Articles
- Page Path
- HOME > J Korean Fract Soc > Volume 37(1); 2024 > Article
- Original Article Cephalomedullary Nailing with an Additional Cannulated Screw Fixation in Basicervical Femur Fractures
- Keong-Hwan Kim, Woo Dong Nam, Yeon Sik Heo, Gu-Hee Jung
-
Journal of The Korean Orthopaedic Trauma Association 2024;37(1):22-29.
DOI: https://doi.org/10.12671/jkfs.2024.37.1.22
Published online: January 31, 2024
2Department of Orthopedic Surgery, Gyeongsang National University School of Medicine, Jinju, Korea
- 1,269 Views
- 14 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
The purpose of this study is to analyze the clinical results of patients with basicervical fracture undergoing cephalomedullary nailing (CMN) with an additional cannulated screw fixation compared to only performing CMN. We hypothesized that a difference may exist in the clinical outcomes if an ad-ditional screw is fixed with CMN compared to only performing CMN in basicervical fracture.
Materials and Methods
A total of 28 consecutive patients who underwent CMN for basicervical fracture were included. In 9 cases, only CMN was conducted, and in 19 cases, an additional cannulated screw fixation was performed with CMN. Bone union, sliding distance, reduction status, and fixation failure were evaluated by postoperative radiography, and ambulatory ability was evaluated by functional results. These findings were compared between a group of CMN and a group of CMN with an additional cannulated screw.
Results
There were 4 males and 24 females with a mean age of 84 years (range, 69–100 years). No significant difference was found in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5–13.4 mm] vs 3.5 mm [range, 0.1– 9.2 mm]; p=0.045). Among the two groups, only one case of fixation failure at the postoperative four months was observed in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
Published online Jan 24, 2024.
https://doi.org/10.12671/jkfs.2024.37.1.22
Abstract
Purpose
The purpose of this study is to analyze the clinical results of patients with basicervical fracture undergoing cephalomedullary nailing (CMN) with an additional cannulated screw fixation compared to only performing CMN. We hypothesized that a difference may exist in the clinical outcomes if an additional screw is fixed with CMN compared to only performing CMN in basicervical fracture.
Materials and Methods
A total of 28 consecutive patients who underwent CMN for basicervical fracture were included. In 9 cases, only CMN was conducted, and in 19 cases, an additional cannulated screw fixation was performed with CMN. Bone union, sliding distance, reduction status, and fixation failure were evaluated by postoperative radiography, and ambulatory ability was evaluated by functional results. These findings were compared between a group of CMN and a group of CMN with an additional cannulated screw.
Results
There were 4 males and 24 females with a mean age of 84 years (range, 69–100 years). No significant difference was found in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5–13.4 mm] vs 3.5 mm [range, 0.1–9.2 mm]; p=0.045). Among the two groups, only one case of fixation failure at the postoperative four months was observed in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
초록
목적
대퇴 경부 기저부 골절 환자에서 골수정 고정과 함께 추가적인 유관 나사못 고정을 시행한 환자 증례들을 골수정 단독 시행한 환자 증례와 비교하여 임상적 결과를 분석하고자 하였다.
대상 및 방법
골수정 고정을 시행한 28명의 연속된 대퇴 경부 기저부 골절 환자들을 대상으로 하였다. 9명은 골수정 단독으로 시행하였고, 19명은 골수정과 함께 추가 유관 나사못 고정을 시행하였으며 두 군 간 방사선학적 및 기능적 결과를 비교하였다.
결과
남자 4명, 여자 24명이었고, 평균 나이는 84세(범위 69-100세)였다. 수술 후 보행 능력 회복은 두 군 간 유의한 차이를 보이지 않았으나, 래그 스크류의 슬라이딩 거리는 골수정 단독군에서 유의하게 더 큰 슬라이딩 거리를 보였다(6.2 mm [범위 2.5-13.4 mm] vs 3.5 mm [범위 0.1-9.2 mm]; p=0.045). 두 군 전체 환자 중 골수정 단독으로 시행한 1예에서 수술 후 4개월에 고정 실패 소견을 보였고(p=0.321), 금속 제거 후 인공 고관절 반치환술을 시행하였다.
결론
대퇴 경부 기저부 골절에서 골수정 고정과 함께 추가적인 유관 나사못을 고정하는 술식은 안전하고 신뢰할 만한 수술 방법이다. 이 방법은 양호한 임상 경과를 보여주며 대퇴 경부 기저부 골절 치료에 있어 좋은 대안이 될 수 있을 것이다.
Introduction
Basicervical femur fracture is a rare hip fracture that occurs at the base of the femoral neck and is morphologically distinct from other hip fractures.1) Basicervical fracture is known to be a relative risk factor for fixation failure due to biomechanical instability of the fracture caused by its location and morphological characteristics.2,3,4) When osteosynthesis is considered for basicervical fracture, a sliding hip screw and cephalomedullary nail are primarily used as in other pertrochanteric fractures; however, optimal treatment for this fracture is still controversial.1,5) Nonetheless, several authors reported optimal results for the use of cephalomedullary nailing (CMN) and recommended the nail in these fractures.6,7)
Rotational instability is one of the concerns in basicervical fracture, and additional reinforcement to provide stability, such as a derotational screw, can be considered when using a conventional lag screw pattern device.8) Despite these considerations, there are several reports that a sliding hip screw with an additional screw are not superior to a sliding hip screw alone in biomechanical and clinical studies.9,10) However, there is a lack of studies using a cephalomedullary nail with an additional screw for basicervical fractures.
We hypothesized that a difference in clinical outcomes will be observed if an additional screw is fixed with CMN compared to only performing CMN in basicervical fracture. When performing CMN for proximal femoral fractures, an additional screw fixation from the lateral trochanteric area to the femoral head is technically demanding, because there is limited space due to the volume of the proximal portion of the nail. The present study describes a surgical technique for inserting an additional cannulated screw through a reverse sequential technique when performing CMN and reports the clinical outcomes of patients with basicervical fracture using this technique compared to nailing alone.
Materials and Methods
This study was conducted after approval of the Institutional Review Board of Kangwon National University Hospital (2022-09-007), and informed consent was waived due to the retrospective nature of the study. Of the 518 patients aged 60 years or older who underwent surgery for hip fractures by one author (K.H.K.) in Kangwon National University Hospital from September 2018 to May 2022, 33 consecutive patients with basicervical fractures who underwent CMN were reviewed. Basicervical fracture was defined as a fracture at the base of the femoral neck, above the lesser trochanter, without involvement of the lesser trochanter, and was noted to be a two-part fracture on plain radiography.4) From November 2020, an additional cannulated screw was fixed to the anterior part of the nail. Those who were followed for more than 12 months, or who obtained bone union and recovered their ambulatory ability to preinjury levels even before 12 months, were included. In the study, a total of 28 patients were included as 5 patients were lost to follow-up before bone union was achieved. In 9 cases, only CMN was performed, and in 19 cases, an additional cannulated screw fixation was employed with CMN.
1. Surgical technique and postoperative protocol
After the patient was placed on a fracture table under spinal or general anesthesia, a closed reduction was performed by adjusting the affected leg. Next, CMN (Gamma3 Trochanteric Nail; Stryker Trauma GmbH) was performed.
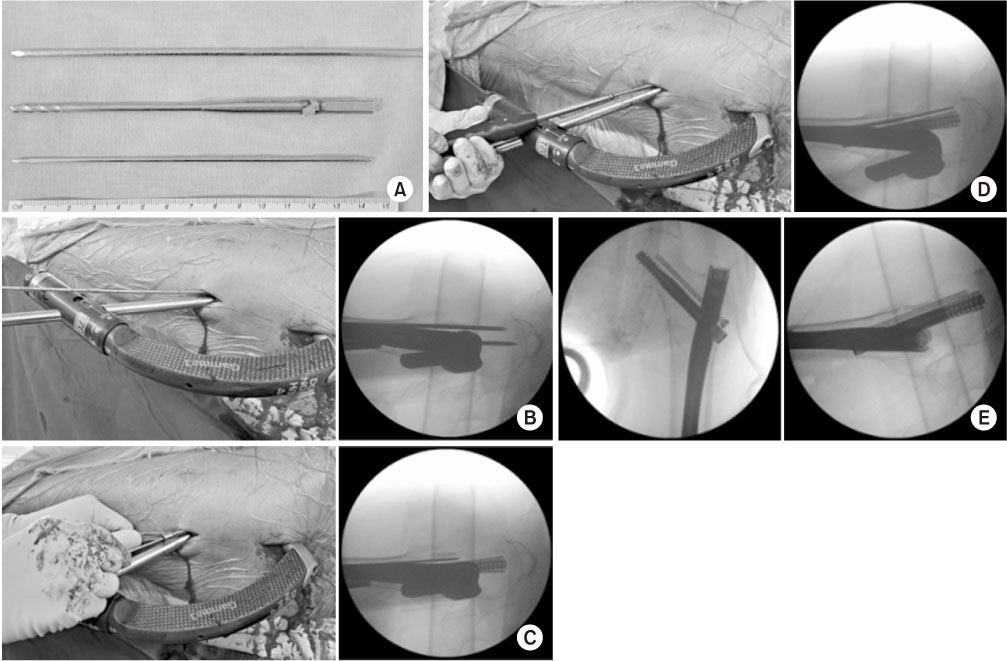
The nail was inserted from the tip of the greater trochanter using the conventional method of entry using a guide pin. After confirming an anatomical reduction of the fracture, a lag screw was inserted. In all cases, to prevent rotation and to allow lateral sliding of the lag screw, the set screw of the lag screw was fixed. In cases of an additional cannulated screw fixation, a 5.0 mm-diamter partially-threaded cannulated screw was inserted in the anterior part of the nail. For technical convenience, guide pin insertion and core reaming were performed in a reverse sequence to insert the cannulated screw. For insertion of the cannulated screw, we used custom-made 3.5 mm-diameter long pin (the same diameter as the core reamer for a 5.0 mm-diameter cannulated screw) and guide pin of the 5.0 mm cannulated screw (Fig. 1A, from top to bottom, the 3.5 mm-diameter long pin, the core reamer, and the guide pin). Before fully engaging the lag screw to the subchondral bone of the femoral head, the custom-made long pin was inserted into the anterior part of the nail from the lateral femoral cortex to the femoral head. Since the guide pin of the 5.0 mm cannulated screw is thin and short, it is difficult to use during the nailing procedure, so a diameter corresponding to the core of the 5.0 mm cannulated screw was tunneled first using the custom-made pin (Fig. 1B). After the lag screw was fully engaged in the subchondral bone, the custom-made pin was removed and manually replaced with the guide pin that was originally used on the 5.0 mm cannulated screw (Fig. 1C). A 5.0 mm cannulated screw was inserted along the guide pin (Fig. 1D). The length of the cannulated screw was selected to be approximately 2 cm shorter than the lag screw given the length of the lag screw and its positional relationship. Following fixation, confirmation that the cannulated screw was appropirately inserted in the anterior part of the nail was obtained (Fig. 1E). After completing insertion of the lag screw and cannulated screw, one distal interlocking screw was inserted.
Fig. 1
Procedure of fixing an additional cannulated screw. Instruments (A), the additional screw fixation during cephalomedullary nailing (B-D), and fluoroscopic images after the fixation (E).
Postoperatively, wheelchair mobilization was started on postoperative day 1, and ambulation using walking aids was implemented, within an acceptable range for pain and the patients’ general condition, on postoperative day 2.
2. Radiographic and functional evaluation
Reduction status was evaluated through plain radiographs of anteroposterior (AP) and translateral views taken immediately after surgery. Alignment and displacement of the main fragments were evaluated according to the method suggested by Fogagnolo et al.,11) and the reduction status was evaluated as good, acceptable, or poor. The tip-apex distance was also measured on the plain radiographs taken immediately after surgery.12)
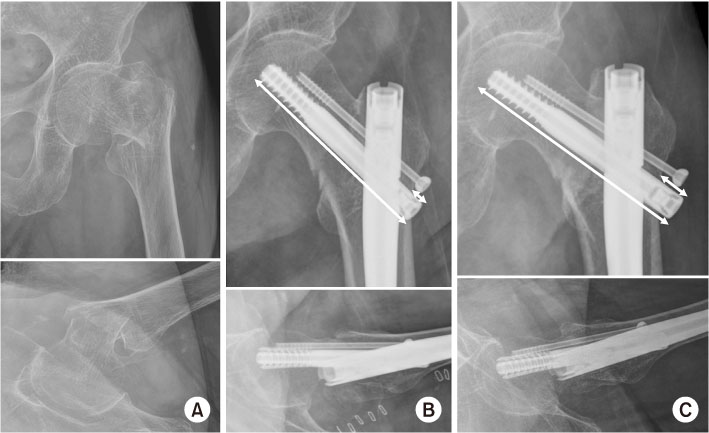
During follow-up, it was determined that bone union was achieved when the radiolucent gap at the fracture site disappeared and bony consolidation was confirmed. Sliding distance of the lag screw was evaluated by laterally protruded length of the lag screw during follow-up through comparison of the AP plain radiographs at both immediate after surgery and the last (Fig. 2). Ambulatory ability was evaluated at the last follow-up visit13) and was compared with the preinjury status.
Fig. 2
Plain radiographs of an 85-year-old female patient with a basicervical fracture at the preoperative (A), postoperative (B), and at the last follow-up of 14 months (C). The laterally protruded length of the lag screw was calculated by multiplying the ratio of the length of the lag screw (long arrows) and the length protruding outward (short arrows) by the actual length of the lag screw.
3. Statistical analysis
IBM SPSS (ver. 21.0; IBM Corp.) was used for statistical comparisons between a group of CMN and a group of CMN with an additional cannulated screw (CMN+S). The Mann–Whitney U test was used to compare continuous variables, and the Fisher’s exact test was used to compare frequencies. A p<0.05 was considered statistically significant.
Results
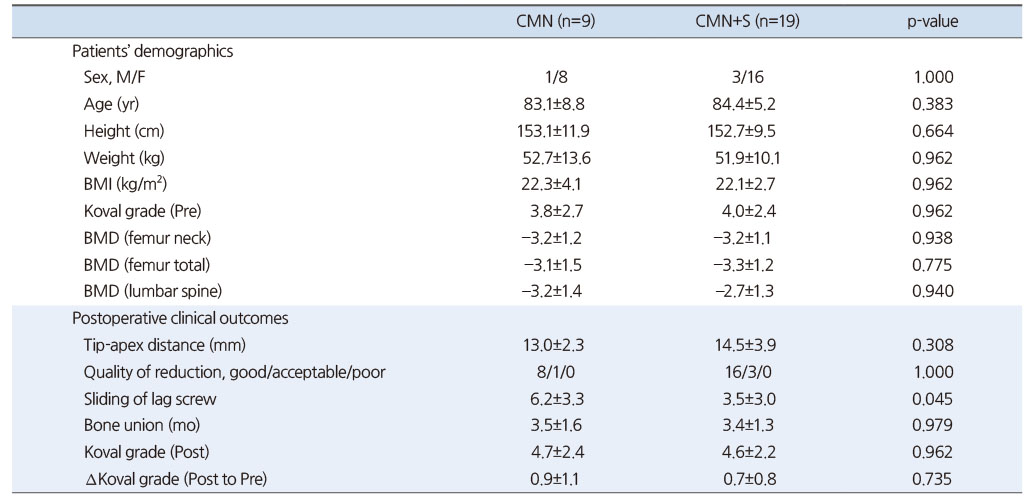
There were 4 males and 24 females with a mean age of 84 years (range, 69-100 years). The patients’ demographic characteristics demonstrated no significant difference between the two groups (Table 1).
Table 1
Comparison between CMN Group and CMN+S Group
In all patients, no difficulty was encountered with inserting the cannulated screw into the anterior part of the nail using the reverse sequential technique. No intraoperative complications including neurovascular injury were documented. In terms of operation time, no significant difference was found with a mean of 35 minutes (range, 15-60 minutes) in the CMN group and a mean of 35.5 minutes (range, 20-65 minutes) in the CMN+S group.
Additionally, no significant differences were observed in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5-13.4 mm] vs 3.5 mm [range, 0.1-9.2 mm]; p=0.045, Table 1).
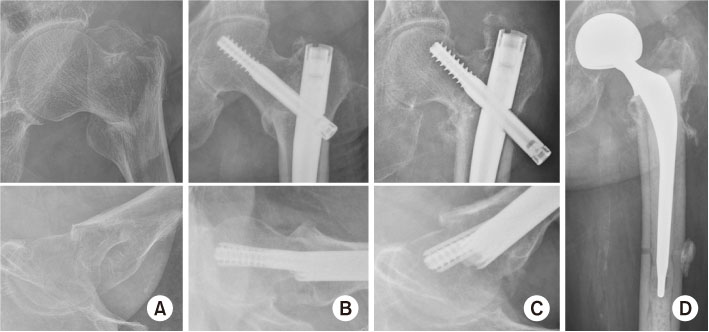
Among the two groups, only one case of fixation failure was documented at the postoperative four months in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed (Fig. 3).
Fig. 3
(A, B) An 82-year-old female patient underwent cephalomedullary nailing for a basicervical fracture. (C, D) Hemiarthroplasty was conducted at postoperative 4 months due to fixation failure.
Discussion
When performing osteosynthesis for basicervical fracture, both extramedullary and intramedullary devices can be used.14) In a multicenter comparative study by Lee et al.,7) they reported that fixation failure was more common with a sliding hip screw than with CMN in basicervical fracture, and the use of CMN was recommended. Regardless of the surgical options for osteosynthesis, in terms of stability of the fracture itself, there are concerns over the proximal fragment impacting into the distal fragment and rotational instability due to the morphological characteristics of the fracture itself. These are suggested to be causes of the relatively higher fixation failure rate.4,8) Furthermore, several authors reported basicervical fracture as one of the risk factors for fixation failure when performing CMN for pertrochanteric fracture.15,16) One possible way to address this problem could be using an additional screw.8) Although an additional screw has been used traditionally with a sliding hip screw, there is a paucity of reports of CMN. In the present study, an additional screw fixation using the reverse sequential technique during CMN was performed, and it resulted in favorable clinical outcomes compared to only performing CMN.
There are previous biomechanical and clinical studies utilizing a sliding hip screw with an additional screw fixation for basicervical fracture, and the results were somewhat inconsistent.9,10,17) Massoud reported favorable clinical outcomes in a case series where basicervical fractures were treated with a sliding hip screw with an additional screw.17) However, in a retrospective comparative study of clinical results for basicervical fractures utilizing a sliding hip screw with or without an additional screw, Su et al.10) reported that the additional screw resulted in less collapse on radiographic measurement, but there was no functional benefit. Also, in Blair et al.’s biomechanical study9) using the osteoporotic cadaveric femur, an additional screw did not significantly increase stability when the sliding hip screw was fixed.
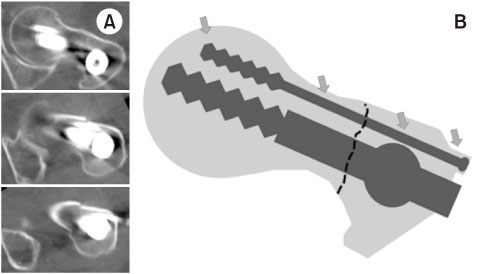
To understand the role of the additional screw, it is necessary to understand the positional relationship of the additional screw with the proximal femur and main implants. Postoperative computed tomographic axial images of a patient undergoing CMN with an additional screw fixation show the positional relationship of the additional screw, and it can be confirmed that the additional screw has multiple reliable mechanical supporting areas despite being in the osteoporotic proximal femur (Fig. 4A). The additional screw is reliably supported in multiple areas, including the subchondral bone of the femoral head, the subcortical area of the femoral neck, the blocking effect of the nail itself, and the lateral cortical bone of the proximal femur (Fig. 4B). In contrast, in the case of a sliding hip screw, the additional screw is likely to provide limited fixation force on the subchondral bone of the femoral head and the lateral cortex of the proximal femur. The results of this study support the hypothesis that the additional screw fixation in CMN for basicervical fracture can be helpful in reinforcing stability given the positional relationship.
Fig. 4
(A) The axial scan confirmed the positional relationship of the additional screw. (B) Schematic diagram of the positional relationship of the additional screw. The additional screw was reliably supported in multiple areas (four arrows).
Gadegone et al.18) reported good clinical results by fixing an additional screw in addition to the nail in unstable trochanteric fractures. In their case series, reoperation and excessive collapse were reduced compared to previous reports, and stability augmentation by the additional screw was suggested as the reason. Their additional screw was 6.4 mm in diameter. However, in our experience, especially in female patients with a small bony structure, it was difficult to insert additional screws more than 6 mm in diameter due to spatial limitations during CMN. A 5.0 mm-diameter cannulated screw was used as the additional screw through a reverse sequential technique in the present study to overcome these difficulties, and the procedure went well without any difficulties in all patients. Because the thickness of the screw is reduced, it may provide relatively less fixation force. However, the additional screw itself was used to augment stability, and there are multiple reliable supporting areas around the additional screw. Therefore, this smaller screw should serve as a secure support in the fixation construct.
There are several limitations to this study. First, this was a retrospective comparative study with a small number of patients. Although this may be a weakness in the study design, nevertheless this is a meaningful study in terms of alerting surgeons to the possibility of an alternative surgical option for a rare hip fracture. In the future, biomechanical studies and larger-scale prospective comparative studies are warranted to provide guidance on the treatment direction of these fractures. Finally, since one cephalomedullary nail was used in all patients, even if the design of cephalomedullary nails is for the most part similar, it may be difficult to generalize to all types of cephalomedullary nails.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
Financial support:None.
Conflict of interests:None.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

