Abstract
-
Background
The purpose of this study was to investigate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures.
-
Methods
Between 2007 and 2020, 17 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion combined with bone defect were investigated. The mean age was 53 years (range, 22‒70 years). The mean follow-up period was 102.2 months (range, 18‒193 months). Serial plain radiographs were used to evaluate radiological outcomes. The University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate clinical outcomes. Complications were also evaluated.
-
Results
All cases achieved complete bony union with mean healing time of 17.6 weeks (range, 14‒22 weeks). The mean clavicle length difference was significantly decreased from 9.1 mm preoperatively to 2.6 mm postoperatively (P<0.001). The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001), respectively. The mean final Quick-DASH score was 18.0. Three cases (17.6%) developed postoperative complications including two cases of shoulder stiffness and one case of screw irritation.
-
Conclusions
Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length.
-
Level of Evidence
Level IV, case series
-
Keywords: Clavicle, Bone fractures, Midshaft, Nonunion, Bone transplantation
Introduction
Clavicle midshaft fractures are common injuries which account for 2%–10% of adult fractures and more than 70% of all clavicle fractures [
1-
3]. Although conservative or surgical treatments for these fractures produce satisfactory radiological and clinical outcomes, nonunion after the treatment has been reported to be between 0.1%–15% [
1,
4,
5]. A systematic review described that overall incidence of clavicle nonunion is approximately 5.9% [
5,
6]. However, the incidence may be as high as 15% for some fracture subtypes [
5,
6].
Due to pain and functional disability, symptomatic clavicle midshaft nonunion may require surgical intervention. Recent studies have reported that clavicle shortening may lead to disturbances in scapular and glenohumeral kinematics as well as cosmetic deformity [
1,
6-
8].
The primary goal of surgical intervention for clavicle midshaft nonunion is to make an alignment and environment conducive to bony union with restoration of clavicle length [
6]. Various operative techniques for the treatment of the clavicle midshaft nonunion have been reported, including plate fixation, intramedullary fixation, external fixation, lag screw fixation, bone grafting, or combinations thereof [
1,
9]. Although there is no prospective comparative study for these treatment options due to the rarity, most surgeons have agreed that open reduction and plate fixation with bone graft is the gold standard technique for the treatment of clavicle midshaft nonunion [
10]. Various reconstructive and grafting techniques have been described, but there is some controversy regarding the necessity, type, and technique of bone graft for the treatment of the clavicle midshaft nonunion [
1].
In cases of persistent atrophic nonunion, autogenous bone graft is considered the best option due to its osteogenic, osteoconductive, and osteoinductive properties [
10]. Several grafting techniques have been introduced, such as cancellous bone graft, strut bone graft, intercalary bone graft, and vascularized bone graft [
1,
6,
8-
12]. Zhang et al. [
9] reported high rate of bone union after plate fixation and autogenous cancellous bone graft with satisfactory clinical outcomes for atrophic clavicle nonunions. In cases with atrophic fracture ends or bone defect, cortical bone graft may be necessary for restoration of clavicle length [
8]. Several studies have advocated that restoration of clavicle length compared with the contralateral side is important for clinical outcomes after surgery [
6-
8]. Therefore, structural bone graft using autogenous iliac bone is effective solution for atrophic clavicle nonunion combined with bone defect [
7,
8,
10-
14]. However, there has been little study on descriptive surgical details for interpositional bone graft with plate fixation and its efficacy for restoration of clavicle length.
The purpose of this study was to evaluate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures. This study was conducted to identify whether this technique would promote effective bone healing and restore clavicle length.
Methods
Ethics Statement
The study was approved by the Institutional Review Board of Keimyung University Dongsan Hospital (IRB No. 202405046) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient Selection
We retrospectively reviewed 18 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for clavicle midshaft nonunion combined with bone defect in Keimyung University Dongsan Hospital between 2007 and 2020. The inclusion criteria were patients with (1) symptomatic atrophic nonunion caused by failure of union after conservative or operative treatments; (2) bone defect >10 mm after resection of both sclerotic margins. The exclusion criteria were patients with (1) hypertrophic or oligotrophic nonunion; (2) pathologic nonunion; or (3) follow-up period ≤12 months after index surgery. One patient was excluded due to lack of follow-up evaluation. The remaining 17 patients were included in this study.
Patient’s demographic data was listed in (
Table 1). The mean age of the patients at the time of index surgery was 53 years (range, 22–70 years). There were 14 males and three females. Nine patients underwent index surgery on left side. The injury mechanism at the time of initial fracture were traffic accidents in nine cases and slip down in eight cases, and the mean interval from initial treatment after fracture to index surgery was 14.3 months (range, 5–60 months).
For the initial fracture, there were five cases of conservative treatment. Twelve cases were transferred to our clinic after surgical treatment at another hospital. All cases demonstrated atrophic nonunion. The causes of nonunion were categorized as follows: five cases of failed conservative treatment, nine cases of fixation failure, and three cases of fracture-related infection. All surgical procedures were performed by a single surgeon (CHC) at a single institution. The mean follow-up period after index surgery was 102.2 months (range, 18–193 months).
Operative Technique
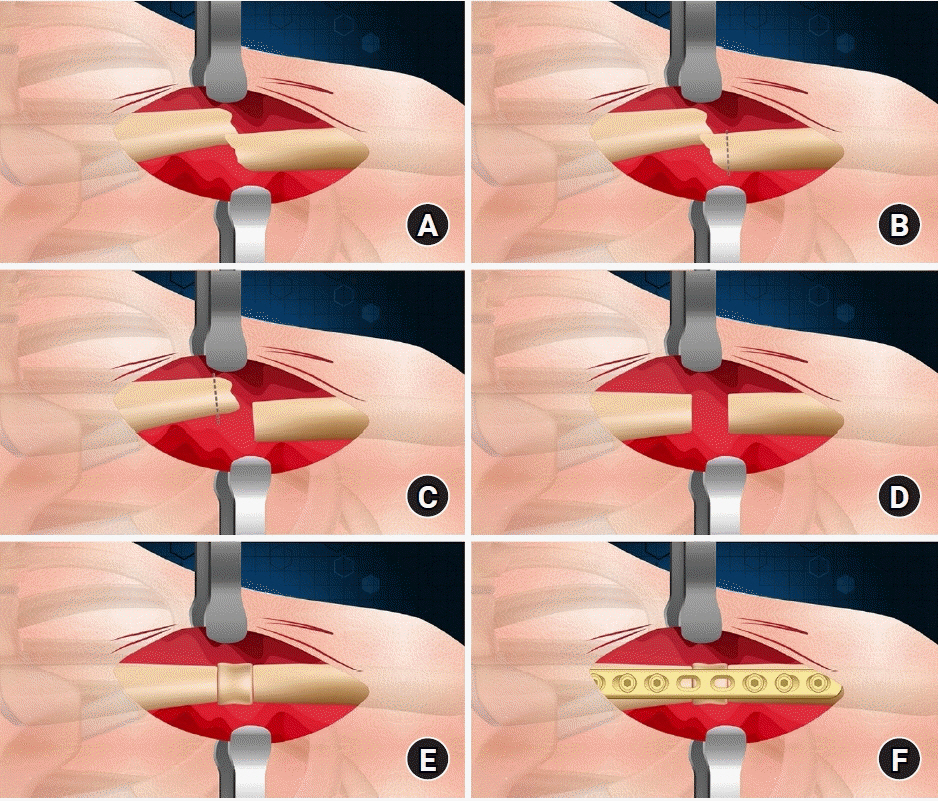
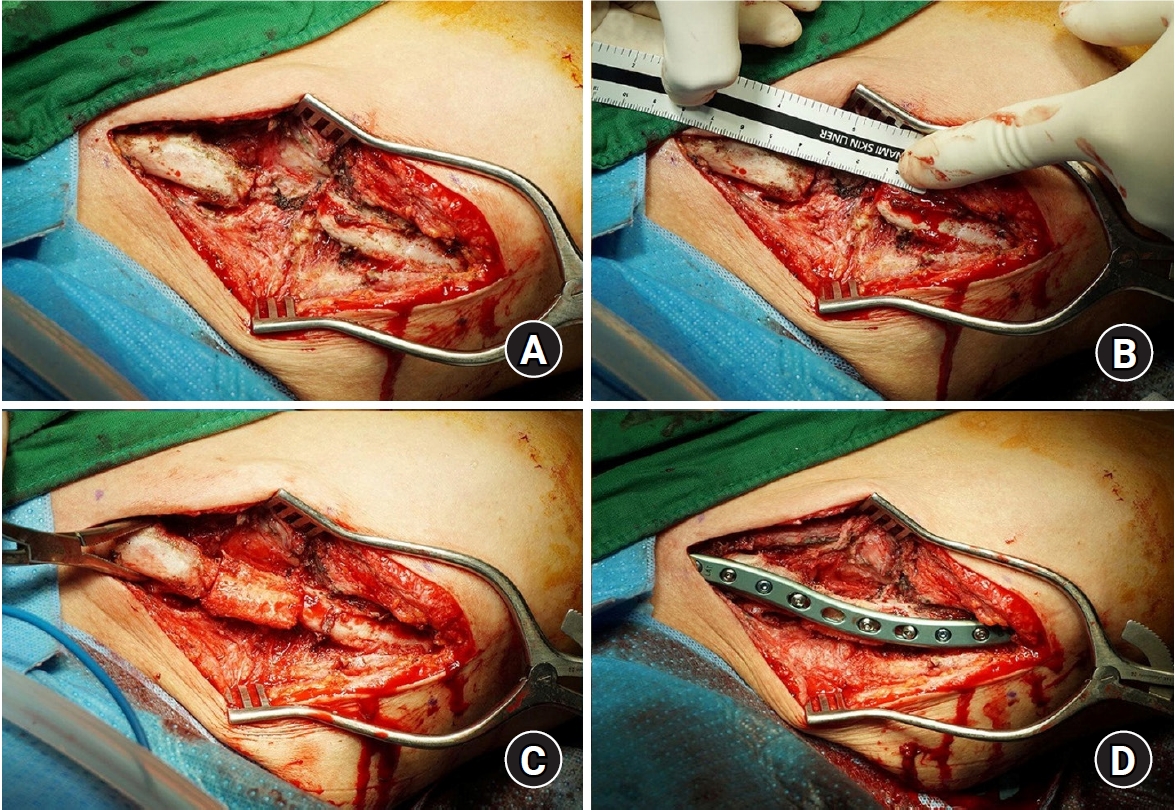
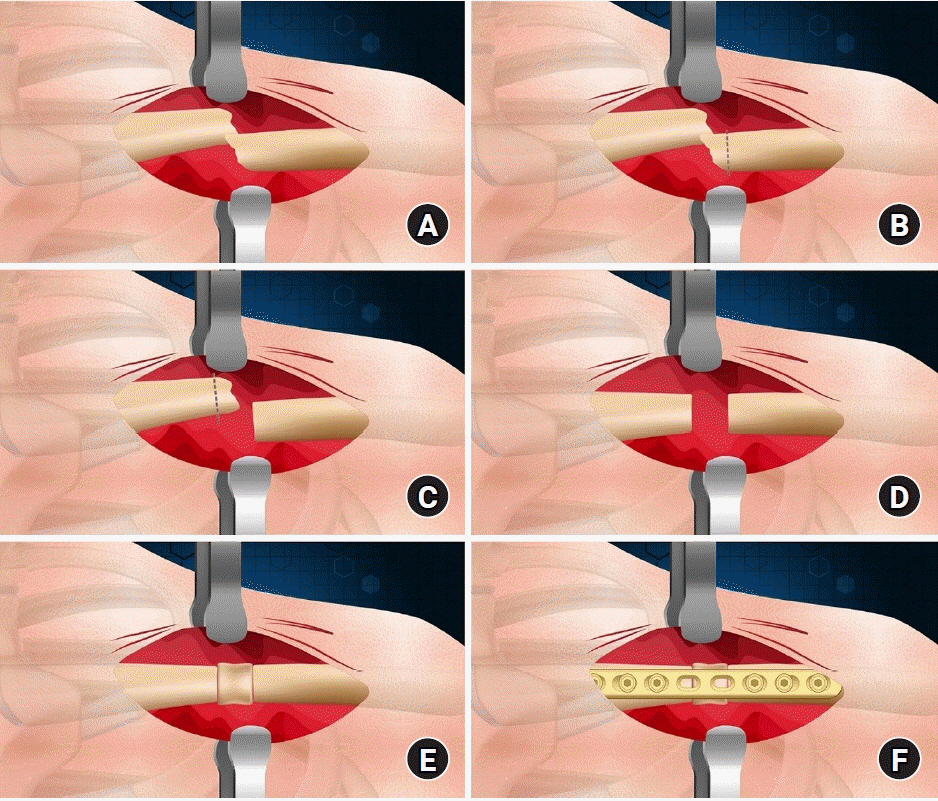
With the patient in the supine position, a skin incision was made along the longitudinal axis of the center of the fracture site or according to the previous surgical scar. The nonunion site was sufficiently exposed, and the surrounding fibrous tissues were removed. Sclerotic bone was then completely resected until a healthy bone is produced with bleeding. Length of the defect area was measured using a ruler after trimming both margins perpendicular to the longitudinal axis of the clavicle. Depending on the measured length of the bone defect, a tricortical iliac bone block was taken using an oscillating saw. Cancellous bone was also harvested. To obtain structural support, the tricortical iliac bone block was interposed between both fragments, followed by plate fixation. The plate with sufficient length was selected and at least three screws were inserted on each side of the proximal and distal fragments to provide sufficient fixation.
Dynamic compression screw technique was used to increase contact surface between the host bone and the graft bone on each side (
Fig. 1). If the interposed iliac bone block is long, it was fixed with a screw through the hole of the plate. In six cases, a 3.5-mm reconstruction locking compression plate (Synthes) was used and an anatomical pre-contoured clavicle plate (Acumed) was used in the other 11 cases. Wearing the arm sling for 4 weeks after index surgery, active and passive shoulder motions were begun once the pain was tolerable.
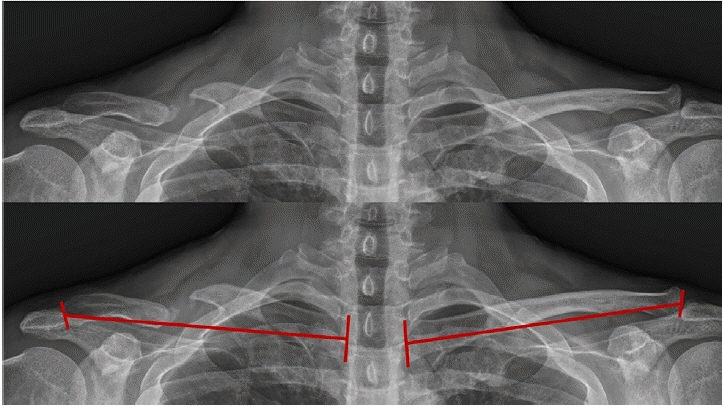
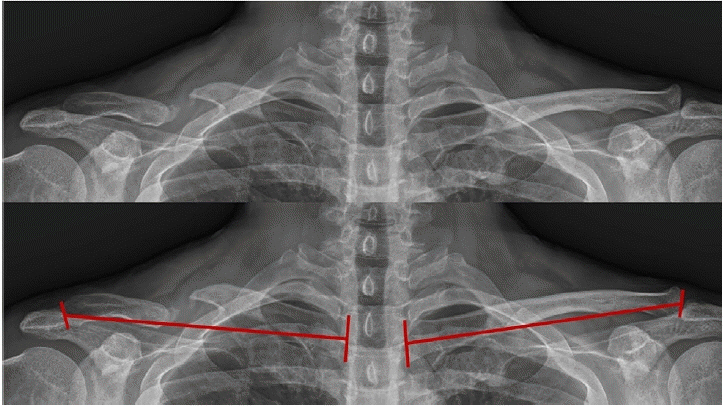
Radiological outcomes were assessed by serial plain radiographs to confirm bone union and clavicle length difference (CLD) after index surgery. Bony union was defined as a completely bridging bone in both anterosuperior and oblique views of clavicle. Using both anteroposterior clavicle plain radiograph, total length of the clavicle was measured bilaterally and defined as the linear distance between the midpoint of the acromial end and the midpoint of the sternal end of the clavicle (
Fig. 2). Clinical outcomes were assessed using the University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score. Intraoperative and postoperative complications were also evaluated.
Statistical analysis was performed using IBM SPSS ver. 25.0 (IBM Corp.). The Wilcoxon signed-rank test was used for comparison of ASES and UCLA scores between preoperative and final follow-up evaluations. The point biserial correlation analysis, Kendall rank correlation analysis, and Spearman correlation test were used to determine the correlation between clinical outcomes and variables such as age, sex, involved side, cause of nonunion, initial treatment, interval from initial treatment to index surgery, union time, and final CLD. Statistical significance was set at P-values of <0.05.
Results
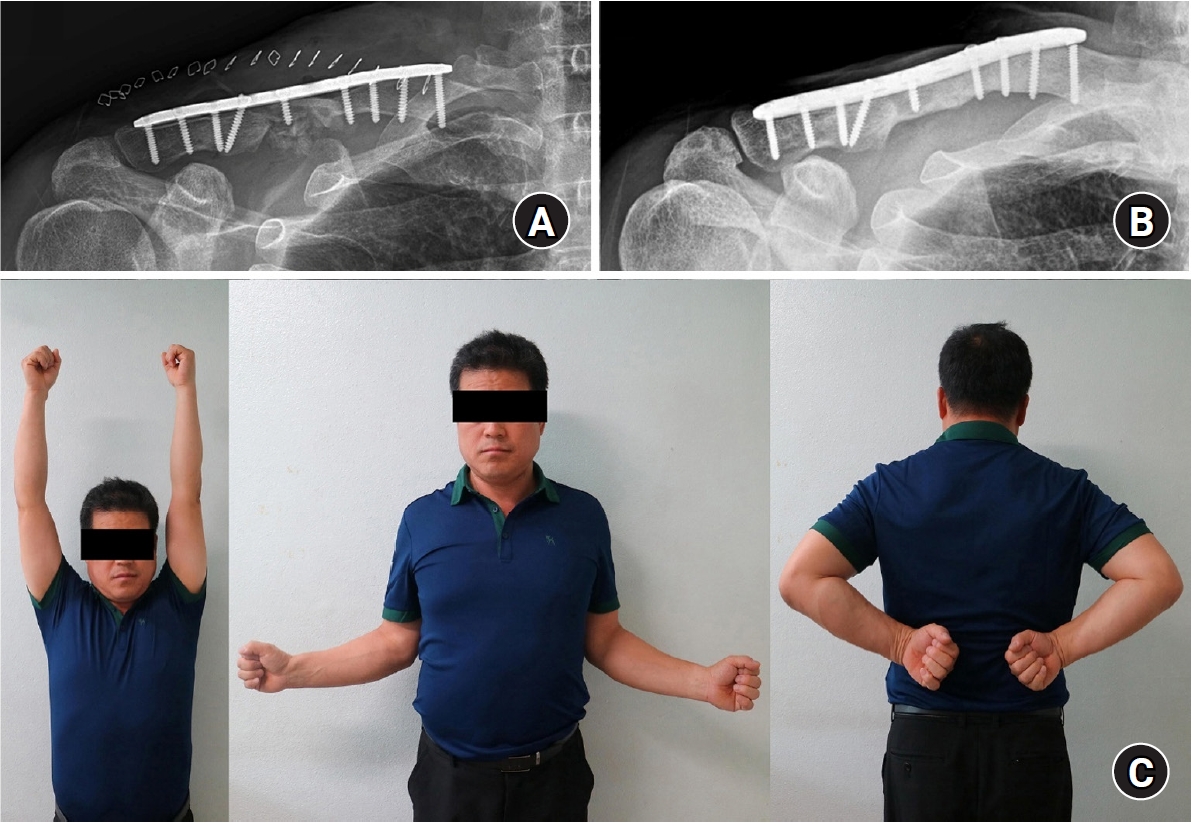
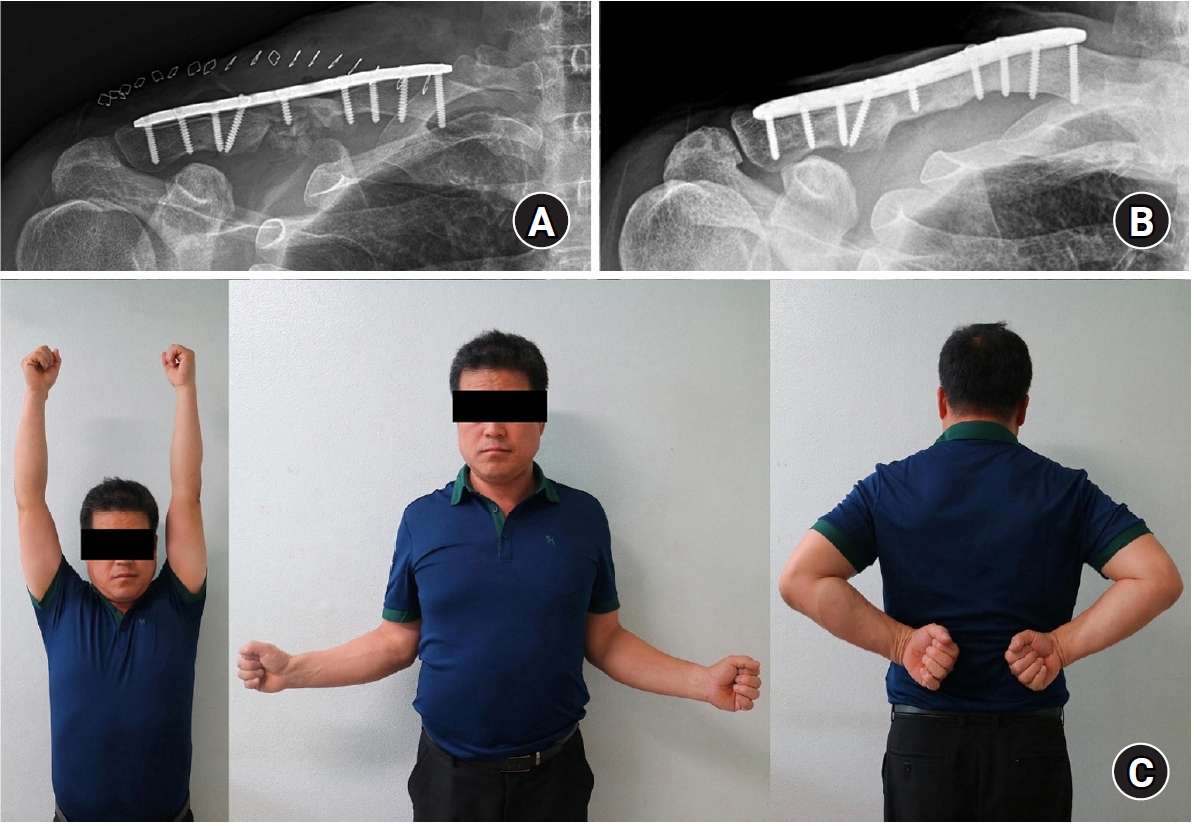
In all cases, complete bony union was achieved (
Figs. 3 and
4). The mean time of union was 17.6 weeks (range, 14–22 weeks). The mean CLD was significantly decreased from 9.1 mm (range, 2.5–16.4 mm) before surgery to 2.6 mm (range, 0.3–5.6 mm) after surgery (P<0.001).
The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001). The mean final Quick-DASH score was 18. No differences were observed between final clinical scores and variables including age, sex, involved side, cause of nonunion, initial treatment, interval from initial trauma to index surgery, union time, and final CLD (P>0.05) (
Table 2).
Three cases (17.6%) developed postoperative complications, including two cases of shoulder stiffness and one case of screw irritation. No donor site morbidity was found for any case. A patient (case no. 7) with shoulder stiffness underwent implant removal and arthroscopic capsular release at 12 months after the index surgery. A patient (case no. 11) with screw irritation underwent implant removal at 18 months after the index surgery. Two patients (cases no. 8 and 10) without any discomfort underwent implant removal by patient’s request. There were no complications such as refracture after implant removal.
Discussion
Plate fixation with bone graft is considered the best choice for atrophic clavicle nonunion [
6,
15]. Undoubtedly, when compared with other fixation techniques, plate fixation has more advantages in controlling rotational force and recovering from clavicle shortening. However, techniques for plating or bone graft are still controversial.
Most surgeons agree that bone graft is necessary for the treatment of clavicle nonunion. Nevertheless, several studies have reported good radiological and clinical outcomes with plate fixation or external fixation without bone graft [
16,
17]. Huang et al. [
17] reported the utilization of a dynamic compression plate without bone graft is an effective option in cases with atrophic clavicle nonunion. In contrast, van der Meijden et al. [
3] recommended that plate fixation and bone graft is the best treatment option for symptomatic clavicle midshaft nonunion, including local bone graft for hypertrophic nonunion and iliac bone graft for atrophic nonunion.
Although there is controversy for the shortening of the clavicle length after fracture, it has been reported that, if the clavicle is shortened by more than 15–20 mm, it can cause shoulder abduction weakness and substantial problems in shoulder function due to abnormal kinematics [
6-
8]. Therefore, restoration of the clavicle length in surgical treatment of atrophic clavicle nonunion is important for recovery of shoulder function. Intercalary tricortical iliac bone graft or free vascularized bone graft has been reported as a good treatment options for atrophic nonunion with severe bone defect. Bone defects of 1.5–3 cm should be interposed with a tricortical iliac bone graft to prevent the shortening of the clavicle length [
6,
14]. A vascularized bone graft can be used for extremely rare cases with larger defects >3 cm [
6,
14].
A few surgeons have advocated the necessity of intercalary autogenous bone graft for atrophic clavicle nonunion [
7,
8,
11,
13,
14,
18]. Simpson and Jupiter [
18] reported excellent radiological and clinical outcomes after plate fixation with intercalary tricortical iliac bone graft for clavicle midshaft nonunion, especially in the case of atrophic nonunion or bone defect. Ballmer et al. [
11] reported satisfactory results after intercalary tricortical iliac bone graft in patients with bone defects over 15 mm. They emphasized that intercalary tricortical iliac bone graft is important for restoration of the function of the acromioclavicular joint and sternoclavicular joint with the preservation of the costoclavicular space [
11]. Rollo et al. [
8] reported intercalary allograft bone graft can be used in place of vascularized bone graft for cases with significant bone loss. Lim et al. [
12] introduced the dual bone graft technique with plate fixation, which showed satisfactory results. Bridging over the nonunion gap, iliac cortical bone graft was placed under the nonunion site and cancellous bone was packed into the gap [
12]. We totally agreed on the necessity of structural bone graft for atrophic clavicle nonunion and have used interpositional tricortical iliac bone graft technique for the cases with bone defect >10 mm after resection of both sclerotic margins. The present study demonstrated that this technique for atrophic clavicle nonunion produced excellent the radiological and clinical outcomes. To prevent shortening of the clavicle length and provide structural support, a tricortical iliac bone with 2–3 mm long to match the length of the bone defect area was harvested. Accordingly, a tricortical iliac bone block was interposed in a somewhat tight manner. Then, plate and screws were fixed using a dynamic compression technique. These meticulous procedures may have a positive effect on complete bone healing and prevention of refracture after implant removal. The results of this study have led us to believe that several factors attributed to the excellent radiological and clinical outcomes. First, the interpositional tricortical bone graft restored the clavicle length. Second, a dynamic compression plating technique with autogenous bone graft provided both biological healing ability and mechanical stability.
Surgeries for clavicle midshaft nonunion are related to more complications when compared with those for acute fractures [
13,
19,
20]. Faraud et al. [
19] reported that 15 out of 21 cases (71.4%) achieved complete bone healing after plate fixation and bone graft for the clavicle midshaft nonunion. Six cases with complications required a revision procedure, including three cases of infection and three cases of fixation failure. Wiss and Garlich [
20] reported that 63 out of 71 cases (87.3%) achieved complete bone union after plate fixation with or without bone graft for the clavicle midshaft nonunion. Three cases (4.2%) with revision surgery achieved bone union, but six cases (8.5%) had remained nonunion. Clavicle nonunions caused by failed previous surgery can decrease the biologic healing potential and may lead to failure of union after the revision surgery [
12]. In the present study, 12 cases presented with atrophic nonunion after surgery including, nine cases of fixation failure and three cases of fracture-related infection. However, all cases achieved complete bone union without any major complications.
Superior plating is associated with hardware prominence due to the subcutaneous position of the plate and sometimes needed hardware removal [
1]. Hollo et al. [
7] reported that plate fixation with cortical bone graft for clavicle nonunion produced a high rate of bone union with restoration of the clavicle length. However, four refractures occurred after plate removal and three of them required revision [
7]. Disadvantages of autogenous iliac bone graft included the limited volume of available bone, increased operative time, and donor site morbidity such as pain, hematoma formation, and iliac fracture [
6,
15,
20]. Beirer et al. [
13] reported excellent clinical and radiologic results after iliac bone graft and plate fixation for 14 cases with clavicle nonunion or malunion. However, two cases experienced a secondary fracture of the anterior superior iliac spine as a complication at the donor site and one case experienced refracture after implant removal [
13]. They emphasized that the decision and timing of implant removal should be individually and carefully counseled. The present study revealed that three cases (17.6%) had postoperative complications, including two cases of shoulder stiffness and one case of screw irritation. No donor site morbidity was found for any case. Although only four cases had implant removal, the patients did not have refracture after implant removal.
This study has several limitations. First, this is a retrospective study. Second, the number of cases was small. Third, there was no comparison with the control group. Fourth, clavicle length measured by plain radiograph may not be accurate due to distorted rotation caused by X-ray beams.
Conclusions
Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length.
Article Information
-
Author contributions
Conceptualization: ESS. Data curation, Formal analysis: BSP, CJY. Writing-original draft: ESS, BSP. Writing-review & editing: CJY, CHC. All authors read and approved the final manuscript.
-
Conflict of interest
None.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
Fig. 1.Steps of the interpositional tricortical iliac bone graft with plate fixation. (A) Exposure of the nonunion site. (B, C) Resection of sclerotic bone with trimming both margins to be perpendicular to the long axis of the clavicle. (D) Measurement of the length of the bone defect. (E) Interposition of tricortical iliac bone block between both fragments. (F) Plate and screws fixation.
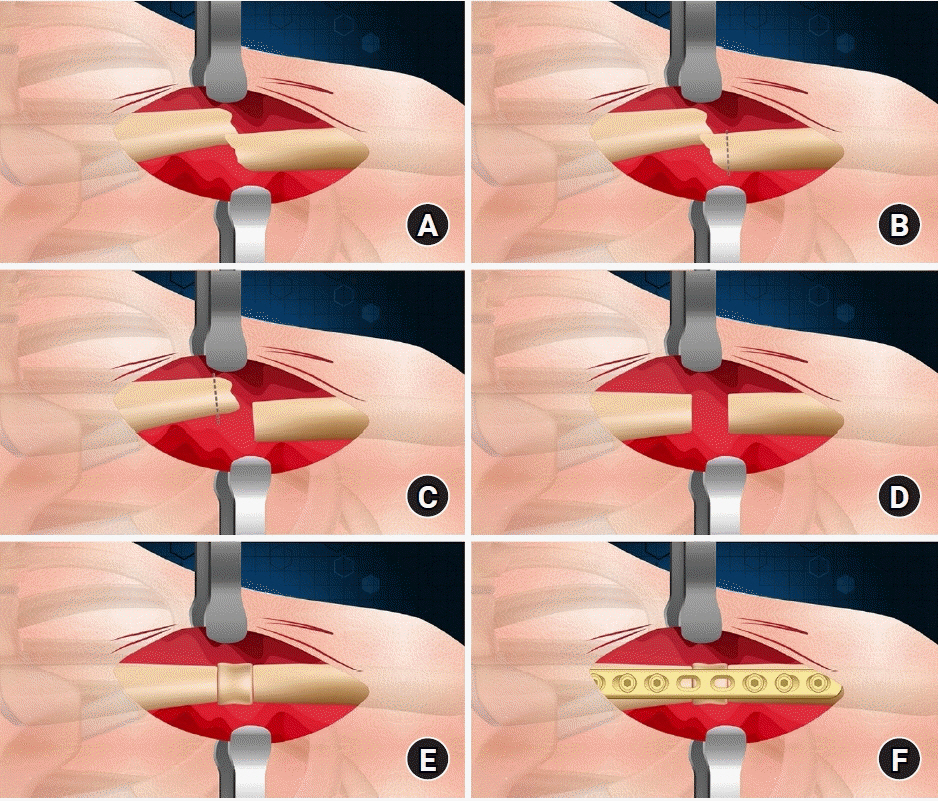
Fig. 2.Preoperative radiographs of 48-year-old man (case no. 14) with right atrophic clavicle nonunion. The clavicle length (red line) was determined on standard anteroposterior plain radiograph by measuring the linear distance between the midpoint of the acromial end and the midpoint of the sternal end of the clavicle.
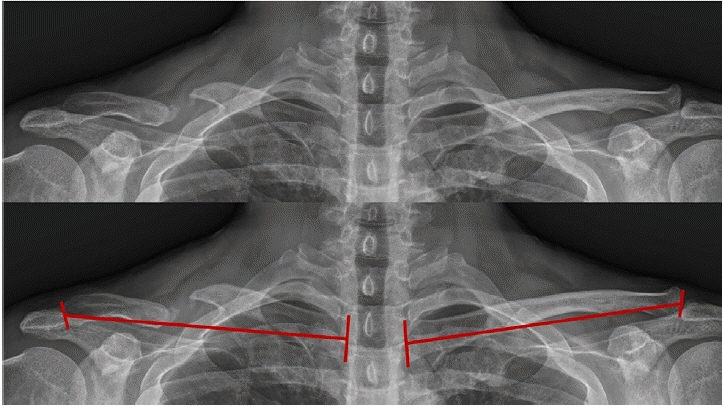
Fig. 3.Intraoperative photos (case no. 14). (A) Sufficient resection of sclerotic bone. (B) Measurement of the length of the bone defect. (C) Interposition of tricortical iliac bone block. (D) Plate and screws fixation.
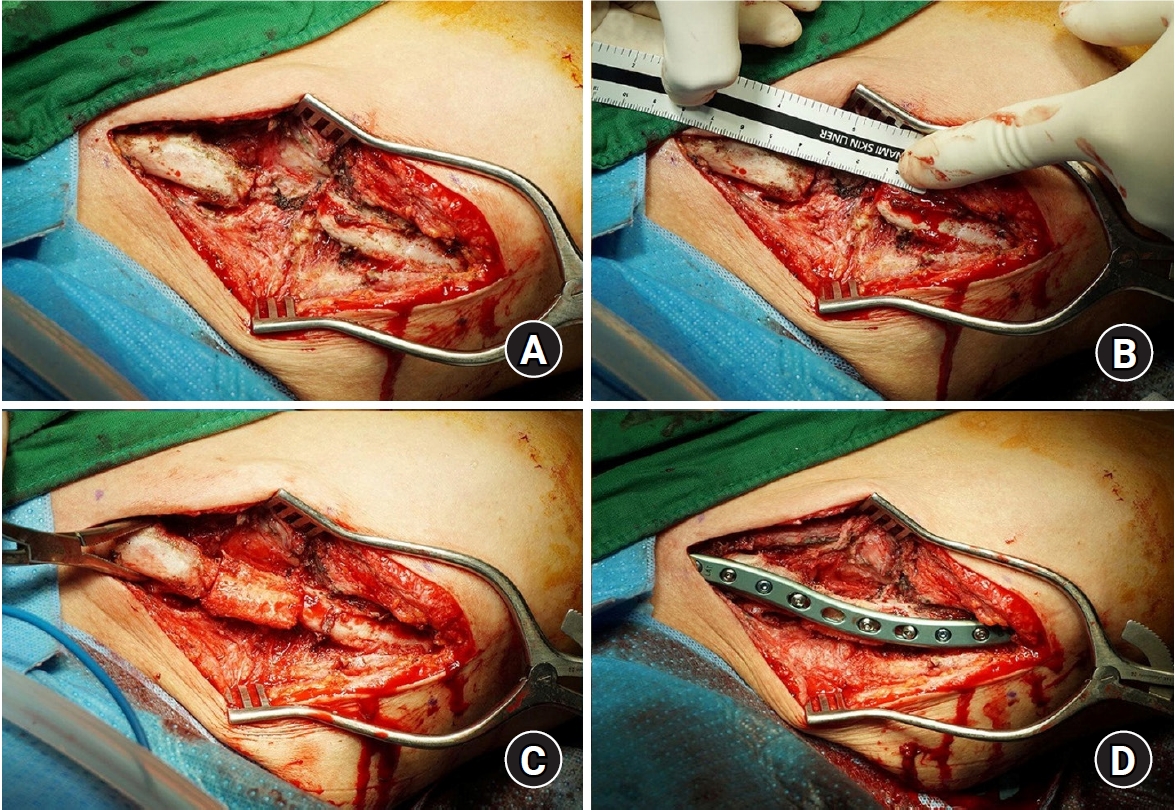
Fig. 4.Postoperative radiographs and clinical photos (case no. 14). (A) Immediate postoperative image. (B) Image at final follow-up evaluation. (C) Clinical photos at final follow-up evaluation. Written informed consent for using the images was obtained from the patient.
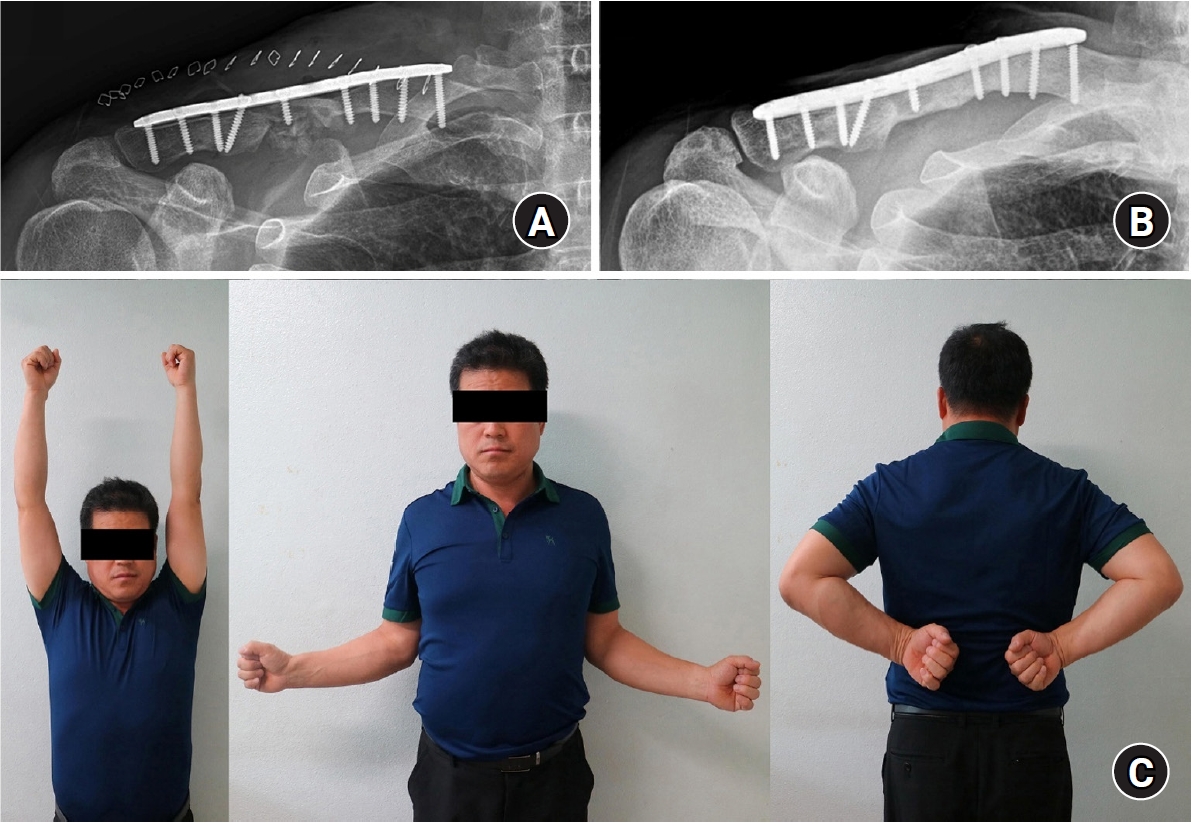
Table 1.Demographic and clinical data of 17 patients
|
Case no. |
Sex |
Age (yr) |
Involved side |
Initial treatment |
Interval from IT to IS (mo) |
Union time (mo) |
UCLA score
|
ASES score
|
Final Quick- DASH score |
FU period (mo) |
CLD
|
Complication |
|
Preoperative |
Final |
Preoperative |
Final |
Preoperative |
Postoperative |
|
1 |
Male |
64 |
Left |
Conservative |
7 |
17 |
15 |
35 |
57 |
100 |
0 |
193 |
6.9 |
4.9 |
- |
|
2 |
Male |
70 |
Left |
Conservative |
12 |
16 |
21 |
35 |
64 |
100 |
0 |
190 |
14.9 |
4.1 |
- |
|
3 |
Male |
56 |
Right |
ORIF |
20 |
16 |
14 |
26 |
43 |
81 |
46 |
41 |
15.2 |
5.6 |
Stiffness |
|
4 |
Male |
44 |
Left |
Conservative |
10 |
18 |
17 |
22 |
58 |
65 |
65 |
49 |
16.4 |
5.3 |
- |
|
5 |
Male |
66 |
Left |
ORIF |
16 |
22 |
20 |
33 |
54 |
96 |
27 |
31 |
15.7 |
0.7 |
- |
|
6 |
Male |
60 |
Left |
ORIF |
5 |
17 |
13 |
27 |
32 |
87 |
38 |
18 |
8.2 |
1.1 |
- |
|
7 |
Female |
53 |
Right |
Conservative |
60 |
20 |
17 |
26 |
59 |
81 |
43 |
167 |
10.2 |
2.2 |
Stiffness |
|
8 |
Male |
65 |
Right |
Conservative |
7 |
14 |
19 |
33 |
51 |
90 |
5 |
162 |
9.8 |
1.6 |
- |
|
9 |
Male |
52 |
Right |
ORIF |
7 |
20 |
18 |
30 |
59 |
87 |
30 |
149 |
7.5 |
1.9 |
- |
|
10 |
Male |
42 |
Left |
ORIF |
9 |
20 |
20 |
33 |
54 |
95 |
2 |
136 |
2.5 |
1.3 |
- |
|
11 |
Male |
39 |
Right |
ORIF |
6 |
18 |
13 |
33 |
15 |
95 |
2 |
120 |
12.8 |
0.3 |
Screw irritation |
|
12 |
Male |
60 |
Right |
ORIF |
9 |
16 |
20 |
33 |
43 |
90 |
5 |
120 |
9.3 |
3.0 |
- |
|
13 |
Male |
69 |
Right |
ORIF |
13 |
16 |
15 |
33 |
48 |
95 |
2 |
90 |
3.5 |
2.8 |
- |
|
14 |
Male |
48 |
Right |
ORIF |
32 |
18 |
33 |
35 |
93 |
100 |
0 |
82 |
2.5 |
1.9 |
- |
|
15 |
Female |
40 |
Left |
ORIF |
15 |
14 |
22 |
33 |
70 |
100 |
2 |
80 |
3.8 |
1.9 |
- |
|
16 |
Female |
22 |
Left |
ORIF |
5 |
16 |
10 |
27 |
28 |
80 |
5 |
71 |
11.0 |
1.4 |
- |
|
17 |
Male |
48 |
Left |
ORIF |
11 |
22 |
21 |
26 |
60 |
65 |
30 |
39 |
5.0 |
3.7 |
- |
Table 2.Correlations between final clinical scores and variables
|
Variable |
Final UCLA score
|
Final ASES score
|
Final Quick-DASH score
|
|
r |
P-value |
r |
P-value |
r |
P-value |
|
Age |
0.357 |
0.159 |
0.321 |
0.208 |
–0.014 |
0.957 |
|
Sex |
–0.227 |
0.382 |
–0.070 |
0.789 |
–0.025 |
0.923 |
|
Involved side |
0.219 |
0.399 |
0.139 |
0.595 |
–0.182 |
0.484 |
|
Type of nonunion |
–0.157 |
0.544 |
–0.132 |
0.606 |
0.327 |
0.197 |
|
Initial treatment |
0.064 |
0.808 |
0.086 |
0.743 |
–0.155 |
0.552 |
|
From IT to IS |
0.009 |
0.973 |
0.188 |
0.470 |
0.047 |
0.859 |
|
Union time |
–0.249 |
0.334 |
–0.218 |
0.401 |
0.272 |
0.291 |
|
CLD |
–0.217 |
0.402 |
–0.166 |
0.525 |
0.099 |
0.705 |
References
- 1. deMeireles AJ, Czerwonka N, Levine WN. Clavicle nonunion and malunion: surgical interventions for functional improvement. Clin Sports Med 2023;42:663-75.PubMed
- 2. Kim SC, Yoo JC, Park JH, et al. Changes in shoulder trauma during the COVID-19 pandemic: a South Korean Survey. Clin Orthop Surg 2023;15:300-7.ArticlePubMedPMCPDF
- 3. van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg 2012;21:423-9.ArticlePubMed
- 4. Jo YH, Lee BG. Clavicle midshaft fractures should not be considered an easy surgery: reduction and prebending. Clin Shoulder Elb 2023;26:341-2.ArticlePubMedPMCPDF
- 5. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. systematic review of 2144 fractures. On behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma 2005;19:504-7.PubMed
- 6. Martetschläger F, Gaskill TR, Millett PJ. Management of clavicle nonunion and malunion. J Shoulder Elbow Surg 2013;22:862-8.ArticlePubMed
- 7. Hollo D, Kolling C, Audigé L, Moro F, Rikli D, Müller AM. Plating and cortical bone grafting of clavicular nonunions: clinical outcome and its relation to clavicular length restoration. JSES Int 2020;4:508-14.ArticlePubMedPMC
- 8. Rollo G, Vicenti G, Rotini R, et al. Clavicle aseptic nonunion: is there a place for cortical allogenic strut graft? Injury 2017;48 Suppl 3:S60-5.ArticlePubMed
- 9. Zhang J, Yin P, Han B, Zhao J, Yin B. The treatment of the atrophic clavicular nonunion by double-plate fixation with autogenous cancellous bone graft: a prospective study. J Orthop Surg Res 2021;16:22.ArticlePubMedPMCPDF
- 10. Zhang C, Ma T, Duan N, et al. Clinical and radiographic outcomes of revision with autogenous “structured” bone grafting combined with superior plate for recalcitrant atrophic nonunion of clavicular midshaft: a retrospective study. Int Orthop 2022;46:2585-92.ArticlePubMedPDF
- 11. Ballmer FT, Lambert SM, Hertel R. Decortication and plate osteosynthesis for nonunion of the clavicle. J Shoulder Elbow Surg 1998;7:581-5.ArticlePubMed
- 12. Lim S, Cho E, Chun JM, Jeon IH. Osteosynthesis with autologous dual bone graft for nonunion of midshaft clavicle fractures: clinical and radiological outcomes. Eur J Orthop Surg Traumatol 2022;32:159-65.ArticlePubMedPDF
- 13. Beirer M, Banke IJ, Harrasser N, et al. Mid-term outcome following revision surgery of clavicular non- and malunion using anatomic locking compression plate and iliac crest bone graft. BMC Musculoskelet Disord 2017;18:129.ArticlePubMedPMCPDF
- 14. Grewal S, Baltes TP, Wiegerinck E, Kloen P. Treatment of a recalcitrant non-union of the clavicle. Strategies Trauma Limb Reconstr 2022;17:1-6.ArticlePubMedPMC
- 15. Riggenbach MD, Jones GL, Bishop JY. Open reduction and internal fixation of clavicular nonunions with allograft bone substitute. Int J Shoulder Surg 2011;5:61-7.ArticlePubMedPMC
- 16. Benshabat D, Factor S, Maman E, et al. Addition of bone marrow aspirate concentrate resulted in high rate of healing and good functional outcomes in the treatment of clavicle fracture nonunion: a retrospective case series. J Clin Med 2021;10:4749.ArticlePubMedPMC
- 17. Huang HK, Chiang CC, Su YP, et al. Role of autologous bone graft in the surgical treatment of atrophic nonunion of midshaft clavicular fractures. Orthopedics 2012;35:e197-201.ArticlePubMed
- 18. Simpson NS, Jupiter JB. Evaluation and surgical management. J Am Acad Orthop Surg 1996;4:1-8.PubMed
- 19. Faraud A, Bonnevialle N, Allavena C, Nouaille Degorce H, Bonnevialle P, Mansat P. Outcomes from surgical treatment of middle-third clavicle fractures non-union in adults: a series of 21 cases. Orthop Traumatol Surg Res 2014;100:171-6.ArticlePubMed
- 20. Wiss DA, Garlich JM. Clavicle nonunion: plate and graft type do not affect healing rates. A single surgeon experience with 71 cases. J Shoulder Elbow Surg 2021;30:679-84.ArticlePubMed
 , Bum-Soon Park, MD
, Bum-Soon Park, MD , Chang-Jin Yon, MD, PhD
, Chang-Jin Yon, MD, PhD , Chul-Hyun Cho, MD, PhD
, Chul-Hyun Cho, MD, PhD



 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

