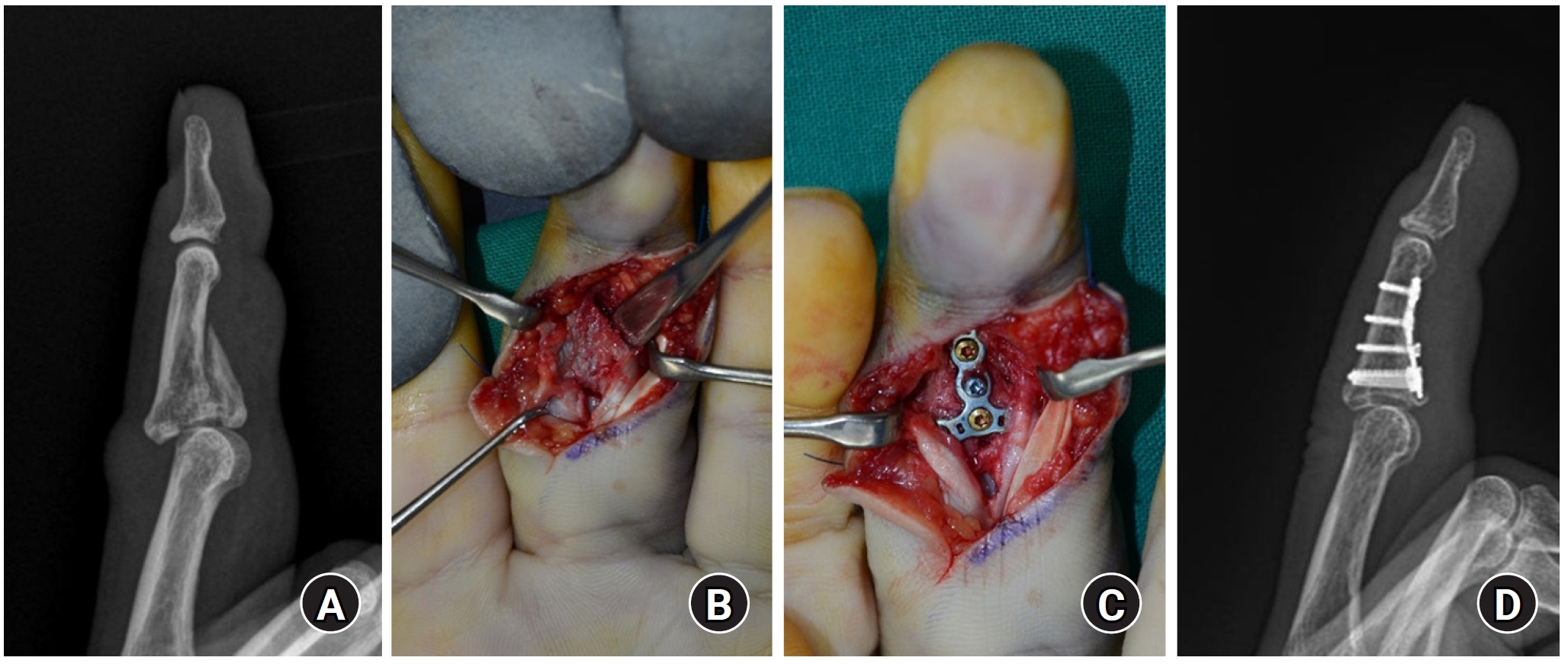
Fig. 7). This technique results in less soft tissue dissection compared to a volar approach and facilitates easier reduction of the articular fragments, ultimately enabling early joint mobilization through locking plate fixation.
Volar dislocations are relatively rare and are often associated with the attachment of the central slip to the dorsal fragment. If inadequately treated, they can result in extension lag of the PIP joint, and over time, the conjoint lateral band may shift volarly, causing hyperextension of the DIP joint and leading to a boutonniere deformity. When instability increases during flexion, when the fragment comprises more than 50% of the joint surface, or when extension is restricted or dislocation is observed during flexion, surgical treatment is indicated (
Fig. 8).
Surgical Treatment
As noted previously, the decision-making factors for surgical treatment include the presence of intraarticular fractures, the stability of the fracture, and the degree of soft tissue injury. Additionally, patient-related factors, such as high physical activity levels, occupations that require heavy use of the hands, and the dominant hand, are also considered. In such cases, more robust fixation and early rehabilitation are often prioritized. Based on the location and pattern of the fracture, a computed tomography scan is performed to assess the need for surgery and establish a surgical plan. In addition to the traditional methods of closed reduction and K-wire fixation, various other surgical techniques are available. The surgeon should select the most appropriate method based on familiarity and expertise, considering the fracture characteristics and the patient’s individual factors [
9].
The most commonly used fixation method for hand fractures is K-wire fixation. Typically, after closed reduction, K-wires are percutaneously inserted, and once the fracture site is stabilized, the pins are removed [
5,
54]. Although complications such as pin migration, loss of fracture stability, skin irritation, and potential infection may occur, these are relatively uncommon. According to Hsu et al. [
54], the reported infection rate is 7%, most of which are superficial and rarely progress to osteomyelitis or pyogenic arthritis. The main advantage of K-wire fixation over plate fixation is the reduced risk of additional soft tissue damage, as well as the avoidance of adhesions between bone and tendon, which can lead to joint stiffness. Additionally, there is no need for secondary surgery to remove the plate, making K-wire fixation the preferred choice [
55]. The inserted K-wires are typically removed at postoperative 10 to 28 days after insertion, depending on the fracture pattern, patient factors, and the surgeon’s experience [
9].
In cases where K-wire fixation alone cannot provide adequate stability, plate fixation may be used selectively. The type of plate (e.g., compression, tension band, bridge, or neutralization plate) depends on the method used to fix the fractures. When using plate fixation, it is essential that the screws do not penetrate beyond the distal cortex, to avoid causing damage to surrounding structures such as tendons, nerves, or blood vessels. After achieving stable fixation with the plate, early joint motion is encouraged. The skin incision and soft tissue dissection required for fracture reduction and plate fixation, as well as adhesions caused by the plate itself, can lead to joint stiffness, which is a significant disadvantage of plate fixation [
9]. Depending on the surgeon’s preference, some studies report better clinical outcomes with plate fixation compared to K-wire. Additionally, robust mini and low-profile metal plates with superior fixation strength have been introduced, reducing the impact on the surrounding soft tissues of the hand [
12,
41,
56]. Recent studies have also compared the use of bioabsorbable miniplates for metacarpal fractures with conventional metallic plates [
57].
Screws smaller than 2 mm can be used for fragment fixation following either closed reduction or open reduction, utilizing lag screw or neutralization screw techniques. This method is commonly used for simple oblique fractures and provides intermediate stability between K-wire and plate, making it stable enough for early rehabilitation without causing irritation from the fixation device. However, this method is difficult to apply in cases of comminuted or transverse fractures, and the risk of causing additional fractures during screw insertion may arise if the bone fragments are small. In a prospective study by Horton et al. [
58], comparing the closed reduction with K-wire fixation and open reduction with lag screw fixation for spiral or oblique fractures of the proximal metacarpal, no significant functional or radiological differences were observed between the two groups.
Recently, an intramedullary fixation technique using headless screws has been attempted following its initial introduction in 2010 by Boulton et al. [
59] The use of headless screws for intramedullary fixation offers advantages such as a small incision (2‒3 mm), high stability, minimal damage to the periosteum surrounding the fracture, and reduced soft tissue irritation from the fixation device, while also allowing direct compression of the fracture site [
60]. This method is most suitable for extraarticular transverse or short oblique shaft fractures, and it can also be applied to base fractures, comminuted fractures, and open fractures [
60]. However, it is absolutely contraindicated in cases of active infection or open growth plates, and caution should be exercised in the case of intraarticular fractures, long oblique fractures, and subchondral fractures [
61].
The surgical technique can be divided into antegrade and retrograde insertion depending on the direction of screw insertion. The antegrade approach includes two methods: the intraarticular approach, which accesses only the joint surface of the proximal metacarpal base, and the transarticular approach, which passes through the metacarpal head to fix the fracture [
62-
64]. The intraarticular method is more commonly used [
60].
The single headless screw fixation method, using the longest and thickest screw to stabilize the fracture, is often preferred. This method provides adequate fixation for simple fractures, such as transverse or short oblique shaft fractures. However, the fracture pattern can pose significant risks. In comminuted neck fractures, excessive compression from the headless screw may lead to bone shortening. Additionally, due to the relatively larger diameter of the medullary canal compared to the screw, fixation at the metaphysis may be inadequate, often necessitating the insertion of additional screws [
62,
65].
Wide-awake local anesthesia no tourniquet (WALANT) is a technique that uses a local anesthetic composed of 1% lidocaine, 1:100,000 epinephrine, and 8.4% bicarbonate to achieve both anesthesia and hemostasis simultaneously [
66]. This technique was organized and popularized by Lalonde et al. [
67], and has been widely applied in hand surgery. Since WALANT does not require a tourniquet, it avoids the pain associated with tourniquet use and allows for real-time assessment of hand function during surgery. This makes it particularly useful for tendon surgeries and has also been increasingly applied in hand fracture surgeries [
67]. However, its effectiveness in finger fractures may be limited because, even before WALANT, local anesthesia was sufficient for performing surgery while assessing joint motion. Additionally, a finger tourniquet can create a bloodless field without the need for epinephrine. Although WALANT theoretically has broad applicability for all local anesthesia surgeries in hand fractures, it is considered particularly useful in cases where a finger tourniquet is difficult to apply, such as with fractures of the proximal phalanx shaft or base.
Complications
Stiffness
Stiffness is the most common complication following hand fractures [
11,
56]. It can affect not only the injured finger but also adjacent digits or even the entire hand [
41]. Contributing factors include swelling and soft tissue damage resulting from trauma, infection, surgery-induced injury, or vascular dysfunction [
56,
68]. Notably, prolonged immobilization—regardless of whether surgery was performed—is strongly associated with stiffness [
11]. In the past, some physicians believed that refraining from finger joint motion for up to 6 to 8 weeks, until the late 1970s, was the best approach for healing [
51]. However, joint stiffness resulting from prolonged immobilization can cause pain and burden for both the patient and physical therapist during rehabilitation, and in some cases, secondary surgeries such as capsular release or tenolysis may be required. These secondary procedures, however, do not always yield optimal results.
Early joint motion can help alleviate swelling and reduce stiffness [
11,
68]. Musculoskeletal tissues require adequate movement and stress to maintain health. The timing and method of initiating joint motion depend on the fracture pattern and fixation technique, and therefore, there are no standardized guidelines. In the case of unstable fractures, it is necessary to provide rigid fixation followed by early mobilization [
69]. Generally, radiographic stability with callus formation is observed several weeks after achieving real fracture site stability, so it is recommended to begin joint motion around 2 to 4 weeks after pin removal [
9].
The immobilization position is also important. A common limitation in finger motion occurs in the MCP joint, where flexion is often restricted due to the "cam effect", while in the PIP joint, extension is more frequently limited. For hand fractures, preventing future finger stiffness is best achieved by immobilizing the MCP joint at 50°–70° of flexion and the PIP joint from 15° to full extension, thereby maintaining the intrinsic positive position [
8].
Malrotation and malunion in the coronal plane tend to result in poorer outcomes compared to sagittal plane malunion, as overlap between the fingers due to malunion can lead to significant functional impairments [
56]. No standardized method currently exists to objectively assess the degree of rotational alignment in the fingers for guiding corrective surgery. With MCP and PIP joint flexion, finger overlapping or scissoring is regarded as malrotation [
70-
72]. Furthermore, on this position, second to fifth ray fingertip point can converge to scaphoid tubercle [
72,
73], which may warrant reoperation [
74]. Therefore, malunion should be assessed early in the course of fracture healing or immediately after surgical fixation. Under general anesthesia, when active finger flexion is not possible, passively extending the wrist causes the fingers to flex due to the tension in the flexor tendons. This maneuver helps detect any overlap between the fingers, which may indicate a rotational deformity.
Nonunion of phalangeal fractures is uncommon, with a reported incidence of around 1% [
56]. Factors that influence fracture healing include the fracture pattern including bone loss, stability, soft tissue damage such as open fractures, vascular injury, and fixation in a distracted fracture site. Although it may take considerable time to confirm fracture union and radiographic fracture lines can be visible for as long as 1 year, clinical signs and symptoms such as instability, gross deformity, implant failure, and persistent pain are far more important in determining nonunion [
56].
While radiographic nonunion does not always lead to clinical complications, intervention is required when symptoms such as pain are present. Treatment options include osteosynthesis with bone grafting, arthrodesis, and amputation [
7]. When osteosynthesis is attempted, careful preparation of the fracture ends is essential. Fenestration drilling can promote endosteal circulation at the fracture site, followed by placement of bone grafts in the prepared space. Although the fixation techniques used to restore normal anatomy in cases of nonunion are similar to those used for primary fracture treatment, it is advisable to pursue more stable fixation.
Conclusions
The goal of treatment for hand fractures is to maintain the normal alignment of the fractured finger, achieve a pain-free state, and restore the full ROM to ultimately return the finger to its pre-injury condition. The treating physician decides between conservative and surgical treatment. When conservative treatment is chosen, decisions must be made regarding immobilization methods and the timing for initiating joint motion, and it is necessary to monitor any displacement through outpatient follow-up. When surgical treatment is chosen, it is important to understand the characteristics of the fracture to determine how to approach fracture fixation and which method to use. Postoperatively, it is essential to check for infections at the surgical site and for any displacement of the fixation, while reducing the risk of stiffness through ROM exercises at the appropriate time.
Article Information
-
Author contributions
Conceptualization: HTK, JKL. Formal analysis: JKL. Methodology: HTK. Project administration: JKL. Supervision: JKL. Validation: HTK, JKL. Writing-original draft: HTK. Writing-review & editing: JKL. All authors read and approved the final manuscript.
-
Conflicts of interest
Jun-Ku Lee is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
-
Funding
None.
-
Data availability
Not applicable.
-
Acknowledgments
We would like to express our sincere gratitude to Dr. Soo-Hong Han (Department of Orthopedic Surgery, CHA Bundang Medical Center), and Dr. Jong Woong Park (Department of Orthopedic Surgery, Korea University Anam Hospital) for providing the surgical images used in this review article.
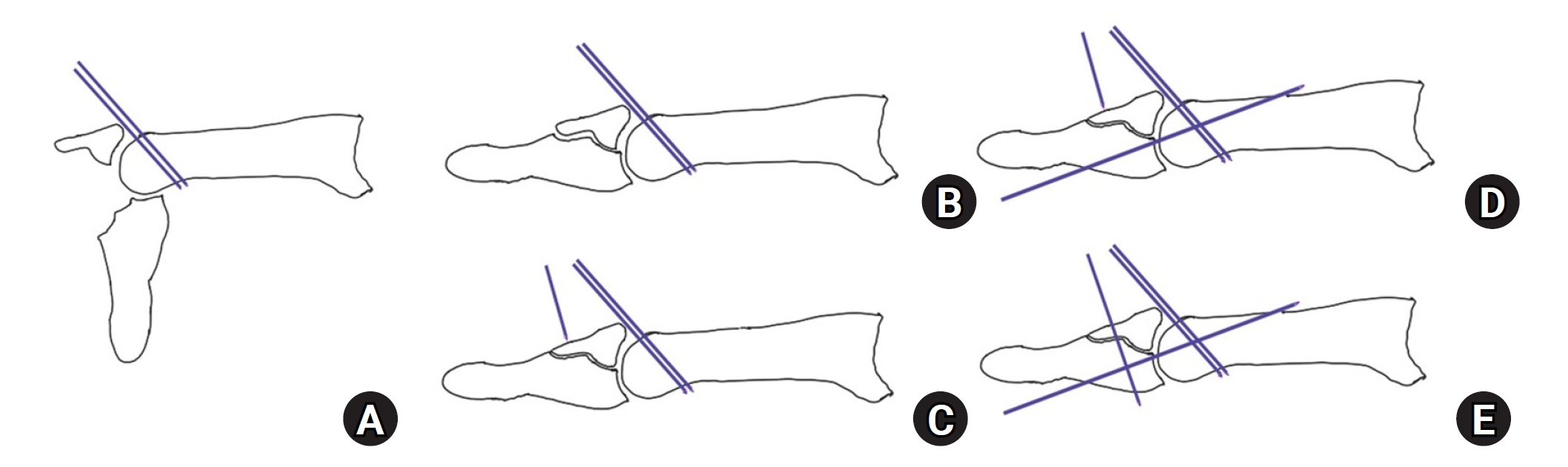
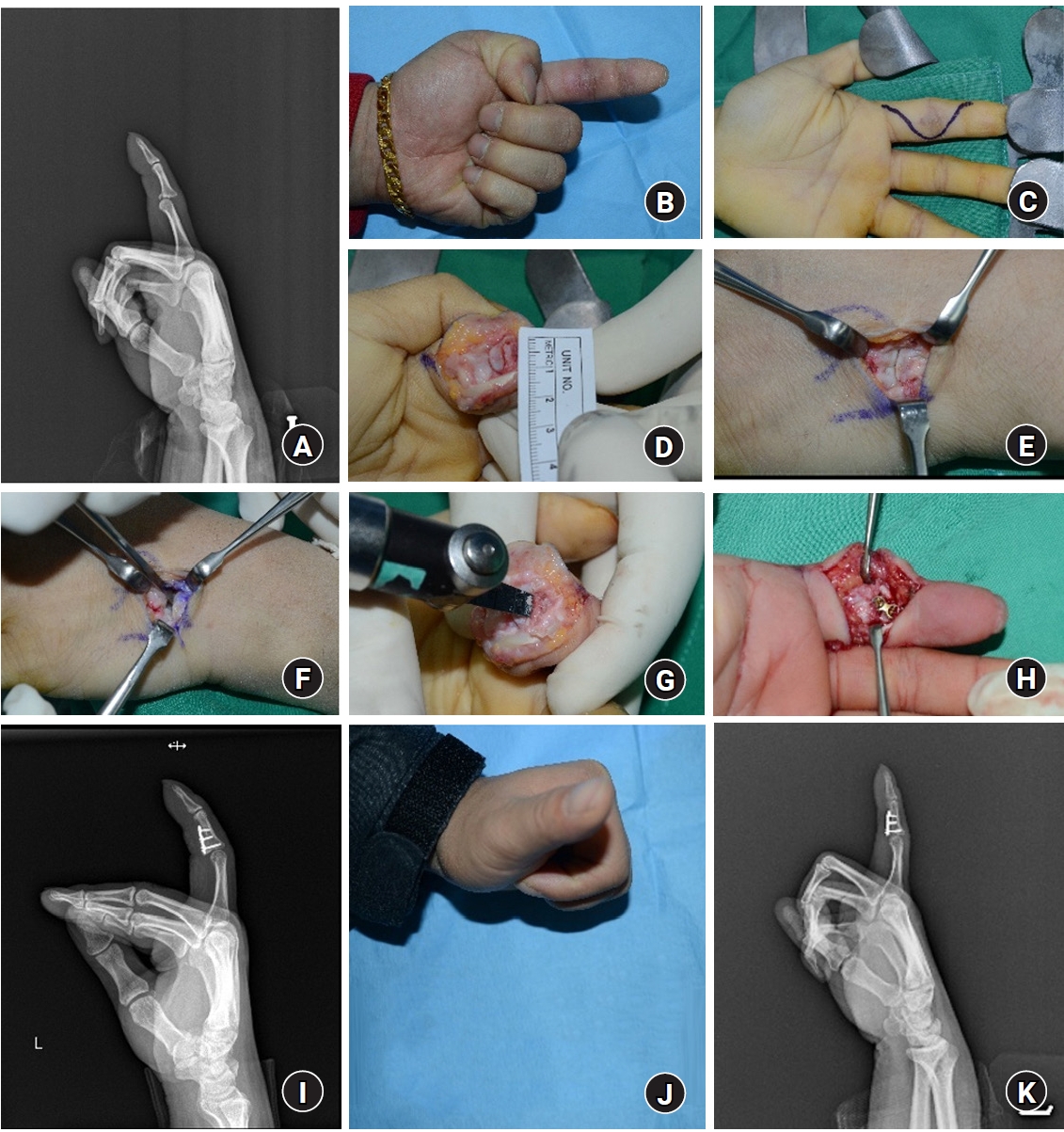
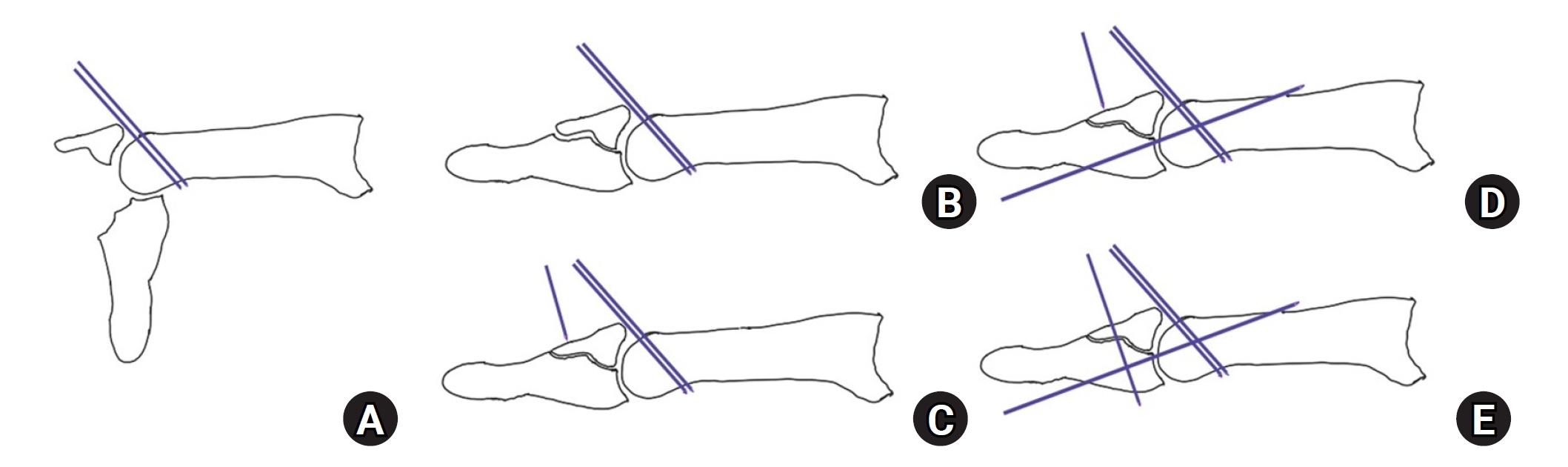
Fig. 1.Modified extension block pinning technique. One or two extension blocking pins are inserted from the dorsal aspect of the proximal phalanx head at around a 45° angle to prevent dorsal fragment displacement (A). Although the distal phalanx segment is extended, the reduction is not perfect (B). With the aid of a dorsal counterforce reduction Kirschner wire (K-wire), an axial transarticular K-wire is inserted from the volar aspect of the distal phalanx (C, D). A dorsal counterforce K-wire is additionally inserted to fix the dorsal fragment in addition to the conventional extension block technique (E).
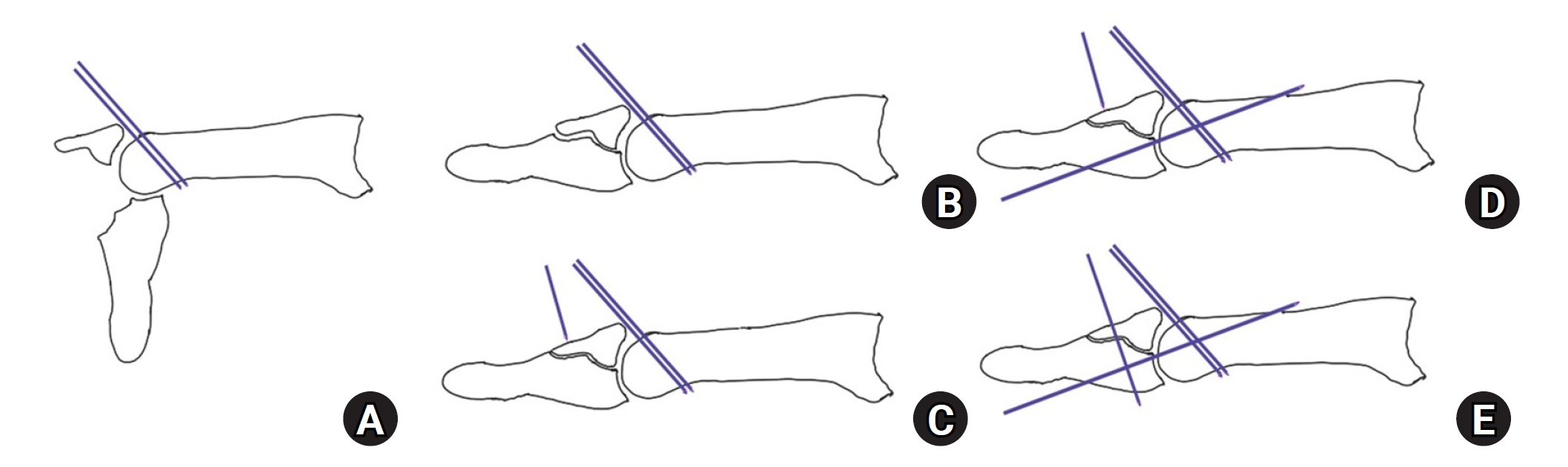
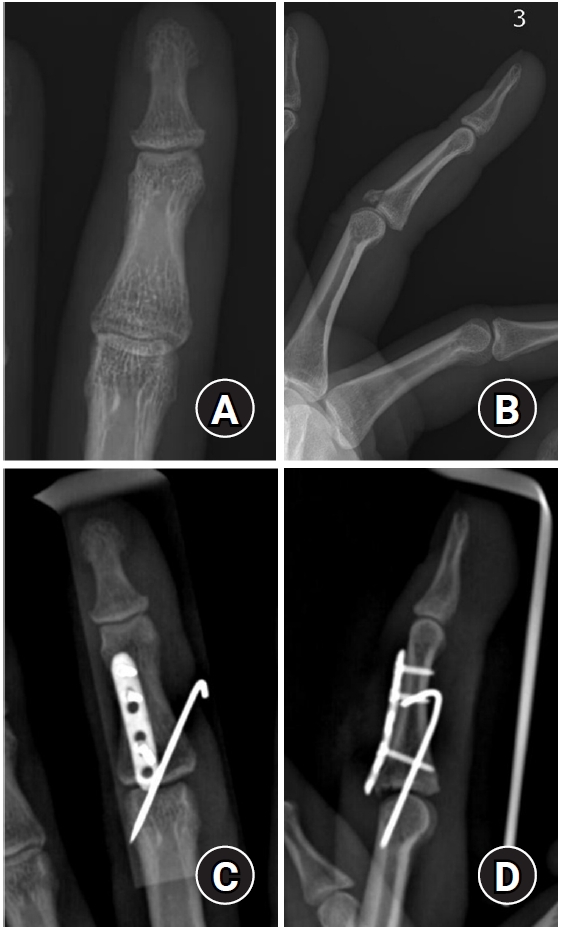
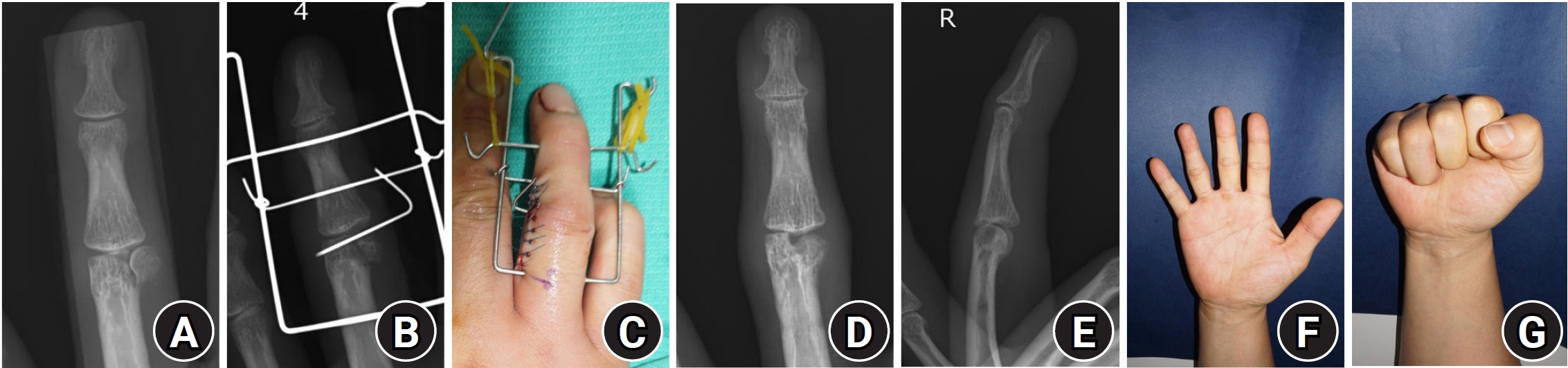
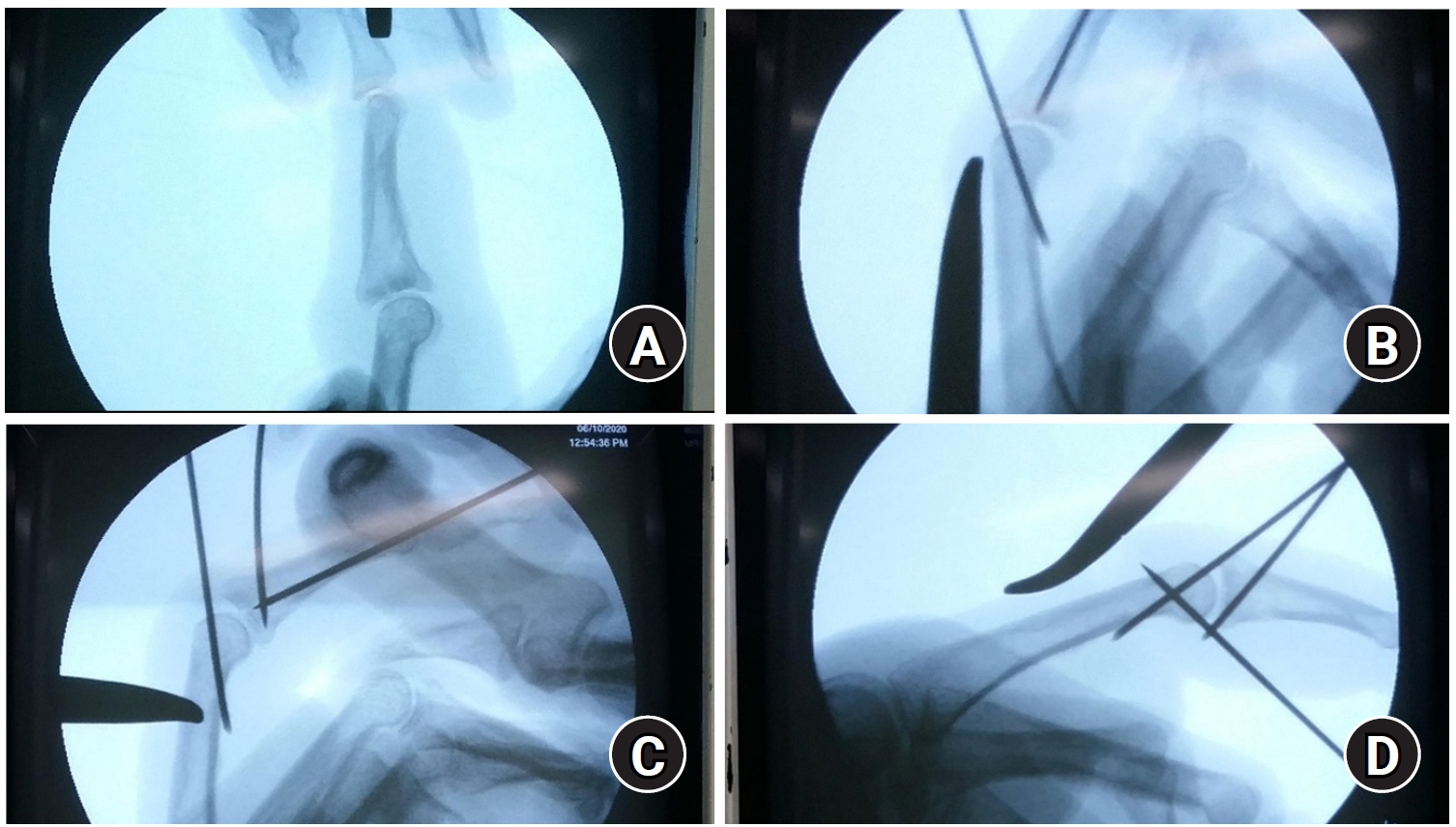
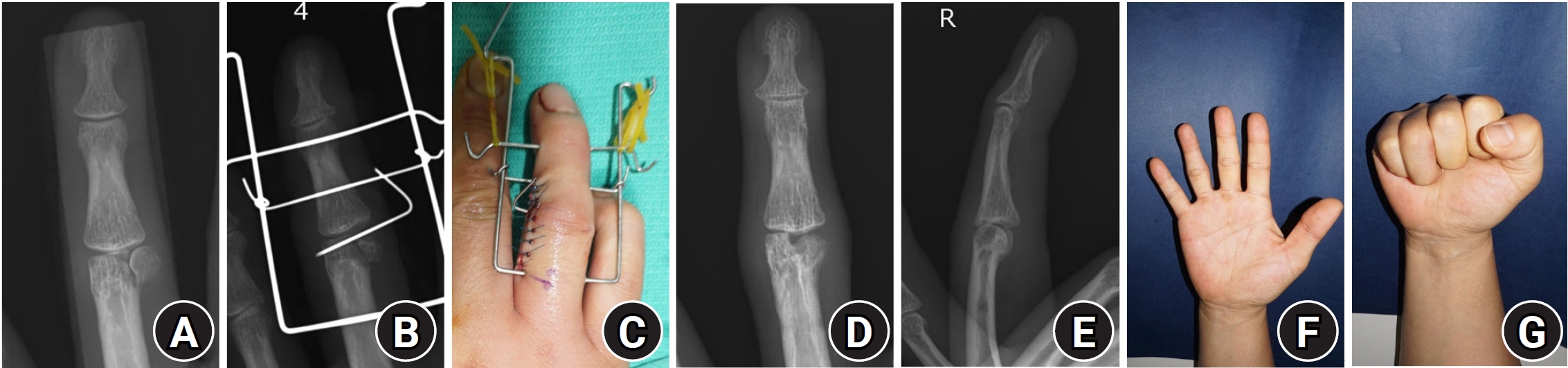
Fig. 2.Distraction dynamic external fixator for displaced condylar fracture of the proximal phalanx. Open reduction was required for a displaced articular fracture involving the condyle of the proximal phalangeal head of the fourth finger (A). Due to the presence of small fracture fragments, the fracture was stabilized using a distraction dynamic external fixator and a temporary Kirschner wire (B, C). Bone union was achieved; however, malunion persisted in the coronal plane (D, E). Despite the malunion, there was no functional impairment of hand movement (F, G).
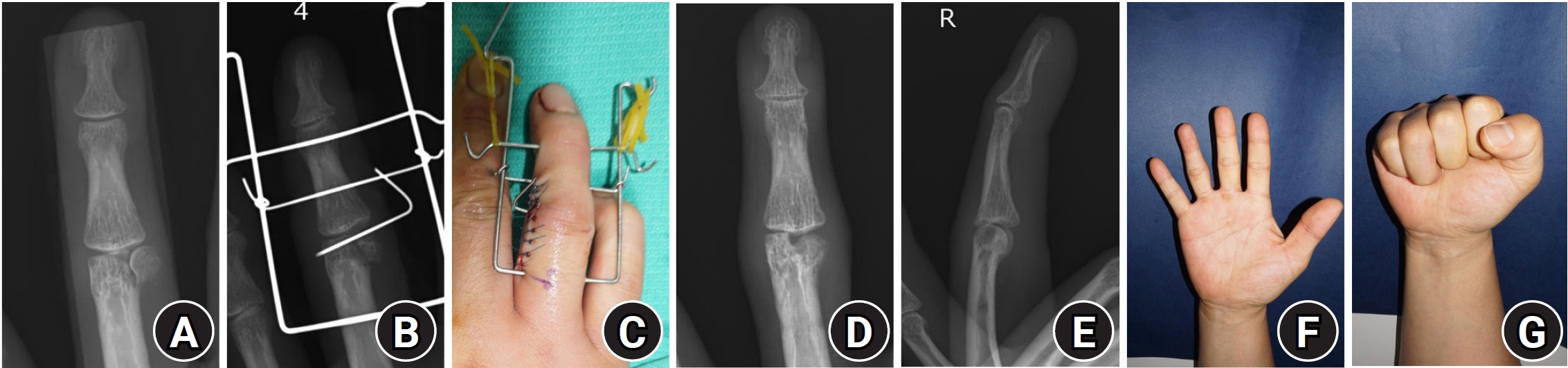
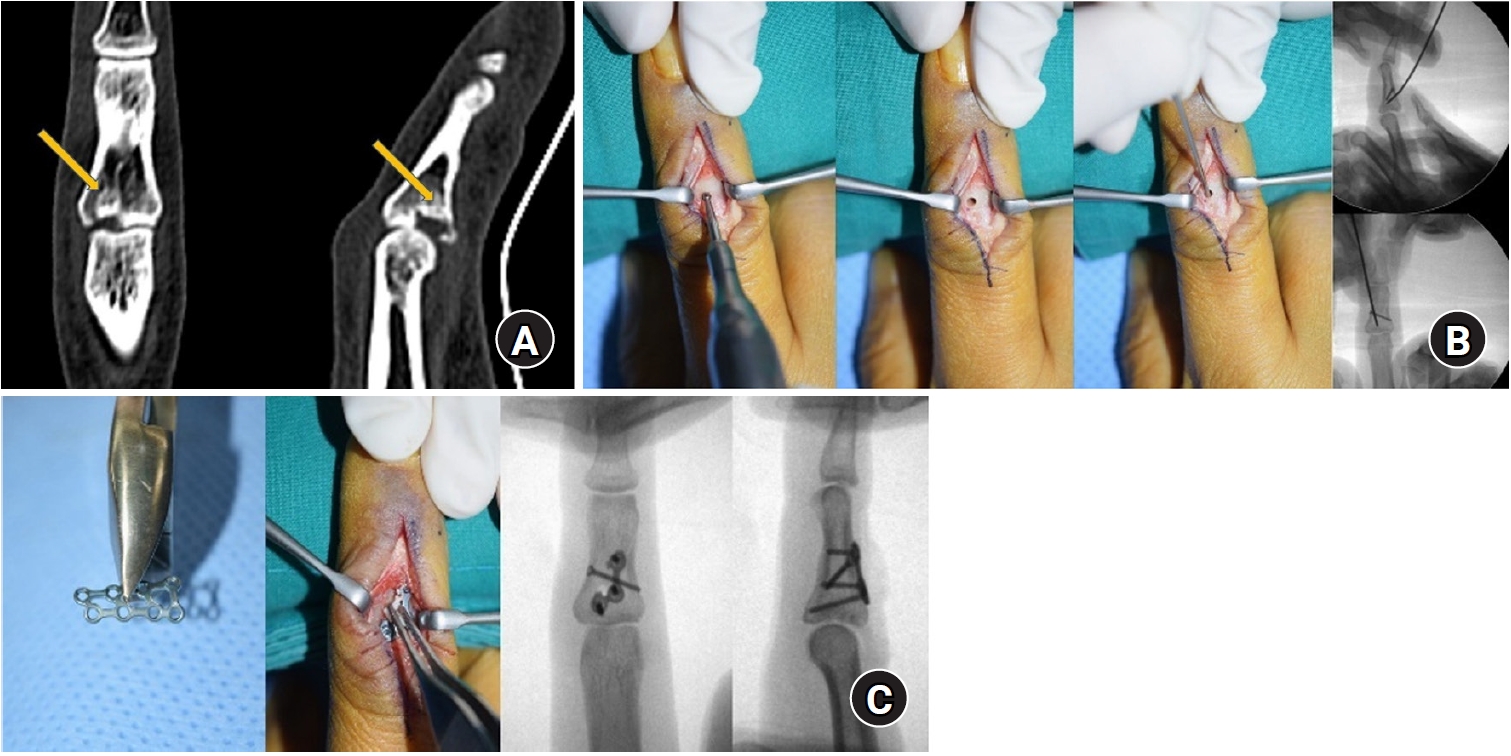
Fig. 3.Proximal phalanx fracture of fourth finger with difference between X-ray findings and physical examination. Fracture of the proximal phalanx base of the fourth finger was shown with minimal displacement on the X-ray (A-C). However, finger overlap due to rotational displacement was observed on physical examination (D).
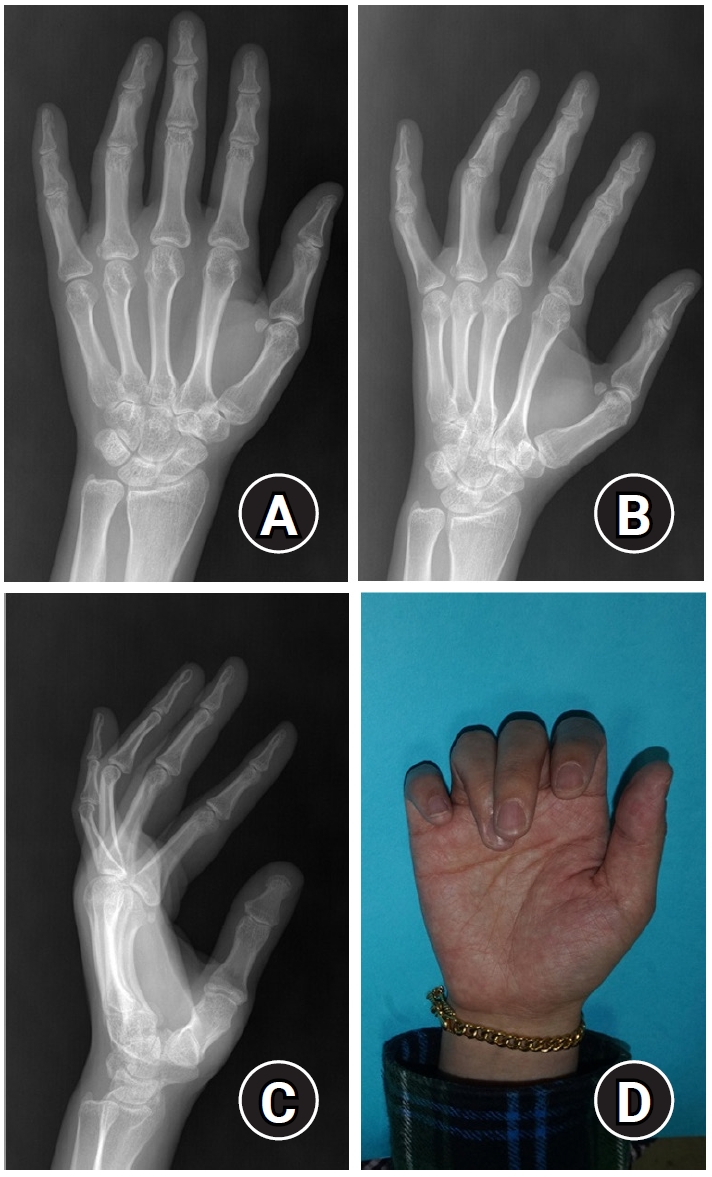
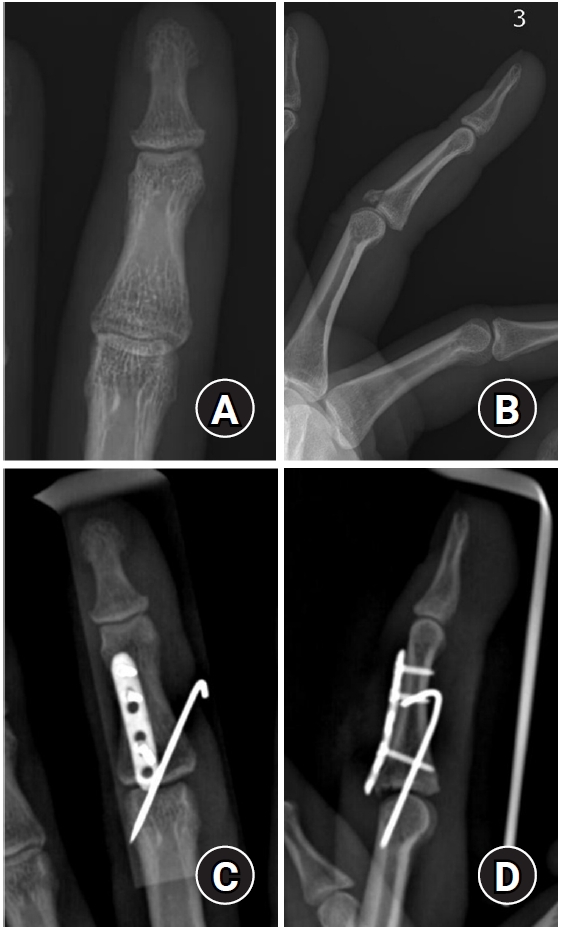
Fig. 4.Fracture of the base of the middle phalanx with dorsal subluxation. Subluxation of the proximal interphalangeal joint was caused by a basal fracture of the left third middle phalanx (A). The articular surface was reduced, and plate fixation was performed through a volar approach (B, C). The fracture surface was successfully reduced, and the subluxation was corrected (D). Case courtesy of SH Han from CHA University, Seongnam, Korea.
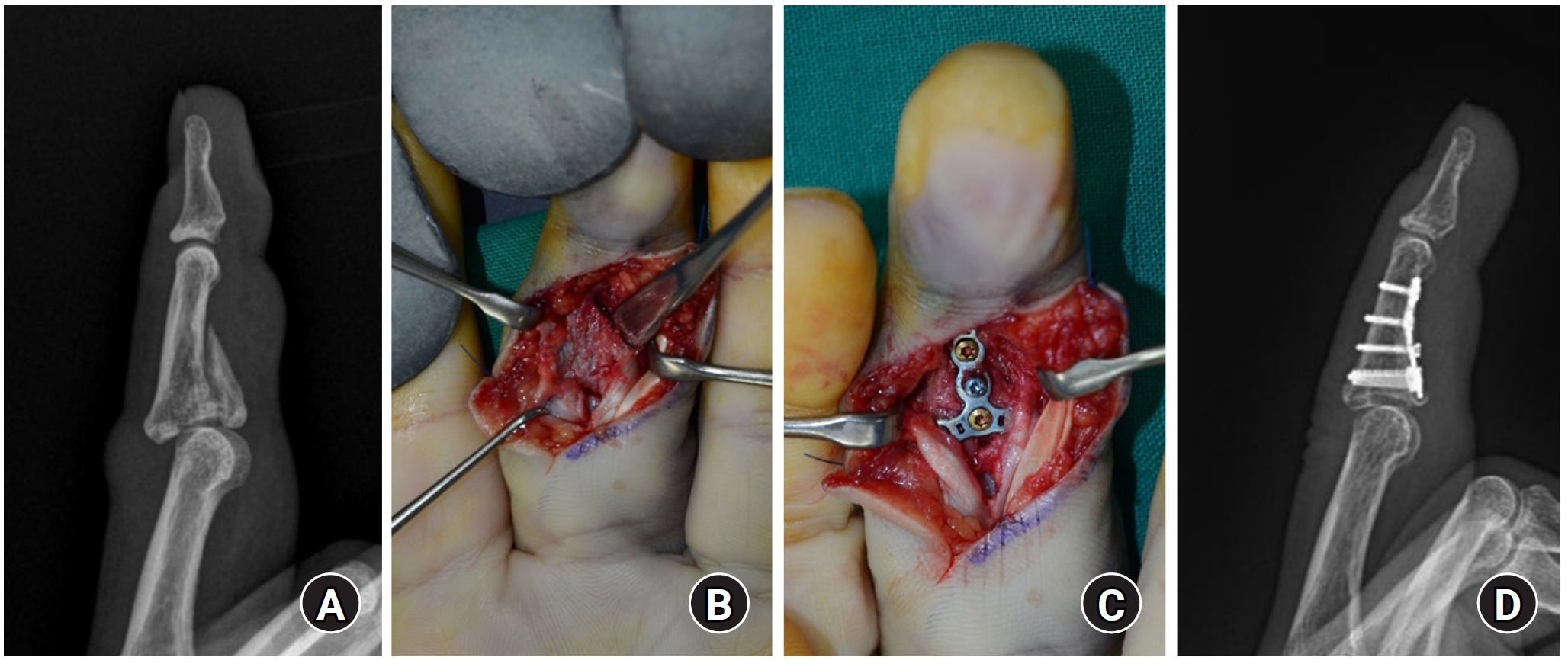
Fig. 5.Hemi-hamate arthroplasty. Lateral plain X-ray presented middle phalanx base volar comminuted fracture and dorsal subluxation of joint (A). The patient complaint limited flexion in preoperative clinic (B). Volar Bruner incision was designed (C) and the fractured site was visualized with shot-gun approach (D). After fracture fragment measurement, dorsal hamate-metacarpal joint is approached for hemi-hamate harvest (E, F). With fractured proximal phalanx base preparation, the harvested hamate bone was grafted and fixed with small sized plate and screws (G, H). Post operatively harvested bone well fixed with implant without joint subluxation (I). On 8 months of post-operation, patient recovered full flexion without arthritic change (J, K). Case courtesy of SH Han from CHA University, Seongnam, Korea.
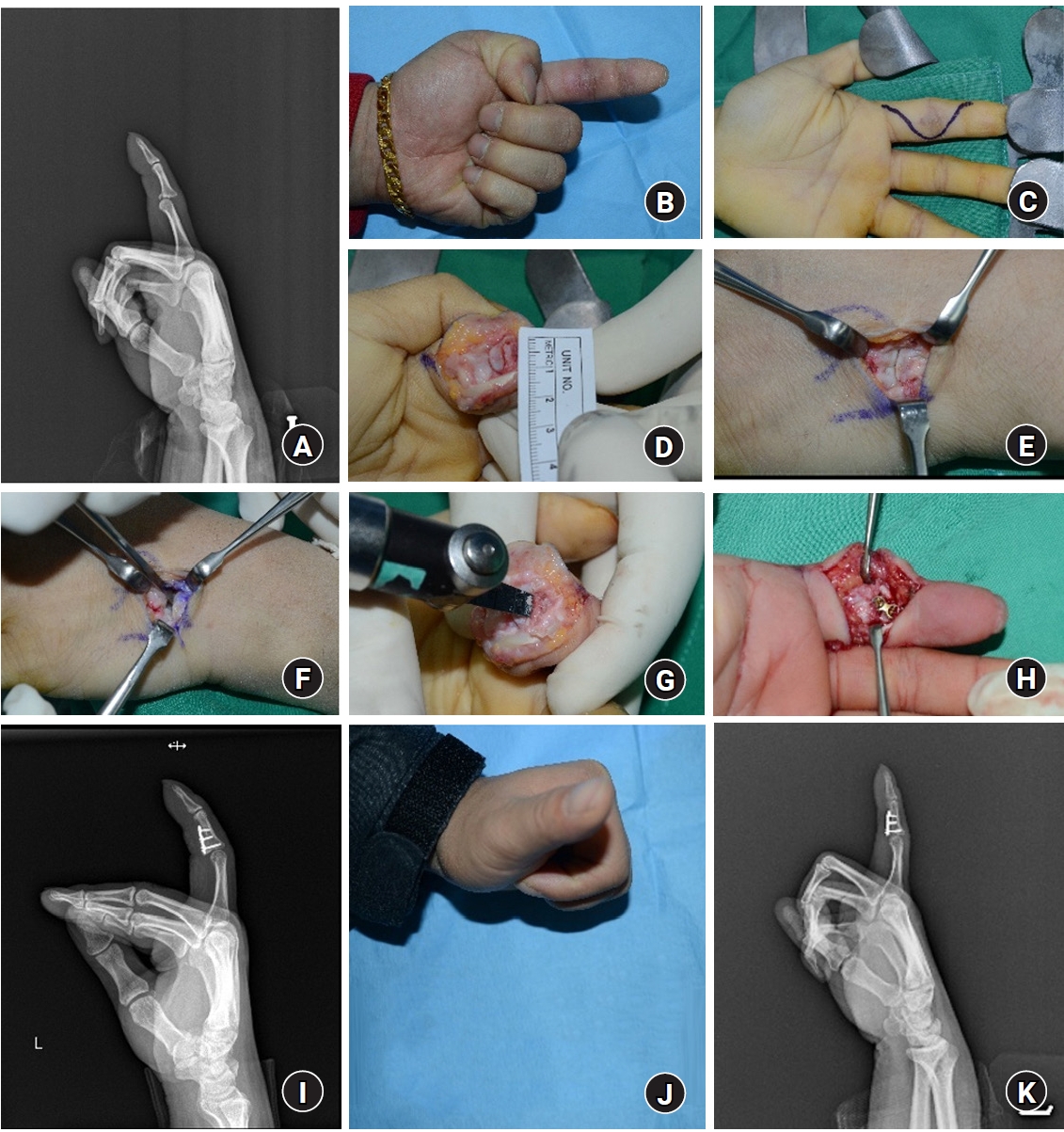
Fig. 6.Closed reduction and K-wire fixation for depressed articular fragment and dorsal subluxation. In lateral C-arm image intensifier, middle phalanx articular fragment depressed and dorsal joint subluxation was identified (A). With extension blocking pin inserted, the depressed joint fragment reduced using intramedullary K-wire by closed method (B). Additional inter-fragment K-wire inserted from dorsal aspect in properly reduced position (C). Finally, additional volar flexion blocking pin was inserted (D).
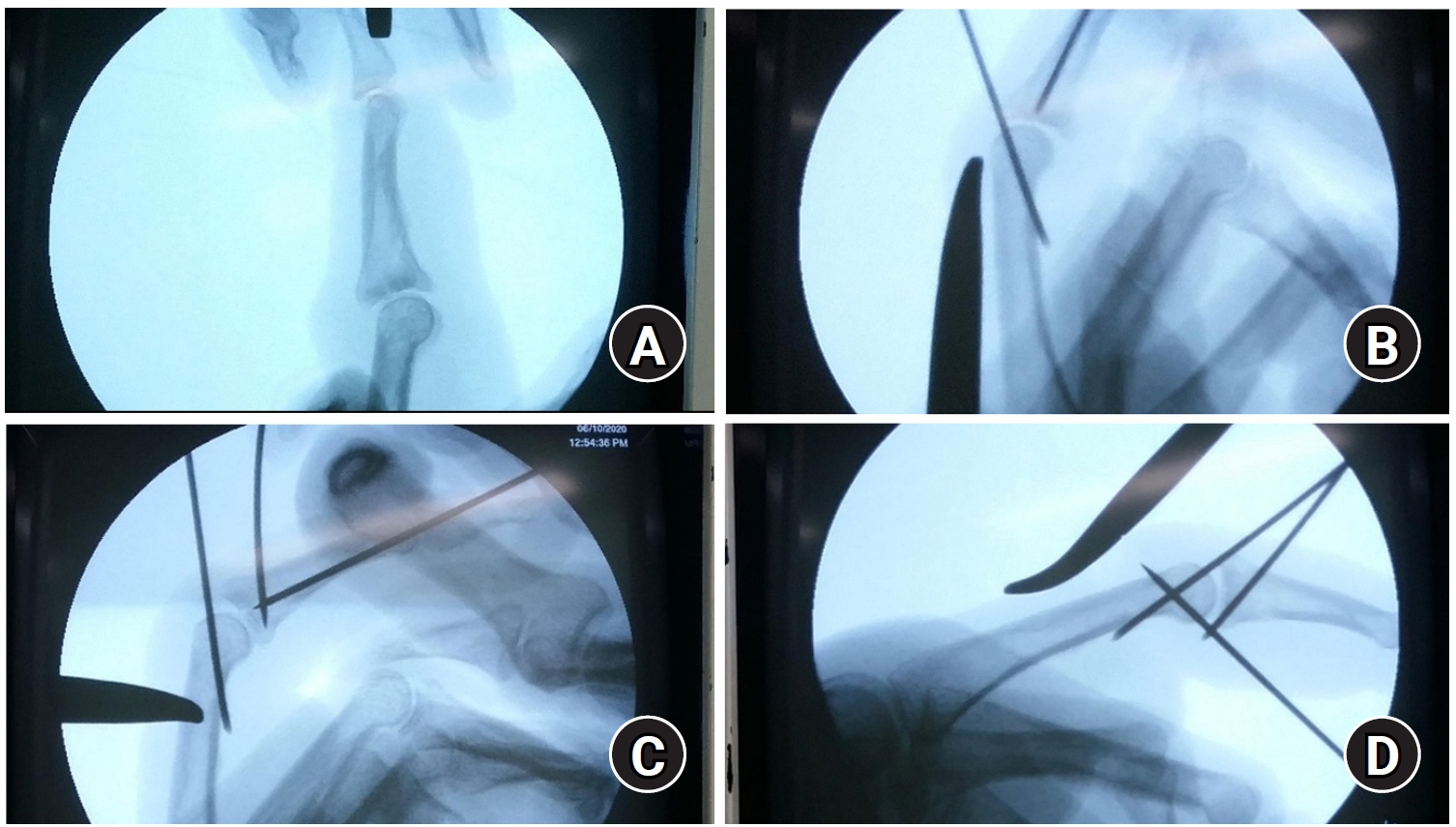
Fig. 7.A representative case of trans-osseous reduction and dorsal locking plate fixation. A preoperative computed tomography scan presented a volar lip fracture with a depressed intra-articular fragment (arrows) (A). Cortical window creation on the dorsal bare area of the middle phalanx, and reduction of the impacted fragment using a Kirschner-wire inserted through the window (B). Locking plate positioning after reduction and insertion of the most proximal screw to buttress the articular fragment (C). Case courtesy of JW Park from Korea University, Seoul, Korea.
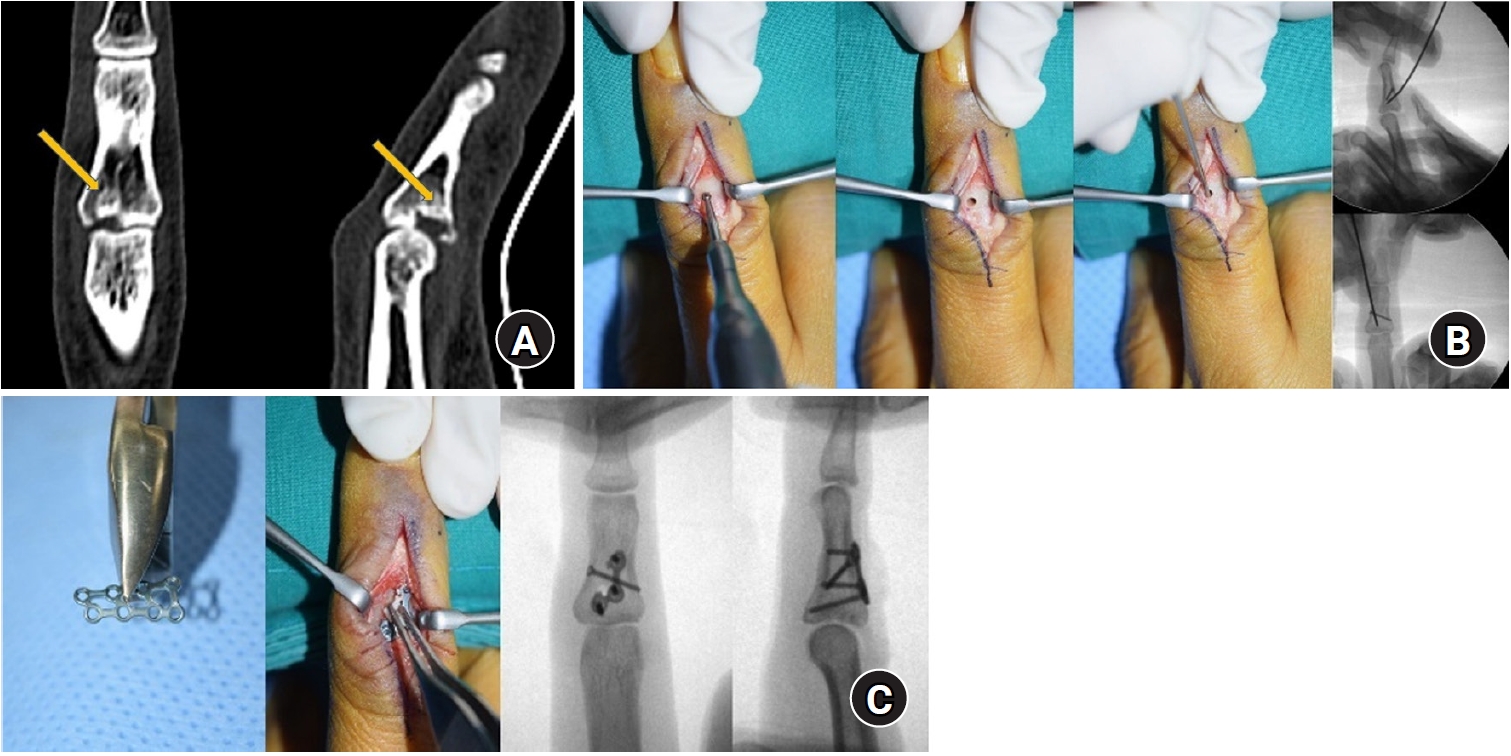
Fig. 8.Middle phalanx base fracture and subluxation. Subluxation of the proximal interphalangeal joint was caused by a fracture of the base of the right third middle phalanx (A, B). Fractures and subluxations were reduced by dorsal plating and temporary K-wire fixation (C, D).
References
- 1. Popova D, Welman T, Vamadeva SV, Pahal GS. Management of hand fractures. Br J Hosp Med (Lond) 2020;81:1-11.ArticlePubMed
- 2. Yoon YC, Baek JR. Current concepts of fractures and dislocation of the hand. J Musculoskelet Trauma 2016;29:143-59.ArticlePDF
- 3. Feehan LM, Sheps SB. Incidence and demographics of hand fractures in British Columbia, Canada: a population-based study. J Hand Surg Am 2006;31:1068-74.ArticlePubMed
- 4. De Jonge JJ, Kingma J, van der Lei B, Klasen HJ. Phalangeal fractures of the hand: an analysis of gender and age-related incidence and aetiology. J Hand Surg Br 1994;19:168-70.ArticlePubMed
- 5. Kremer L, Frank J, Lustenberger T, Marzi I, Sander AL. Epidemiology and treatment of phalangeal fractures: conservative treatment is the predominant therapeutic concept. Eur J Trauma Emerg Surg 2022;48:567-71.ArticlePubMed
- 6. Butt WD. Fractures of the hand: I. description. Can Med Assoc J 1962;86:731-5.PubMedPMC
- 7. Heifner JJ, Rubio F. Fractures of the phalanges. J Hand Surg Eur Vol 2023;48(2_suppl):18S-26S.ArticlePubMedPDF
- 8. Freeland AE, Hardy MA, Singletary S. Rehabilitation for proximal phalangeal fractures. J Hand Ther 2003;16:129-42.ArticlePubMed
- 9. Boeckstyns ME. Current methods, outcomes and challenges for the treatment of hand fractures. J Hand Surg Eur Vol 2020;45:547-59.ArticlePubMedPDF
- 10. Zhang M, Hirth M, Cole T, Hew J, Lim P, Ng S. A systematic review of conservatively managed isolated extra-articular proximal phalanx finger fractures in adults. JPRAS Open 2024;41:37-51.ArticlePubMedPMC
- 11. Neumeister MW, Winters JN, Maduakolum E. Phalangeal and metacarpal fractures of the hand: preventing stiffness. Plast Reconstr Surg Glob Open 2021;9:e3871. ArticlePubMedPMC
- 12. El-Saeed M, Sallam A, Radwan M, Metwally A. Kirschner wires versus titanium plates and screws in management of unstable phalangeal fractures: a randomized, controlled clinical trial. J Hand Surg Am 2019;44:1091e1-9.ArticlePubMed
- 13. Schneider LH. Fractures of the distal phalanx. Hand Clin 1988;4:537-47.ArticlePubMed
- 14. Liodaki E, Xing SG, Mailaender P, Stang F. Management of difficult intra-articular fractures or fracture dislocations of the proximal interphalangeal joint. J Hand Surg Eur Vol 2015;40:16-23.ArticlePubMedPDF
- 15. Kim J, Ki SH, Cho Y. Correction of distal phalangeal nonunion using peg bone graft. J Hand Surg Am 2014;39:249-55.ArticlePubMed
- 16. Liao JC, Das De S. Management of tendon and bony injuries of the distal phalanx. Hand Clin 2021;37:27-42.ArticlePubMed
- 17. Simon RR, Wolgin M. Subungual hematoma: association with occult laceration requiring repair. Am J Emerg Med 1987;5:302-4.ArticlePubMed
- 18. Gellman H. Fingertip-nail bed injuries in children: current concepts and controversies of treatment. J Craniofac Surg 2009;20:1033-5.ArticlePubMed
- 19. Fehrenbacher V, Blackburn E. Nail bed injury. J Hand Surg Am 2015;40:581-2.ArticlePubMed
- 20. Ganesh Kumar N, Chung KC. An evidence-based guide for managing phalangeal fractures. Plast Reconstr Surg 2021;147:846e-861e.ArticlePubMed
- 21. Tuttle HG, Olvey SP, Stern PJ. Tendon avulsion injuries of the distal phalanx. Clin Orthop Relat Res 2006;445:157-68.ArticlePubMed
- 22. Husain SN, Dietz JF, Kalainov DM, Lautenschlager EP. A biomechanical study of distal interphalangeal joint subluxation after mallet fracture injury. J Hand Surg Am 2008;33:26-30.ArticlePubMed
- 23. Okafor B, Mbubaegbu C, Munshi I, Williams DJ. Mallet deformity of the finger. Five-year follow-up of conservative treatment. J Bone Joint Surg Br 1997;79:544-7.ArticlePubMed
- 24. Handoll HH, Vaghela MV. Interventions for treating mallet finger injuries. Cochrane Database Syst Rev 2004;(3):CD004574.Article
- 25. Niechajev IA. Conservative and operative treatment of mallet finger. Plast Reconstr Surg 1985;76:580-5.ArticlePubMed
- 26. Ishiguro T, Inoue K, Matsubayashi T, Ito T, Hashizume N. A new method of closed reduction for mallet fractures. J Jpn Soc Surg Hand 1988;5:444-7.
- 27. Lee YH, Kim JY, Chung MS, Baek GH, Gong HS, Lee SK. Two extension block Kirschner wire technique for mallet finger fractures. J Bone Joint Surg Br 2009;91:1478-81.ArticlePubMedPDF
- 28. Lee SK, Kim KJ, Yang DS, Moon KH, Choy WS. Modified extension-block K-wire fixation technique for the treatment of bony mallet finger. Orthopedics 2010;33:728.ArticlePubMed
- 29. Yamanaka K, Sasaki T. Treatment of mallet fractures using compression fixation pins. J Hand Surg Br 1999;24:358-60.ArticlePubMedPDF
- 30. Lee SH, Lee JE, Lee KH, Pyo SH, Kim MB, Lee YH. Supplemental method for reduction of irreducible mallet finger fractures by the 2-extension block technique: the dorsal counterforce technique. J Hand Surg Am 2019;44:695.ArticlePubMed
- 31. Lamaris GA, Matthew MK. The diagnosis and management of mallet finger injuries. Hand (N Y) 2017;12:223-8.ArticlePubMedPDF
- 32. Chang WH, Thomas OJ, White WL. Avulsion injury of the long flexor tendons. Plast Reconstr Surg 1972;50:260-4.ArticlePubMed
- 33. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am 1977;2:66-9.ArticlePubMed
- 34. Smith JH Jr. Avulsion of a profundus tendon with simultaneous intraarticular fracture of the distal phalanx: case report. J Hand Surg Am 1981;6:600-1.ArticlePubMed
- 35. Halat G, Negrin L, Erhart J, Ristl R, Hajdu S, Platzer P. Treatment options and outcome after bony avulsion of the flexor digitorum profundus tendon: a review of 29 cases. Arch Orthop Trauma Surg 2017;137:285-92.ArticlePubMedPDF
- 36. Kong AC, Kitto A, Pineda DE, Miki RA, Alfonso DT, Alfonso I. Four anchor repair of jersey finger. Iowa Orthop J 2021;41:95-100.
- 37. Huq S, George S, Boyce DE. Zone 1 flexor tendon injuries: a review of the current treatment options for acute injuries. J Plast Reconstr Aesthet Surg 2013;66:1023-31.ArticlePubMed
- 38. McCallister WV, Ambrose HC, Katolik LI, Trumble TE. Comparison of pullout button versus suture anchor for zone I flexor tendon repair. J Hand Surg Am 2006;31:246-51.ArticlePubMed
- 39. Stamos BD, Leddy JP. Closed flexor tendon disruption in athletes. Hand Clin 2000;16:359-65.ArticlePubMed
- 40. London PS. Sprains and fractures involving the interphalangeal joints. Hand 1971;3:155-8.ArticlePubMedPDF
- 41. Gaston RG, Chadderdon C. Phalangeal fractures: displaced/nondisplaced. Hand Clin 2012;28:395-401.ArticlePubMed
- 42. Singh J, Jain K, Ravishankar R. Outcome of closed proximal phalangeal fractures of the hand. Indian J Orthop 2011;45:432-8.ArticlePubMedPMCPDF
- 43. Caggiano NM, Harper CM, Rozental TD. Management of proximal interphalangeal joint fracture dislocations. Hand Clin 2018;34:149-65.ArticlePubMed
- 44. Leibovic SJ, Bowers WH. Anatomy of the proximal interphalangeal joint. Hand Clin 1994;10:169-78.ArticlePubMed
- 45. Barksfield RC, Bowden B, Chojnowski AJ. Hemi-hamate arthroplasty versus transarticular Kirschner wire fixation for unstable dorsal fracture-dislocation of the proximal interphalangeal joint in the hand. Hand Surg 2015;20:115-9.ArticlePubMed
- 46. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am 2010;35:2046-52.ArticlePubMed
- 47. Lee JK, Kim YS, Lee JH, Jang GC, Han SH. Open reduction and internal fixation for dorsal fracture-dislocation of the proximal interphalangeal joint. Handchir Mikrochir Plast Chir 2020;52:18-24.ArticlePubMed
- 48. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am 2008;33:19-25.ArticlePubMed
- 49. Lee LS, Lee HM, Hou YT, Hung ST, Chen JK, Shih JT. Surgical outcome of volar plate arthroplasty of the proximal interphalangeal joint using the Mitek micro GII suture anchor. J Trauma 2008;65:116-22.ArticlePubMed
- 50. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am 2003;28:856-65.ArticlePubMed
- 51. Buckwalter JA. Activity vs. rest in the treatment of bone, soft tissue and joint injuries. Iowa Orthop J 1995;15:29-42.PubMedPMC
- 52. Finsen V. Suzuki's pins and rubber traction for fractures of the base of the middle phalanx. J Plast Surg Hand Surg 2010;44:209-13.ArticlePubMed
- 53. Park JH, Park GW, Choi IC, Kwon YW, Park JW. Dorsal transosseous reduction and locking plate fixation for articular depressed middle phalangeal base fracture. Arch Orthop Trauma Surg 2019;139:141-5.ArticlePubMedPDF
- 54. Hsu LP, Schwartz EG, Kalainov DM, Chen F, Makowiec RL. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am 2011;36:610-6.ArticlePubMed
- 55. von Kieseritzky J, Nordstrom J, Arner M. Reoperations and postoperative complications after osteosynthesis of phalangeal fractures: a retrospective cohort study. J Plast Surg Hand Surg 2017;51:458-62.ArticlePubMed
- 56. Wellborn PK, Allen AD, Draeger RW. Current outcomes and treatments of complex phalangeal and metacarpal fractures. Hand Clin 2023;39:251-63.ArticlePubMed
- 57. Waris E, Ashammakhi N, Happonen H, et al. Bioabsorbable miniplating versus metallic fixation for metacarpal fractures. Clin Orthop Relat Res 2003;(410):310-9.ArticlePubMed
- 58. Horton TC, Hatton M, Davis TR. A prospective randomized controlled study of fixation of long oblique and spiral shaft fractures of the proximal phalanx: closed reduction and percutaneous Kirschner wiring versus open reduction and lag screw fixation. J Hand Surg Br 2003;28:5-9.ArticlePubMedPDF
- 59. Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am 2010;35:1260-3.ArticlePubMed
- 60. Sivakumar BS, An VV, Graham DJ, Ledgard J, Lawson RD, Furniss D. Intramedullary compression screw fixation of proximal phalangeal fractures: a systematic literature review. Hand (N Y) 2022;17:595-601.ArticlePubMedPMCPDF
- 61. Itadera E, Yamazaki T. Trans-metacarpal screw fixation for extra-articular proximal phalangeal base fractures. J Hand Surg Asian Pac Vol 2017;22:35-8.ArticlePubMed
- 62. del Pinal F, Moraleda E, Ruas JS, de Piero GH, Cerezal L. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am 2015;40:692-700.ArticlePubMed
- 63. Casal O, Vegas M, Estefania Diez M, Cano P, Maya Gonzalez J, Nevado E. Percutaneous osteosynthesis with headless cannulated screws in the treatment of metacarpal and proximal and middle phalanxes fractures of the hand. Rev Iberoam Cir Mano 2018;46:117-25.Article
- 64. Jovanovic N, Aldlyami E, Saraj B, et al. Intramedullary percutaneous fixation of extra-articular proximal and middle phalanx fractures. Tech Hand Up Extrem Surg 2018;22:51-6.ArticlePubMed
- 65. Gaspar MP, Gandhi SD, Culp RW, Kane PM. Dual antegrade intramedullary headless screw fixation for treatment of unstable proximal phalanx fractures. Hand (N Y) 2019;14:494-9.ArticlePubMedPMCPDF
- 66. Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am 2013;38:2025-8.ArticlePubMed
- 67. Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am 2005;30:1061-7.ArticlePubMed
- 68. Onishi T, Omokawa S, Shimizu T, Fujitani R, Shigematsu K, Tanaka Y. Predictors of postoperative finger stiffness in unstable proximal phalangeal fractures. Plast Reconstr Surg Glob Open 2015;3:e431. ArticlePubMedPMC
- 69. Wang ED, Rahgozar P. The pathogenesis and treatment of the stiff finger. Clin Plast Surg 2019;46:339-45.ArticlePubMed
- 70. Day CS. Fractures of the metacarpals and phalanges. In: Green DP, Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green's operative hand surgery. Elsevier Churchill Livingstone; 2017. p. 231-77.
- 71. Henry MH. Hand fractures and dislocations. In: Rockwood CA, Green DP, Bucholz RW, editors. Rockwood and Green's fractures in adults. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. p. 711-80.
- 72. Jupiter JB, Axelrod TS, Belsky MR. Fractures and dislocations for the hand. In: Browner BD, editor. Skeletal trauma: basic science, management, and reconstruction. 3rd. Saunders; 2003. p. 1153-267.
- 73. Ashkenaze DM, Ruby LK. Metacarpal fractures and dislocations. Orthop Clin North Am 1992;23:19-33.ArticlePubMed
- 74. Ring D. Malunion and nonunion of the metacarpals and phalanges. Instr Course Lect 2006;55:121-8.ArticlePubMed
 , Jun-Ku Lee, MD1,2
, Jun-Ku Lee, MD1,2


 E-submission
E-submission KOTA
KOTA
 ePub Link
ePub Link Cite
Cite

