Search
- Page Path
- HOME > Search
Original Articles
- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
- Han-Kook Yoon, So Ra Yoon, Kee-Bum Hong, Youngsu Jung, SeongJu Choi, Jun-Ku Lee
- J Musculoskelet Trauma 2026;39(1):12-19. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00297

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The COVID-19 pandemic is likely to have affected bone health in older adults in Korea. This study aimed to analyze changes in the epidemiology and management of distal radius fractures (DRFs) in older adults before and during the COVID-19 pandemic.
Methods
Patients with DRF aged over 50 years in 2017, 2018, 2020, and 2021 were included in this study. Patients were classified into a group with DRF occurring between 2017 and 2018 (before COVID-19) and a group with DRF occurring between 2020 and 2021 (during COVID-19). We calculated the incidence rates of DRF and compared them between the two groups. We also analyzed and compared demographic data (age, sex, income, residence) and the operation rate for DRF between the two groups. Patient selection and treatment were based on International Classification of Diseases, 10th revision codes.
Results
A total of 140,634 patients with DRF (before COVID-19, 69,794; during COVID-19, 70,840) were included. The incidence of DRF before COVID-19 (184.4/100,000 person-years) was higher than during COVID-19 (169.8/100,000 person-years). The operation rate was higher during COVID-19 (86.9%) than before COVID-19 (83.3%).
Conclusion
During the COVID-19 pandemic, the incidence of DRF decreased in South Korea. However, the rate of surgical treatment increased and exceeded the global surgical rate. Level of evidence: III.
- 212 View
- 6 Download

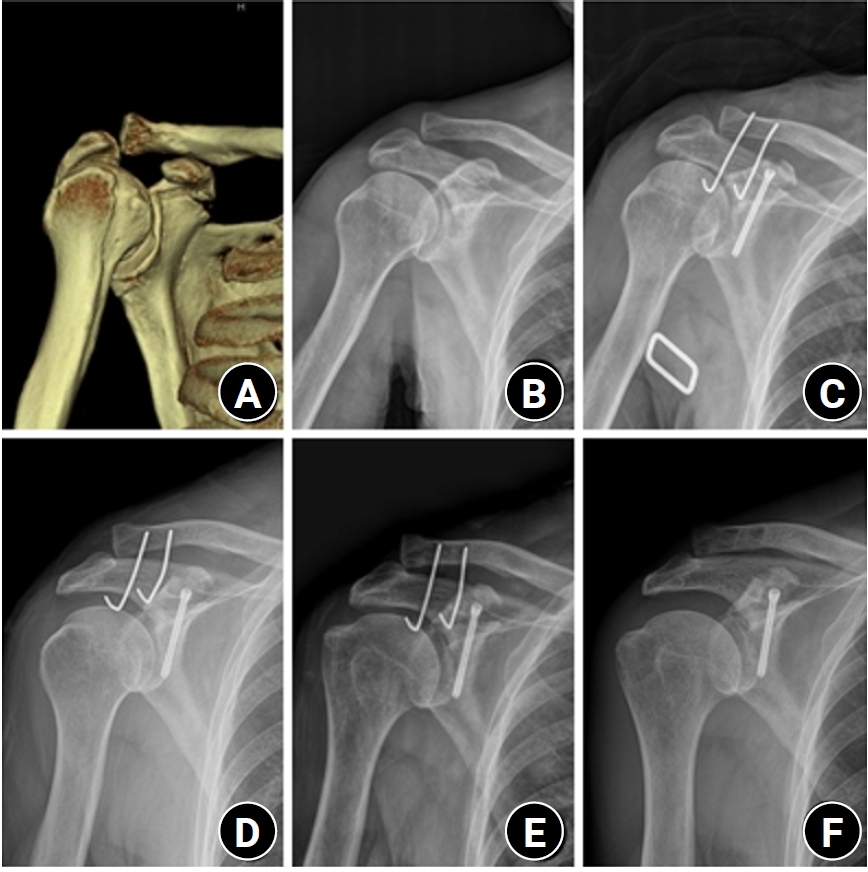
- Surgical outcomes of the coracoid process fracture associated with the acromioclavicular joint injury in Korea: a case series
- Dongju Shin, Sung Choi, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2026;39(1):54-61. Published online January 14, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00346
-
 Abstract
Abstract
 PDF
PDF - Background
Excluding technical reports and isolated case reports, there are no published studies evaluating coracoid process fixation with or without an acromioclavicular joint (ACJ) stabilization procedure for coracoid process fractures associated with ACJ injury. The purpose of this study was to assess the surgical outcomes of coracoid process fractures associated with ACJ injuries and to determine the usefulness of coracoid process fixation with or without an ACJ stabilization procedure.
Methods
From February 2006 to December 2015, patients with coracoid process fractures associated with ACJ injuries were enrolled. Radiological and clinical outcomes were analyzed in 12 patients who underwent coracoid process fixation with or without an ACJ stabilization procedure. A 3.5-mm cannulated screw with a washer or a 3.0-mm headless compression screw was used for coracoid process fixation, and either a clavicle hook plate or Kirschner (K)-wires were used for ACJ injuries when additional fixation was necessary.
Results
Bone union was achieved in 11 patients (91.7%), while one case was determined to be a nonunion at 6 months. Radiological union occurred at an average of 3 months (range, 1.5–4 months) in all patients except the nonunion case. At the final follow-up, the average clinical scores were a visual analogue scale (VAS) pain score of 1.5 (range, 0–4) and a UCLA score of 30.9 (range, 28–35). Clinical outcomes were satisfactory in all patients, including the patient with nonunion.
Conclusion
The clinical and radiological outcomes of treating coracoid process fractures associated with ACJ injuries using coracoid process fixation with or without ACJ stabilization were favorable. A cannulated screw with a washer and clavicle hook plate fixation may provide sufficient stability for both the coracoid process fracture and the ACJ injury when feasible. Level of evidence: IV.
- 182 View
- 6 Download

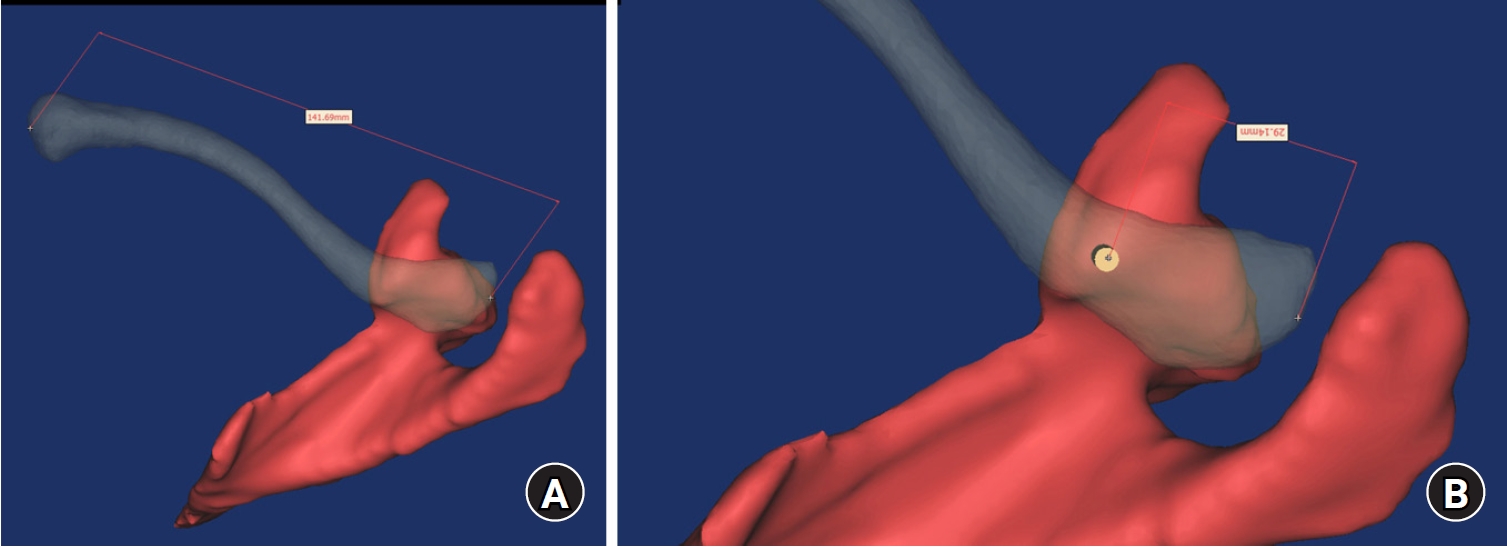
- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
-
 Abstract
Abstract
 PDF
PDF - Background
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 671 View
- 22 Download

Review Articles
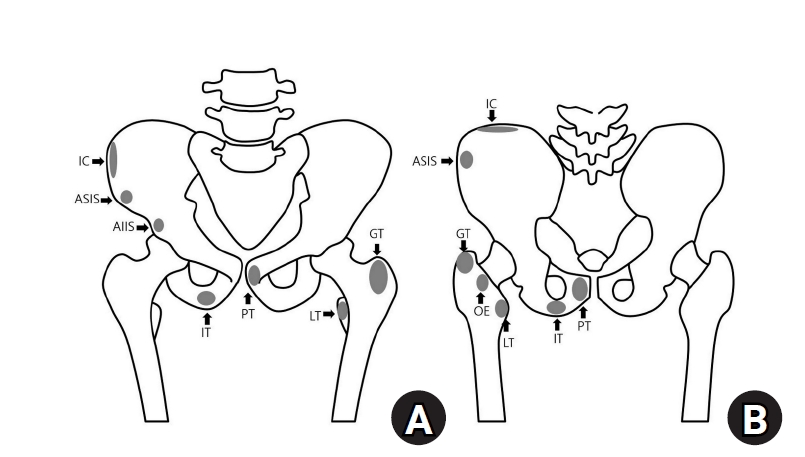
- Avulsion fractures around the hip joint and pelvis
- Won-Sik Choy, Yonghan Cha, Jung-Taek Kim, Jun-Il Yoo, Jin-Woo Kim
- J Musculoskelet Trauma 2025;38(2):53-62. Published online March 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00010
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures occur when tendons or ligaments are subjected to forces greater than they can withstand at the apophysis or enthesis, regardless of fusion status. The pelvis and hip joint are vulnerable to these injuries due to the diverse muscular structures in these structures, which serve as origins for multiple muscles leading to the lower extremities. Pelvic avulsion fractures commonly affect young athletes, but can also occur in adults. The diagnosis typically involves assessing trauma history, a clinical examination, and radiographic imaging. If the diagnosis is unclear, additional tests such as computed tomography and magnetic resonance imaging may assist in the diagnosis and provide useful information for treatment decisions. While most avulsion fractures respond well to conservative treatment, surgical intervention may be preferred in severe displacements, cases of significant retraction in active athletes, or when a faster recovery is necessary. Chronic or neglected injuries may lead to excessive osseous formation around the pelvis, causing impingement syndromes. Recognizing characteristic radiological findings based on pelvic anatomy helps to make an accurate diagnosis, as chronic injuries can mimic tumors or infectious conditions, necessitating a careful differential diagnosis.
-
Citations
Citations to this article as recorded by- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
Dawid Bartosik, Bartlomiej Cwikla, Anna Kowalczyk, Michalina Loson-Kawalec, Anna Palka-Szymaniec, Bartosz Starzynski, Alina Keska, Jakub Szkuta, Klaudia Wojcik
Cureus.2026;[Epub] CrossRef
- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
- 9,162 View
- 137 Download
- 1 Crossref

- Easily missed nondisplaced fractures accompanying complete fractures in the lower extremity and pelvis: a narrative review
- Young-Chang Park
- J Musculoskelet Trauma 2025;38(1):5-12. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00017
-
 Abstract
Abstract
 PDF
PDF - Nondisplaced fractures accompanying complete fractures are often difficult to detect on plain radiographs or computed tomography scans, posing a diagnostic challenge. The diagnosis of these frequently overlooked injuries can be delayed, potentially leading to suboptimal patient outcomes. This review discusses four commonly missed fracture patterns in the lower extremity and pelvis, including posterior involvement in fragility fractures of the pelvis, intertrochanteric extensions in isolated greater trochanter fractures, ipsilateral femoral neck fractures in high energy femoral shaft fractures, and posterior malleolar fractures in distal spiral tibial shaft fractures. An accurate diagnosis of these accompanying nondisplaced fractures is critical for optimizing surgical outcomes. Surgeons should incorporate thorough preoperative evaluations into their clinical practice to facilitate early detection and appropriate treatment strategies. Prompt identification and comprehensive management remain essential for improving patient outcomes.
- 1,376 View
- 47 Download

Original Article
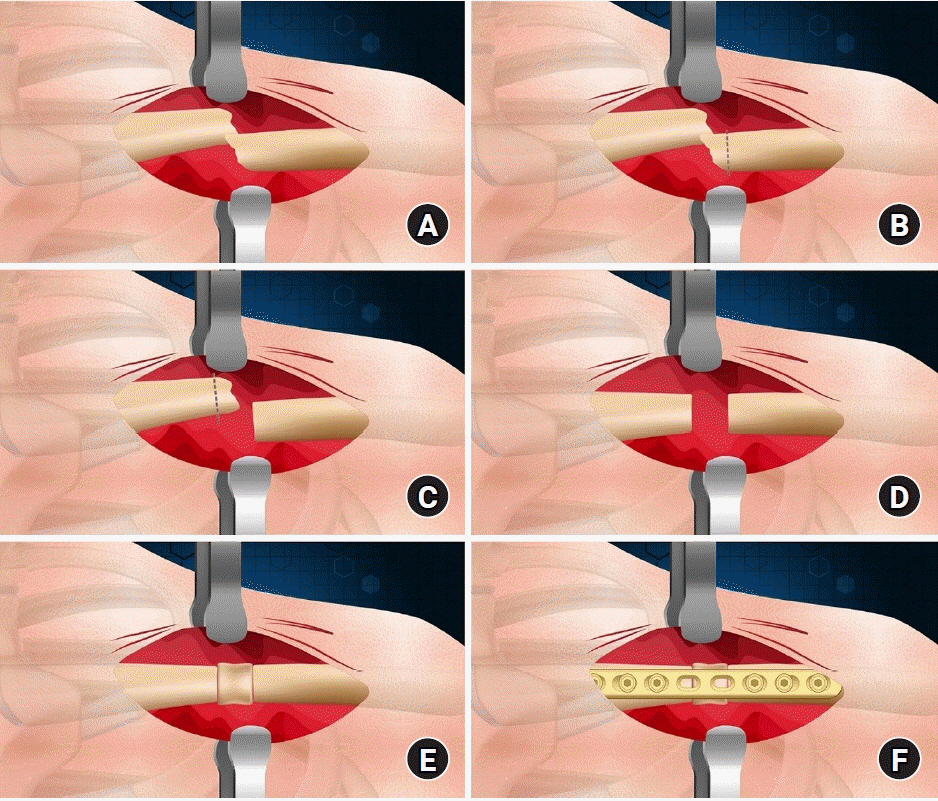
- Interpositional tricortical iliac bone graft in nonunion of midshaft clavicular fractures
- Eun-Seok Son, Bum-Soon Park, Chang-Jin Yon, Chul-Hyun Cho
- J Musculoskelet Trauma 2025;38(1):23-31. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00004
-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to investigate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures. Methods: Between 2007 and 2020, 17 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion combined with bone defect were investigated. The mean age was 53 years (range, 22–70 years). The mean follow-up period was 102.2 months (range, 18–193 months). Serial plain radiographs were used to evaluate radiological outcomes. The University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate clinical outcomes. Complications were also evaluated. Results: All cases achieved complete bony union with mean healing time of 17.6 weeks (range, 14–22 weeks). The mean clavicle length difference was significantly decreased from 9.1 mm preoperatively to 2.6 mm postoperatively (P<0.001). The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001), respectively. The mean final Quick-DASH score was 18.0. Three cases (17.6%) developed postoperative complications including two cases of shoulder stiffness and one case of screw irritation. Conclusions: Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length. Level of evidence: Level IV, case series.
- 2,026 View
- 44 Download

Review Articles
- Avulsion Fractures around the Hip Joint and Pelvis
- Ha-Yong Kim, Hajun Jang, Jung-Taek Kim, Jin-Woo Kim, Jun-Il Yoo, Won-Sik Choy, Yonghan Cha
- J Korean Fract Soc 2024;37(3):150-157. Published online July 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.3.150
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures occur when tendons or ligaments are subjected to forces greater than they can withstand at the apophysis or enthesis, regardless of the fusion status. Given the diverse muscular structures around the pelvis and hip joint, which serve as origins for multiple muscles leading to the lower extremities, these areas are vulnerable to such injuries. Pelvic avulsion fractures commonly af-fect young athletes, but they can also occur in adults. Diagnosis typically involves assessing the trauma history, clinical examination, and radiographic imaging. In cases of unclear diagnosis, additional tests, such as computed tomography or magnetic resonance imaging, may assist in treatment decisions and diagnosis. Although most avulsion fractures respond well to conservative treatment, surgical interven-tion may be preferred in severe displacements, significant retraction in active athletes, or when a faster recovery is necessary. Chronic or neglected injuries may lead to excessive osseous formation around the pelvis, causing impingement syndromes. Recognizing the characteristic radiological findings based on the pelvic anatomy aids in accurate diagnosis because chronic injuries might mimic tumors or infectious conditions, necessitating a careful differential diagnosis.
- 1,537 View
- 45 Download

- Avulsion Fractures in the Ankle and Foot
- Gyeong Hoon Lim, Jae Won Kim, Sung Hyun Lee
- J Korean Fract Soc 2024;37(2):102-116. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.102
-
 Abstract
Abstract
 PDF
PDF - An avulsion fracture occurs when a muscle-tendon unit attached to a bone produces sufficient force to tear a fragment of the bone. If not treated properly, this injury can lead to deformity, nonunion, malunion, pain, and disability. Although avulsion fractures around the foot and ankle can occur anywhere there are tendon and ligament attachments, they are common in the anterior talofibular ligament, anterior-inferior tibiotalar ligament, calcaneal tuberosity, the base of the fifth metatarsal, and navicular bone. The optimal treatment for each fracture depends on the location and severity of the fracture. Conservative treatment involves limiting weight bearing for a period, splint immobilization, and using various orthoses. Surgical treatment is usually reserved for cases of severe displacement or when nonsurgical treatment has failed. The goals of surgery include reduction of the fracture fragment, prevention of nonunion or malunion and soft tissue injury, and early return to function. The decision for each treatment modality may depend on the patient demographics or preferences and the surgeon experience. This review summarizes previous and current views on the pathogenesis, diagnosis, and treatment of common avulsion fractures to guide the treatment and diagnosis.
- 2,097 View
- 48 Download

Original Article
- Cephalomedullary Nailing with an Additional Cannulated Screw Fixation in Basicervical Femur Fractures
- Keong-Hwan Kim, Woo Dong Nam, Yeon Sik Heo, Gu-Hee Jung
- J Korean Fract Soc 2024;37(1):22-29. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.22
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study is to analyze the clinical results of patients with basicervical fracture undergoing cephalomedullary nailing (CMN) with an additional cannulated screw fixation compared to only performing CMN. We hypothesized that a difference may exist in the clinical outcomes if an ad-ditional screw is fixed with CMN compared to only performing CMN in basicervical fracture.
Materials and Methods
A total of 28 consecutive patients who underwent CMN for basicervical fracture were included. In 9 cases, only CMN was conducted, and in 19 cases, an additional cannulated screw fixation was performed with CMN. Bone union, sliding distance, reduction status, and fixation failure were evaluated by postoperative radiography, and ambulatory ability was evaluated by functional results. These findings were compared between a group of CMN and a group of CMN with an additional cannulated screw.
Results
There were 4 males and 24 females with a mean age of 84 years (range, 69–100 years). No significant difference was found in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5–13.4 mm] vs 3.5 mm [range, 0.1– 9.2 mm]; p=0.045). Among the two groups, only one case of fixation failure at the postoperative four months was observed in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
- 1,273 View
- 14 Download

Review Articles
- Fragility Fractures of the Pelvis and Sacrum
- Se-Won Lee, Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):29-38. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.29
-
 Abstract
Abstract
 PDF
PDF - The incidence of fragility fractures of the pelvis (FFP) has increased significantly due to the aging popu-lation and improved diagnostic modalities. The evaluation and treatment of these patients differ from that of high-energy pelvic ring injuries typically seen in younger patients. Therefore, it is important to classify the FFP by patterns of the classification system to standardize optimal treatment criteria and appropriate treatment strategy. However, some cases are not classifiable according to the FFP classifi-cation. A newly proposed classification that can be verified by comparing existing FFP classifications is needed to overcome the weak points. Non-operative treatment is usually considered first and should focus on early mobilization. Operative fixation should focus on stabilizing the minimally invasive pelvic ring than the reduction of fractures to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility.
- 1,908 View
- 33 Download

- Current Concepts of Vitamin D and Calcium in the Healing of Fractures
- Jihyo Hwang
- J Korean Fract Soc 2021;34(3):117-121. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.117
-
 Abstract
Abstract
 PDF
PDF - Fragile fractures, also known as osteoporosis fractures, insufficiency fractures, and senile fractures are a significant problem encountered by orthopedic surgeons. Calcium and vitamin D are essential for maintaining bone health and deficiencies in calcium and vitamin D are major risk factors for the development of osteoporosis. Sufficient amounts of calcium are also required for fracture-callus mineralization. Hence, compromised bone repair that is frequently observed in osteoporotic patients might be attributed to calcium and vitamin D deficiencies. Consequently, calcium and vitamin D supplementation represents a potential strategy for treating compromised fracture healing in osteoporotic patients. There is some clinical evidence of the positive effect of supplementation in fracture healing and posttraumatic bone turnover, but research in this area is ongoing. Calcium and vitamin D should be the primary treatment of choice in osteopenic patients with an insufficiency of calcium and vitamin D and for the prevention of secondary osteoporotic fractures. Calcium and vitamin D can also be used as addition to other primary osteoporotic medications such as antiresorptive or bone-forming agents. The role of calcium and vitamin D in fracture healing and the therapeutic potential of calcium and vitamin D supplementation is summarized in this context.
- 6,902 View
- 81 Download

Case Reports
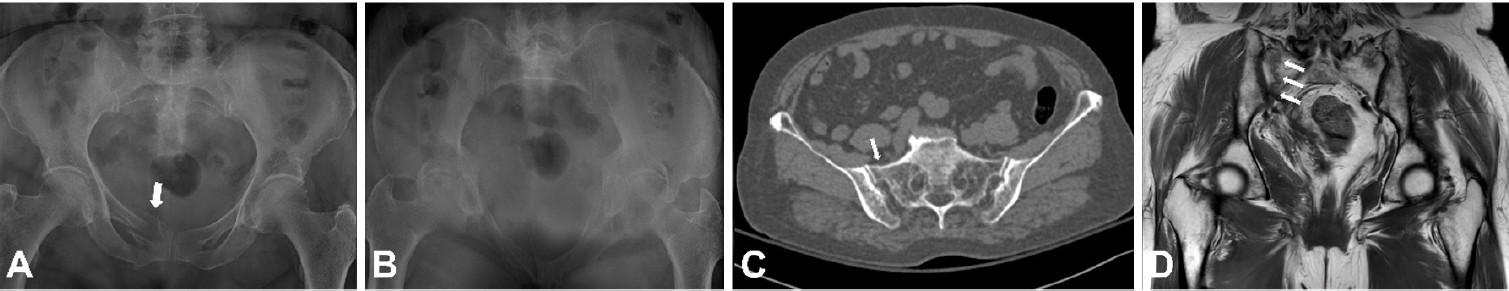
- Latent Superior Gluteal Artery Injury by Entrapment between the Fragments in Transverse Acetabular Fracture - A Case Report -
- Hyuk Jin Choi, Byung Chul Kim, Hoon Kwon, Jae Hoon Jang
- J Korean Fract Soc 2021;34(1):30-33. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.30
-
 Abstract
Abstract
 PDF
PDF - The superior gluteal artery is branched from the internal iliac artery and is located outside the pelvis through a greater sciatic notch. This anatomical characteristic makes the artery vulnerable to injury when pelvic fracture involves the sciatic notch. In the case of a superior gluteal artery injury, hemodynamic instability can occur, and appropriate evaluation and management are mandatory in the acute phase. On the other hand, if the initial detection of the injury is neglected due to a masked pattern, it can cause massive bleeding during surgery, resulting in difficult hemostasis. This paper reports an experience of a latent superior gluteal artery injury by entrapment between the fragments of a transverse acetabular fracture.
-
Citations
Citations to this article as recorded by- Superior gluteal artery injury in pelvic ring injury and acetabular fracture: Single center observational study
Hoon Kwon, Jae Hoon Jang, Nam Hoon Moon, Seung Joon Rhee, Dong Yeon Ryu, Tae Young Ahn
Journal of Orthopaedic Science.2024; 29(6): 1483. CrossRef
- Superior gluteal artery injury in pelvic ring injury and acetabular fracture: Single center observational study
- 770 View
- 5 Download
- 1 Crossref

- Sclerotherapy Using Abnobaviscum for the Extensive Recurrent Chronic Morel-Lavallée Lesions - A Case Report -
- Joon-Kuk Kim, Ji-Won Jung, Ki-Chul Park
- J Korean Fract Soc 2020;33(4):222-226. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.222
-
 Abstract
Abstract
 PDF
PDF - The Morel-Lavallée lesion (MLL) is a closed soft-tissue degloving injury, resulting in characteristic hemo-lymphatic fluid collection between the fascia and subcutaneous layers. The MLL was managed routinely with drainage and compression bandages, but sclerotherapy can be used in patients with chronic lesions refractory to first-line therapy. This paper presents a case of extensive recurrent chronic MLL treated with sclerotherapy using Abnobaviscum, which has been used to treat adhesion in malignant pleural effusion.
-
Citations
Citations to this article as recorded by- Seroma prevention with topical Abnobaviscum sclerotherapy following excision of giant cervical lipoma
Jun Ho Choi, Seung Yeon Choi, Jae Ha Hwang, Kwang Seog Kim, Sam Yong Lee
Archives of Craniofacial Surgery.2023; 24(1): 10. CrossRef
- Seroma prevention with topical Abnobaviscum sclerotherapy following excision of giant cervical lipoma
- 752 View
- 10 Download
- 1 Crossref

- Brachial Plexus Neuropathy after Revision of Clavicular Fracture Nonunion: A Case Report
- Youngwoo Kim, Suk Kyu Choo, Neunghan Jeon
- J Korean Fract Soc 2020;33(1):22-26. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.22
-
 Abstract
Abstract
 PDF
PDF - We performed a revisionary open reduction and internal fixation for treating nonunion of the mid-shaft of the left clavicle with an autogenous cancellous bone graft. On postoperative day 4, the patient presented with neurologic deficits in the left upper extremity. We removed the implant and made a superior angulation to decompress the brachial plexus. At 6 months postoperatively, callus bridging and consolidation were visible and all hand and elbow functions were fully recovered. Our case suggests that brachial plexus neuropathy may be caused by stretching and compression after reduction and straightening of the nonunion site around adhesions or scar tissue. Therefore, care should be taken whether there are the risk factors that can cause brachial plexus neuropathy when revision surgery is performed for treating nonunion of a clavicle shaft fracture.
-
Citations
Citations to this article as recorded by- Arcuate osteoplasty for brachial plexus paralysis after plate fixation of mid-clavicle fracture: a case report and literature review
Dongju Shin, Jae Hwi Han
Clinics in Shoulder and Elbow.2025; 28(3): 394. CrossRef
- Arcuate osteoplasty for brachial plexus paralysis after plate fixation of mid-clavicle fracture: a case report and literature review
- 1,141 View
- 1 Download
- 1 Crossref

Review Article
- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- Dong Hee Kim, Jae Hoon Jang, Myungji Shin, Gu Hee Jung
- J Korean Fract Soc 2019;32(4):240-247. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.240
-
 Abstract
Abstract
 PDF
PDF - The fixation methods that can be used for unstable posterior pelvic ring injuries have undergone many innovative changes due to the recent development of surgical and imaging techniques. After understanding the appropriate indications of first and second sacroiliac screw fixation and spinopelvic fixation, innovative methods, including the trans-sacral screw fixation, posterior tension-band plate fixation, and the S2AI screw, would be chosen and applied. Considering the anatomical complexity and proximity to the surrounding vessels and nerves in the posterior fixation, the safe zone according to the fixation options should be well understood in preoperative planning. Moreover, the functional reduction of the posterior pelvic ring through the reduction and fixation of the anterior lesion should be achieved before placing the implant to reduce the number of malposition-related complications.
-
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 1,072 View
- 13 Download
- 1 Crossref

Case Report
- Progressive Brachial Plexus Palsy after Fixation of Clavicle Shaft Nonunion: A Case Report
- Hong Ki Jin, Ki Bong Park, Hyung Lae Cho, Jung Il Kang, Wan Seok Lee
- J Korean Fract Soc 2019;32(2):97-101. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.97
-
 Abstract
Abstract
 PDF
PDF - The brachial plexus palsy is a rare complication of a clavicle fracture, occurring in 0.5% to 9.0% of cases. This condition is caused by excessive callus formation, which can be recovered by a spur resection and surgical fixation. In contrast, only seven cases have been reported after surgical reduction and fixation. A case of progressive brachial plexus palsy was observed after fixation of the displaced nonunion of a clavicle fracture. The symptom were improved after removing the implant.
-
Citations
Citations to this article as recorded by- Arcuate osteoplasty for brachial plexus paralysis after plate fixation of mid-clavicle fracture: a case report and literature review
Dongju Shin, Jae Hwi Han
Clinics in Shoulder and Elbow.2025; 28(3): 394. CrossRef
- Arcuate osteoplasty for brachial plexus paralysis after plate fixation of mid-clavicle fracture: a case report and literature review
- 805 View
- 6 Download
- 1 Crossref

Original Article
- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
- So Young Kim
- J Korean Fract Soc 2019;32(2):89-96. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.89
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This paper reviewed the safety and effectiveness of anchor augmentation with bone cement in osteoporotic femoral fractures.
MATERIALS AND METHODS
A systematic review was conducted by searching multiple databases including five Korean databases, Ovid-MEDLINE, Ovid-EMBASE, and Cochrane Library. Safety was assessed through the incidence of complication. The effectiveness was assessed through the failure rate of anchor fixation, improvement of function and radiological assessment (sliding distance of lag screw and cutout). The safety and effectiveness of anchor augmentation with bone cement were assessed by reviewing all articles reporting on the treatment. Two researchers carried out independently each stage from the literature search to data extraction. The tools of Scottish Intercollegiate Guidelines Networks were used to assess the quality of studies.
RESULTS
Six studies were considered eligible. The safety results revealed a small amount of cement leakage (1 case), but no other severe complications were encountered. Regarding the effectiveness, the failure rate of anchor fixation was 16.7% and the Harris's hip score showed no significant improvement. The sliding distance of the anchor was similar in the cement augmentation group and non-cement group but there was no cutout.
CONCLUSION
The results of the assessment suggest that the safety is acceptable, but further research will be needed to verify the effectiveness of the treatment.
- 719 View
- 5 Download

Case Report
- Bilateral Gluteal Necrosis and Deep Infection after Transarterial Embolization for Pelvic Ring Injury in Patient with Hemodynamic Instability: A Case Report
- Sung Jin Park, Chang Ho Jeon, Nam Hoon Moon, Yong Geon Park, Jae Hoon Jang
- J Korean Fract Soc 2019;32(1):56-60. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.56
-
 Abstract
Abstract
 PDF
PDF - Transarterial embolization is accepted as effective and safe for the acute management in hemodynamically unstable patients with pelvic ring injury. However, transarterial embolization has potential complications, such as gluteal muscle/skin necrosis, deep infection, surgical wound breakdown, and internal organ infarction, which are caused by blocked blood flow to surrounding tissues and organs, and many studies on the complications have been reported. Here, we report an experience of the management of gluteal necrosis and infection that occurred after transarterial embolization, with a review of the relevant literature.
- 836 View
- 0 Download

Original Article
- Surgical Results of Minimally Invasive Percutaneous Plate Fixation in the Treatment of Clavicle Shaft Fracture
- Seong Ho Yoo, Suk Woong Kang, Jae Seung Seo
- J Korean Fract Soc 2019;32(1):21-26. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.21
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study analyzed the results of the midclavicle fracture treatment using the minimally invasive percutaneous plate osteosynthesis (MIPO) technique in a retrospective manner.
MATERIALS AND METHODS
Between March 2013 and March 2017, this study analyzed 40 patients who received MIPO surgery. Excluding 1 patient who underwent surgery on another body part injury, and 4 patients who were lost to follow-up over 1 year, 40 patients were analyzed for their operation time, bone union, functional American Shoulder and Elbow Surgeons score, scar lengths, pain relief (visual analogue scale), and complications.
RESULTS
All patients over a 1 year of follow-up achieved bone union, and American Shoulder and Elbow Surgeons score 97.6 (94–100) on their shoulder functional scores. Their average operation time was 42.7 minutes, and the average scar length was 6.1 cm. Eighteen patients successfully received metal removal using the previous scar without additional incision. The clavicle length was similar in the normal and operated group.
CONCLUSION
Despite its small sample size, clavicle fixation using the MIPO technique can be considered an effective treatment because of its limited number of complications, such as nonunion and rotational angulations. -
Citations
Citations to this article as recorded by- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
Woo Jin shin, Young Woo Chung, Seon Do Kim, Ki-Yong An
Clinics in Shoulder and Elbow.2020; 23(4): 205. CrossRef
- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
- 1,029 View
- 1 Download
- 1 Crossref

Case Report
- Spino-Pelvic Fixation in Unstable Sacral Fracture: A Case Report
- Jung Hwan Choi, Kyu Tae Hwang, Seung Gun Lee, Chang Nam Kang
- J Korean Fract Soc 2018;31(4):145-148. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.145
-
 Abstract
Abstract
 PDF
PDF - A 22-year-old female patient visited the emergency room (ER) after a pedestrian traffic accident in a drunken state. An examination at the ER revealed fractures at the right side of the sacral ala, sacral foramina, left anterior acetabulum, right inferior ramus, and right superior articular process of S1. She underwent spino-pelvic fixation and iliosacral (IS) screw fixation. One year later, bone union was completed and implant removal was performed and the treatment was completed without complications. The authors recommend spino-pelvic fixation and IS screw fixation for unstable sacral fractures as one of the excellent methods for obtaining posterior stability of the pelvis among the various treatments of unstable sacral fractures.
- 346 View
- 1 Download

Review Article
- Pelvis/Acetabular Fractures in the Elderly: When and How to Fix?
- Kyeong Hyeon Park, Chang Wug Oh, Joon Woo Kim
- J Korean Fract Soc 2018;31(3):102-113. Published online July 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.3.102
-
 Abstract
Abstract
 PDF
PDF - Owing to the increase in life expectancy, the incidence of osteoporotic fracture of the pelvis and acetabulum is increasing. Fractures in the elderly population is different from those in younger patients. Pelvic ring and acetabular fractures in geriatric patients are more likely the result of low-energy trauma, but the outcomes are generally poorer than those of the younger population. Multiple management options are available, but no intervention has become the standard of care for these fractures in the elderly. A treatment strategy should be established depending on the state of the individual patient. Regardless of whether nonsurgical or surgical treatment is selected, early ambulation should be considered to avoid the complications associated with prolonged immobilization.
-
Citations
Citations to this article as recorded by- Effect of Korean Medicine Treatments for Pain Reduction in Patients with Hip Fracture : A Retrospective Observational Study
Nam Hoon Kim, Min Seok Oh
Journal of Physiology & Pathology in Korean Medicine.2020; 34(5): 263. CrossRef
- Effect of Korean Medicine Treatments for Pain Reduction in Patients with Hip Fracture : A Retrospective Observational Study
- 529 View
- 6 Download
- 1 Crossref

Case Report
- Clay-Shoveler's Fracture in an 18-Year-Old Cheerleader: A Case Report
- Il Yeong Hwang, Sun Jae Park, Jae Ryong Cha
- J Korean Fract Soc 2018;31(2):57-60. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.57
-
 Abstract
Abstract
 PDF
PDF - Clay-Shoveler's fracture refers to a fracture that is solely developed on the spinous process of the cervical spine or the thoracic vertebrae. This fracture rarely occurs during sporting activities. In this case, an 18-year-old female developed the fracture on the spinous process of the 7th cervical spine and 1st thoracic vertebrae due to the repetitive practice of cheerleading. The patient's pain was improved by wearing a support device and taking an anti-inflammatory analgesic drug and muscle relaxant. Her case is being followed-up at the outpatient department.
-
Citations
Citations to this article as recorded by- Clay-Shoveler’s Fracture on the Baseball Diamond: A Case of Noncontact Thoracic Spine Pain in an Adolescent Athlete
Jason S. Silver, Jordan Bork, Charles D. Kenyon
Current Sports Medicine Reports.2025; 24(6): 140. CrossRef - An unusual cause of neck pain in the physiotherapy clinic: Neglected clay-shoveler's fracture
GaneshSingh Dharmshaktu
Indian Journal of Physical Therapy and Research.2020; 2(2): 147. CrossRef
- Clay-Shoveler’s Fracture on the Baseball Diamond: A Case of Noncontact Thoracic Spine Pain in an Adolescent Athlete
- 1,127 View
- 2 Download
- 2 Crossref

Original Article
- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
- Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
- J Korean Fract Soc 2018;31(1):9-17. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.9
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Iliosacral screw fixation is an effective and less invasive method that is used widely for the definitive treatment of unstable pelvic ring injuries. On the other hand, fixation failures after iliosacral screw fixation have been reported in vertically unstable pelvic ring injuries. This study examined the surgical outcomes of posterior pelvic fixation using S1 and S2 screws in vertically unstable pelvic ring injuries.
MATERIALS AND METHODS
Between January 2011 and April 2016, 17 patients with vertically unstable pelvic ring injuries who met the minimum 1 year follow-up criteria were treated with internal fixation using posterior pelvic S1 and S2 screws. Their mean age was 43.9 years. According to the AO/OTA classification, 10 patients had C1, 6 had C2, and 1 had C3 injuries. Surgical treatments of single or multiple steps, where necessary, were performed by two surgeons. The clinical and radiologic outcomes were assessed retrospectively using radiographs and medical records.
RESULTS
Overall, 16 patients had bone healing without screw loosening; however, one patient could not maintain anterior pelvic fixation because of an open fracture and deep infection in the anterior pelvic ring. Of five patients who complained of neurological symptoms after injury, three had partially recovered from their neurological deficit. At the last follow-up, the clinical outcomes according to the Majeed score were excellent in 5, good in 6, fair in 4, and poor in 2 patients. The postoperative radiologic outcomes by Matta and Tornetta's method were excellent in 5, good in 8, and fair in 4 patients. Malposition of the S2 screw was identified in one case. The mean time to union was 14.6 weeks after surgery.
CONCLUSION
S1 and S2 screw fixation can be an effective treatment option for posterior pelvic stabilization in vertically unstable pelvic ring injuries when considering the surgical outcomes, such as screw loosening and loss of reduction. -
Citations
Citations to this article as recorded by- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
Dong-Hee Kim, Jae Hoon Jang, Myungji Shin, Gu-Hee Jung
Journal of the Korean Fracture Society.2019; 32(4): 240. CrossRef
- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- 559 View
- 3 Download
- 1 Crossref

Review Article
- Conservative Treatment of Mid-Clavicle Fractures
- Woong Kyo Jeong
- J Korean Fract Soc 2018;31(1):22-28. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.22
-
 Abstract
Abstract
 PDF
PDF - Clavicle fractures are very common injuries in adults and children and the majority of these fractures occur in the midshaft. Traditionally, mid-clavicle fractures have been treated with conservative methods and the clinical outcomes of this method are believed to be excellent. On the other hand, recent studies have shown that the clinical results of severe comminuted or markedly displaced fractures after conservative management were not as favorable as previously described. Despite these concerns, the conservative treatment of mid-clavicle fractures is still an efficient method, which can be applied to all patients as a primary care. This review focuses on the proper indication, technique, and limitations of conservative treatment of mid-clavicle fractures.
-
Citations
Citations to this article as recorded by- Two Patients Who Were Hospitalized for Clavicle Fracture Caused by a Traffic Accident and Improved with Korean Medicine Complex Treatment
Deok Kang, ByungSoo Kang, Hwe-Joon Jeong, Dong-Hoon Shin, Kyung-Moon Shin, Ji-Hoon O, Jae-Woo Yang
Journal of Korean Medicine Rehabilitation.2022; 32(3): 179. CrossRef
- Two Patients Who Were Hospitalized for Clavicle Fracture Caused by a Traffic Accident and Improved with Korean Medicine Complex Treatment
- 503 View
- 2 Download
- 1 Crossref

Case Reports
- Atypical Bipolar Segmental Fracture of the Clavicle in an Adolescent: A Case Report
- Joong Bae Seo, Sung Hyun Yoon, Jun Kyom Kim, Sung Hyun Kim, Jae Sung Yoo
- J Korean Fract Soc 2018;31(1):18-21. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.18
-
 Abstract
Abstract
 PDF
PDF - Clavicular fractures commonly occur in adults and children. The usual site of these fractures is the mid clavicle with lateral end and medial end clavicular fractures being less common. Bipolar segmental clavicular injuries involving medial and lateral ends are rare but almost always occur in adults. This paper reports a very rare case of segmental clavicular fracture involving the medial and lateral end in an adolescent caused by direct trauma. The surgical management of a segmental fracture clavicle in an adolescent is reported with a discussion of the relevant literature.
- 308 View
- 3 Download

- Intrapelvic Penetration of Lag Screw in Proximal Femoral Nailing: A Case Report
- Jung Woo Lee, Hong Man Cho, Jae Woong Seo
- J Korean Fract Soc 2017;30(4):203-208. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.203
-
 Abstract
Abstract
 PDF
PDF - Hip fractures are common among elderly individuals. Internal fixation with the intramedullary system has been widely used to treat intertrochanteric femur fractures. The Gamma 3 nail is a useful device for fixating trochanteric fractures of the proximal femur. We report a rare complication of medial pelvic penetration of the lag screw of a Gamma 3 nail two months after surgery. There was a complete separation between the nail body and lag screw, and the lag screw penetrated through the acetabulum into the pelvis. We report a case of unstable intertrochanteric fracture with intrapelvic penetration after surgical treatment with proximal femoral nailing and a case followed by fatal results.
-
Citations
Citations to this article as recorded by- Medial lag screw migration in an intramedullary nail combination
Zac Dragan, Ryan J Campbell, Terence R Moopanar
BMJ Case Reports.2025; 18(3): e262436. CrossRef - Slipped hip acetabular cortical screw: Laparoscopy to the rescue
Nidhi Paswan, Lovenish Bains, Soukat Ali Khan, Anubhav Vindal, Lalit Maini
Journal of Minimal Access Surgery.2025;[Epub] CrossRef - Endovascular assisted removal of intrapelvic lag screw after intramedullary proximal femoral nail: A case report and literature review
Zakaria Mousati, Mathias Van Den Broek, Joren Callaert, Jan Gielis, Kris Govaers
Trauma Case Reports.2023; 46: 100873. CrossRef - Intrapelvic migration of the lag screw in intramedullary nailing after intertrochanteric fracture fixation: A case report
Aymen Ben Fredj, Hedi Rbai, Fourat Farhat, Marouen Berriri
Clinical Case Reports.2022;[Epub] CrossRef - Intramedullary nailing confers an increased risk of medial migration compared to dynamic hip screw fixation in unstable intertrochanteric hip fractures
Gin Way LAW, Yoke Rung WONG, Antony GARDNER, Yau Hong NG
Injury.2021; 52(11): 3440. CrossRef - Medial migration in cephalomedullary nail fixation of pertrochanteric hip fractures
G. W. Law, Y. R. Wong, A. K-S. Yew, A. C. T. Choh, J. S. B. Koh, T. S. Howe
Bone & Joint Research.2019; 8(7): 313. CrossRef - Intrapelvic Migration of the Lag Screw with Wedge Wing from Dyna Locking Trochanteric Nail: A Case Report and Literature Review
Yong-Woo Kim, Weon-Yoo Kim, Kyong-Jun Kim, Se-Won Lee
Hip & Pelvis.2019; 31(2): 110. CrossRef
- Medial lag screw migration in an intramedullary nail combination
- 1,460 View
- 16 Download
- 7 Crossref

Original Article
- Clinical Features and Outcomes of Pelvic Insufficiency Fractures
- Yong Min Seo, Young Chang Kim, Ji Wan Kim
- J Korean Fract Soc 2017;30(4):186-191. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.186
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to investigate the radiological and epidemiological characteristics, as well as the clinical course of pelvic insufficiency fractures in the elderly population.
MATERIALS AND METHODS
At a Haeundae Paik Hospital, we retrospectively reviewed patients with pelvic insufficiency fractures between March 2010 and May 2017. The demographic data of patients were analyzed, and bone mineral density and bone turnover markers were evaluated to estimate the metabolic status of the bone. The radiological characteristics were evaluated by comparing the simple x-ray images with the computed tomography images, and the types of fractures were classified via computed tomography images. For clinical course evaluation, we investigated comorbid complications, and compared the walking ability scale before and 6 months after the fracture.
RESULTS
A total of 42 patients were included, with an average age of 76.5 years. All were female except one case. In 5 cases where the initial medical examination was from another institution, the fracture was not found in 3 cases. All cases received conservative treatment. After the diagnosis of pelvic bone fracture using a simple x-ray imaging, additional fractures were found in 81.0% of the study population using a computed tomography. Initiation of gait occurred at an average of 2.8 weeks, and every case except 1 (97.6%) fully recovered their gait ability.
CONCLUSION
We concluded that there was a limitation with diagnosing pelvic insufficiency fracture using only a simple x-ray imaging technique. In general, cases in this study showed conservative treatment yielded favorable clinical outcome with relatively less critical complications.
- 587 View
- 1 Download

Case Report
- The Different Treatment Methods for Segmental Fractures of the Clavicle: Cases Report
- Sung Sik Ha, Ki Do Hong, Jae Cheon Sim, Yi Rak Seo, Tae Seok Nam
- J Korean Fract Soc 2017;30(3):151-155. Published online July 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.3.151
-
 Abstract
Abstract
 PDF
PDF - Segmental fractures of the clavicle are very rare. Therefore, to date, there has not been a clear, standardized method of management of segmental clavicle fractures. Herein, two patients with a segmental fracture are described: One patient was treated conservatively, while another patient was treated operatively. Both patients showed excellent results. We discuss the various management options with a literature review.
-
Citations
Citations to this article as recorded by- Fratura segmentar da clavícula em paciente politraumatizado: Relato de caso
Carlos A. Sánchez, Pablo J. Coronel, Luisa F. García, Juan S. Afanador, Raúl Gonzalez
Revista Brasileira de Ortopedia.2024; 59(01): e139. CrossRef
- Fratura segmentar da clavícula em paciente politraumatizado: Relato de caso
- 1,010 View
- 3 Download
- 1 Crossref

Original Articles
- Sexual Activity at 1 Year after Acetabular Fracture
- Chan Ho Park, Young Kyun Lee, Kyung Hoi Koo
- J Korean Fract Soc 2017;30(3):111-116. Published online July 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.3.111
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Change in sexual activity after acetabular fracture has not been elucidated to date. Hence, the purpose of this study was to reveal: (1) how acetabular fracture affects the status of sexual activity; (2) how acetabular fracture affects patient satisfaction about sexual activity; and (3) what are the concerns of patients regarding sexual activity.
MATERIALS AND METHODS
Between January 2014 and December 2014, a self-reported questionnaire was conducted with patients who had been sexually active before the treatment for acetabular fracture. Out of the nineteen patients who participated in the questionnaire, twelve men and three women were included for final analysis; patients who were treated conservatively were excluded.
RESULTS
All patients had hip pain (mean visual analogue scale score, 2.9; range, 1-7) at 1 year after the trauma. Fourteen patients (93.3%, 14/15) resumed sexual activity within 1 year (mean, 3.9 months; range, 2–6 months). After excluding one patient who did not recover to allow sexual activity, the frequency of sex was decreased in 11 patients (78.6%, 11/14). Sexual satisfaction was decreased in seven patients (46.7%, 7/15). Old age was associated with decreased sexual satisfaction.
CONCLUSION
Half of the patients showed a decreased satisfaction from sexual activity after acetabular fracture, with hip pain being the most common problem. Although our study was a small, single-center study, it provides information regarding sexual activity of patients after acetabular fracture. -
Citations
Citations to this article as recorded by- Sexual and Urinary Dysfunction Following Isolated Acetabulum Fractures: A Systematic Review of the Literature
Sophia M. Wakefield, Nikolaos K. Kanakaris, Peter V. Giannoudis
Journal of Clinical Medicine.2025; 14(1): 230. CrossRef - The Impact of Surgical Approaches for Isolated Acetabulum Fracture on Sexual Functions: A Prospective Study
Ibrahim Alper Yavuz, Can Aykanat, Cagdas Senel, Fatih Inci, Erman Ceyhan, Yılmaz Aslan, Altug Tuncel, Ahmet Ozgur Yildirim
Journal of Orthopaedic Trauma.2022; 36(3): 124. CrossRef
- Sexual and Urinary Dysfunction Following Isolated Acetabulum Fractures: A Systematic Review of the Literature
- 1,847 View
- 9 Download
- 2 Crossref

- A Comparison of Results between AO Hook Plate and TightRope for Acute Acromioclavicular Joint Dislocation
- Yong Gun Kim, Ho Jae Lee, Dong Won Kim, Jinmyoung Dan
- J Korean Fract Soc 2017;30(1):16-23. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.16
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of our study is to compare the radiographic and clinical outcomes with respect to acromioclavicular (AC) joint dislocation depending on the surgical method: Hook plate (HP) versus TightRope (TR).
MATERIALS AND METHODS
Between May 2009 and May 2012, 51 patients with Rockwood type III-V lesions received clinical and radiographic follow-up. Patients were divided into two groups according to the surgical methods (HP: n=32; TR: n=19). Radiological follow-up included comparative coracoclavicular distance (CCD) measurements as a percentage of the uninjured shoulder. For clinical follow-up, a standardized functional shoulder assessment with the Constant score, University of California at Los Angeles (UCLA) score, and Korea shoulder score (KSS) were carried out.
RESULTS
Comparing the functional results, no differences were observed between the two groups (Constant score: HP, 78.5; TP, 81.4; UCLA score: HP, 29.2; TP, 29.9; KSS: HP, 79.2; TP, 80.7). Time to restoration of the range of motion (ROM) above shoulder level was longer in the HP group than in the TR group. However, the ROM at 1 year postoperation and final follow-up revealed similar results between the two groups. The AC joints were well reduced in both groups, the CCD increased to 44.7% in the HP group and to 76.5% in the TR group at the final follow-up; however, no one was significantly superior to the others. Furthermore, there were 8 cases (25.0%) and 5 cases (26.3%) of AC joint arthritis in the HP group and TR group, respectively. However, the observed AC joint arthritis has a poor correlation between clinical symptom and radiological results in both groups.
CONCLUSION
Both HP and TR fixation could be a recommendable treatment option in acute unstable AC joint dislocation. Both groups showed excellent radiologic and functional results at the final visit. Moreover, there was no significant difference in statistics, except for the time to restoration of ROM above shoulder level. -
Citations
Citations to this article as recorded by- Suture-Button Fixation Outperforms Hook Plate in Functional Outcomes After Acromioclavicular Joint Dislocation
Murat Aşçı, Mete Gedikbaş
Bozok Tıp Dergisi.2025; 15(4): 477. CrossRef - Arthroscopic Treatment of Acromioclavicular Joint Dislocations
Du-Han Kim, Chul-Hyun Cho
Journal of the Korean Orthopaedic Association.2023; 58(5): 384. CrossRef - Combination of Clavicular Hook Plate with Coracoacromial Ligament Transposition in Treatment of Acromioclavicular Joint Dislocation
Aikebaier Tuxun, Ajimu Keremu, Pazila Aila, Maimaitiaili Abulikemu, Zengru Xie, Palati Ababokeli
Orthopaedic Surgery.2022; 14(3): 613. CrossRef
- Suture-Button Fixation Outperforms Hook Plate in Functional Outcomes After Acromioclavicular Joint Dislocation
- 2,375 View
- 6 Download
- 3 Crossref

Review Article
- Fractures of the Tarsal Bone
- Young Hwan Park, Hak Jun Kim, Soo Hyun Kim
- J Korean Fract Soc 2016;29(4):276-282. Published online October 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.4.276
-
 Abstract
Abstract
 PDF
PDF - Fractures of the tarsal bone, such as the navicular, cuboid, and cuneiform, are very rare. These injuries can lead to serious walking difficulties due to pain and deformity of the foot with delayed diagnosis of tarsal bone fractures during an injury to multiple lower extremities. The diagnosis can be done on simple radiographs. Sometime weight bearing radiographs or stress radiographs may be needed for further evaluation. Computed tomography is the most widely available diagnostic tool. Navicular and cuneiform account for the medial column of the foot, whereas cuboid for the lateral column. The treatment of tarsal bone fractures is primarily conservative management, but operative treatment is recommended for intra-articular displacement, dislocation, or shortening of the medial or lateral column of the foot. The operative treatments include screw fixation, plate fixation, or external fixation. Complications include malunion, nonunion, posttraumatic arthritis, avascular necrosis, and deformity of the foot. Tarsal bone fracture has to be evaluated carefully to prevent serious complications.
-
Citations
Citations to this article as recorded by- Effects of Acupuncture Treatment and Taping Therapy After Lisfranc Joint Injuries: A Case Report
Shin-Ae Kim, Su-Woo Kang, Eun-Ji Lee, Min-Kyung Kwak, Hui-Gyeong Jeong, Jae-Uk Sul
Journal of Acupuncture Research.2017; 34(4): 197. CrossRef
- Effects of Acupuncture Treatment and Taping Therapy After Lisfranc Joint Injuries: A Case Report
- 2,210 View
- 27 Download
- 1 Crossref

Original Articles
- Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
- Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
- J Korean Fract Soc 2016;29(3):185-191. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.185
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To introduce the technique of reducing displaced or comminuted clavicle shaft fracture using composite wiring and report the clinical results.
MATERIALS AND METHODS
Between March 2006 and December 2013, 31 consecutive displaced clavicle fractures (Edinburgh classification 2B) treated by anatomic reduction and internal fixation using composite wiring and plates were retrospectively evaluated. The fracture fragments were anatomically reduced and fixed with composite-wiring. An additional plate was applied. Radiographic assessments for the numbers of fragments, size of each fragment and amount of shortening and displacement were performed. The duration for fracture union and complications were investigated retrospectively. The mean fallow-up duration was 15.9 months.
RESULTS
The mean number of fragments was 1.7 (1-3) and the mean width of fracture fragment was 7.1 mm (4.5-10.6 mm). The mean shortening of the clavicle was 20.5 mm (10.3-36.2 mm). The mean number of composite wires used in fixation was 1.9 (1-3). Radiographic union was achieved in all patients with a mean time to union of 11.6 weeks. There were no complications including metal failure, pin migration, nonunion, or infection.
CONCLUSION
The composite wiring was suitable for fixation of small fracture fragment and did not interfere with the union, indicating that it is useful for treatment of clavicle shaft fracture.
- 374 View
- 1 Download

- Hypoesthesia after Open Reduction and Plate Fixation of Clavicular Midshaft Fractures: Correlation with Plate Location and Clinical Features of Hypoesthesia
- Seong Hun Kim, Joon Yub Kim, Kyoung Hwan Koh, Myung Gon Jung, Jae Ho Cho
- J Korean Fract Soc 2016;29(2):121-127. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.121
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study is to evaluate the correlation between the location of the plate and the incidence of clavicular hypoesthesia and the clinical features of patients with clavicular hypoesthesia after open reduction and internal fixation of clavicular midshaft fractures.
MATERIALS AND METHODS
Seventy-eight patients who underwent open reduction and plate fixation for clavicle midshaft fractures between March 2013 and October 2014 were assessed for eligibility. The total clavicular length (A), the distance to the medial end of the plate from the sternoclavicular joint (B), and the distance to the lateral end of the plate from the sternoclavicular joint (C) were measured. Correlation between the location of the clavicular plate and the incidence of clavicular hypoesthesia was evaluated. In addition, the severity, and recovery of hypoesthesia were evaluated. Patient satisfaction, pain visual analogue scale were evaluated regarding hypoesthesia.
RESULTS
The incidence of hypoesthesia was 32.1% (25/78 patients). No correlation was observed with respect to the location of the clavicular plate and the incidence of clavicular hypoesthesia (p=0.666 at the medial end, p=0.369 at the lateral end). Recovery from hypoesthesia was observed in 23 out of 25 patients (p=0.008). Patient satisfaction and pain showed negative correlation with the incidence of hypoesthesia (p=0.002 and p=0.022).
CONCLUSION
There was no correlation between clavicular hypoesthesia and the plate location. Although most cases of hypoesthesia were recovered, we should try to avoid hypoesthesia due to the negative 'correlation' with patient satisfaction and pain.
- 488 View
- 0 Download

- Usefulness of the Additional K-Wire Fixation and Suture for Reinforce the Treatment of Distal Clavicle Fracture Using Modified Tension Band Wiring
- Seung Bum Chae, Chang Hyuk Choi, Dong Young Kim
- J Korean Fract Soc 2016;29(2):107-113. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.107
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We attempted to evaluate the clinical results of modified tension band wiring (MTBW) with additional K-wire fixation and suture for distal clavicle fracture.
MATERIALS AND METHODS
Fifty-nine patients with a distal clavicle fracture from May 2009 to December 2013 treated with MTBW were enrolled in this study. Their fracture types were type 2, 12; and type 3, 33; type 4, 8; and type 5, 6 according to Craig classification group II; average age was 47.2 years with a mean follow-up period of 27.9 months. The operations were performed within a mean of 3.1 days a fter t rauma. The c linical results were evaluated u sing University of California at Los Angeles scores (UCLA), American Shoulder and Elbow Surgeons scores (ASES) and Korean Shoulder Society scores (KSS) at 1 year after surgery.
RESULTS
Radiographic bone union was achieved at a mean of 3.7 months after the operation. In the last observation, their range of motion was forward flexion 159.0°, external rotation 59.8°, and internal rotation 4.3 points, and there were 2 cases of nonunion. Each average functional score was UCLA 31.3 points, KSS 91.6 points, and ASES 93.0 points.
CONCLUSION
For the surgical treatment of distal clavicle fractures, MTBW with additional K-wire fixation and suture is a useful technique allowing early range of motion exercises, minimizing soft tissue damage, and preserving the acromio-clavicular joint. -
Citations
Citations to this article as recorded by- Treatment Results for Unstable Distal Clavicle Fractures Using Hybrid Fixations with Finger Trap Wire and Plate
Jeong-Seok Yu, Bong-Seok Yang, Byeong-Mun Park, O-Sang Kwon
Journal of the Korean Orthopaedic Association.2022; 57(2): 135. CrossRef - Comparison of Locking Compression Plate Superior Anterior Clavicle Plate with Suture Augmentation and Hook Plate for Treatment of Distal Clavicle Fractures
Jun-Cheol Choi, Woo-Suk Song, Woo-Sung Kim, Jeong-Muk Kim, Chan-Woong Byun
Archives of Hand and Microsurgery.2017; 22(4): 247. CrossRef
- Treatment Results for Unstable Distal Clavicle Fractures Using Hybrid Fixations with Finger Trap Wire and Plate
- 850 View
- 7 Download
- 2 Crossref

Case Report
- Periprosthetic Fracture after Hook Plate Fixation in Neer Type II Distal Clavicle Fracture: A Report of 3 Cases
- Kyung Yong Kim, Joon Yub Kim, Won Bok Lee, Myong Gon Jung, Jeong Hyun Yoo, Joo Hak Kim
- J Korean Fract Soc 2016;29(1):55-60. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.55
-
 Abstract
Abstract
 PDF
PDF - Hook plate fixation is a treatment method for the displaced distal clavicle fracture with favorable results regarding bone union and shoulder function, however possible complications include impingement syndromes, subacrormial erosions, acromial fractures, and periprosthetic fractures. In this report, we observed 3 cases of periprosthetic fracture after hook plate fixation. All cases of periprosthetic fractures were initiated at the medial end screw holes. The causes of these periprosthetic fractures appeared to be the off centered fixation of medial end screws near the anterior or posterior cortex which were specific during operations with hook plates with more than 6 holes and the increased stress on the medial end screw by over-reduced or inferiorly reduced position of the distal end of the clavicle by the hook plate.
-
Citations
Citations to this article as recorded by- Comparison of a novel hybrid hook locking plate fixation method with the conventional AO hook plate fixation method for Neer type V distal clavicle fractures
Joongbae Seo, Kang Heo, Seong-Jun Kim, Jun-Kyom Kim, Hee-Jung Ham, Jaesung Yoo
Orthopaedics & Traumatology: Surgery & Research.2020; 106(1): 67. CrossRef - Comparative analysis of a locking plate with an all-suture anchor versus hook plate fixation of Neer IIb distal clavicle fractures
Joong-Bae Seo, Kwon-young Kwak, Jae-Sung Yoo
Journal of Orthopaedic Surgery.2020;[Epub] CrossRef - Comparison of Locking Compression Plate Superior Anterior Clavicle Plate with Suture Augmentation and Hook Plate for Treatment of Distal Clavicle Fractures
Jun-Cheol Choi, Woo-Suk Song, Woo-Sung Kim, Jeong-Muk Kim, Chan-Woong Byun
Archives of Hand and Microsurgery.2017; 22(4): 247. CrossRef
- Comparison of a novel hybrid hook locking plate fixation method with the conventional AO hook plate fixation method for Neer type V distal clavicle fractures
- 686 View
- 1 Download
- 3 Crossref

Original Article
- Usefulness of Spring Plate for Acetabular Posterior Wall Fracture Including Small Fragment
- Jeong Hoon Kang, Sang Hong Lee, Hyeon Jun Lee
- J Korean Fract Soc 2016;29(1):19-25. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.19
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We applied internal fixation using a spring plate against an acetabular posterior wall fracture including small fragments and then evaluated the clinical and radiological results and want to understand the usefulness of the spring plate.
MATERIALS AND METHODS
Fifteen patients in whom fixation was difficult using leg screws or a metal plate because of a small bone fragment, in patients with posterior wall acetabular fractures who presented in our hospital since August of 2011 to March of 2014 were enrolled. The mean age was 42.6 years (range 24-54 years) with relatively young patients, and they were followed-up for at least one year. We analyzed the rate of reduction after surgery using the classification of Matta in radiographs, and the classification of Borrelli in 3-dimensional computed tomography (CT) and clinical results were evaluated using the clinical grading system.
RESULTS
There were five cases of anatomical reduction, 9 cases of imperfect reduction, and 1 case of unsatisfactory reduction according to the classification of Matta. Except for one case during the follow-up period, the union of bone was successful without failure of fixation and the clinical results were 6 cases of excellence, 8 cases of good, and 1 case of failure. Articular displacement was also evaluated in postoperative CT scan according to Borrelli's criteria. The mean of gap and step off was 2.04 mm, 1.3 mm.
CONCLUSION
Use of leg screw fixation and so on in posterior wall fractures including a small fragment of the acetabular rim is not easy. However the method using spring plate fixation enables relatively accurate reduction and fixation for a small fragment and the clinical outcome showed satisfactory results. -
Citations
Citations to this article as recorded by- Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate
HoeJeong Chung, Hoon-Sang Sohn, Jong-Keon Oh, Sangho Lee, DooSup Kim
Medicina.2024; 60(6): 882. CrossRef
- Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate
- 679 View
- 4 Download
- 1 Crossref

Review Article
- Surgical Treatment of Malunion and Nonunion after Pelvic Bone Fracture
- Byung Woo Min, Kyung Jae Lee
- J Korean Fract Soc 2015;28(4):266-272. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.266
-
 Abstract
Abstract
 PDF
PDF - Regardless of the efforts of several treatments after pelvic bone fracture, as many as 5% of all pelvic fractures result in malunion or nonunion of the pelvis. These complications can cause disabling symptoms, including pain, instability, and gait disturbance, which can decrease life quality of patients and increase socioeconomic problems. Therefore concerns regarding the treatment of malunion and nonunion after pelvic bone fracture are increasing. We report our experience and surgical management for pelvic malunion and nonunion.
- 781 View
- 11 Download

Original Article
- Outcomes of Severe Comminuted Distal Radius Fractures with Pronator Preserving Approach
- Seung Hyun Cho, Hong Gi Park, Deuk Soo Jun, Jae Ang Sim, Young Hak Roh, Yong Cheol Yoon, Jong Ryoon Baek
- J Korean Fract Soc 2015;28(3):178-185. Published online July 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.3.178
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We investigate the outcomes of treatment of patients with severe comminuted distal radius fractures with volar plate fixation using a pronator-preserving approach.
MATERIALS AND METHODS
Fourteen patients with severe comminution of the distal radius fractures for whom anatomical reduction of the fractures was deemed difficult to achieve with traditional approaches were enrolled. The gender ratio was 8 males to 6 females, and the average age of the patients was 64.9 years. According to the AO/OTA classification of fractures, 2 patients had 23-A3 fractures, 7 patients had 23-C2, and 5 patients had 23-C3. Radial length, radial inclination, and volar tilt were measured for radiologic evaluation. Modified Mayo wrist score (MMWS) was used for clinical outcome.
RESULTS
Bony union was achieved in all 14 patients without signs of complications. The average time-to-union was 4.3 months (3-6 months). The radiological findings at the final follow-up were as follows: the average radial inclination was 20.5degrees; the average volar tilt, 7.57degrees; and the average radial length, 11.8 mm. At the final follow-up, the results of the MMWS were 'Fair' in 1 patient, 'Good' in 4, and 'Excellent' in 9.
CONCLUSION
We propose that a pronator-preserving approach is an effective treatment for severe comminuted distal radius fracture. -
Citations
Citations to this article as recorded by- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
Jong-Ryoon Baek, Yong-Cheol Yoon, Seung Hyun Baek
Journal of the Korean Fracture Society.2019; 32(4): 204. CrossRef
- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
- 872 View
- 1 Download
- 1 Crossref

Case Report
- Infected Nonunion of Clavicle Shaft after Operation: A Case Report
- Ho Su Jang, Suk Hwan Jang
- J Korean Fract Soc 2015;28(1):77-81. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.77
-
 Abstract
Abstract
 PDF
PDF - The infected nonunion of clavicle with bone defect is an uncommon complication following clavicle shaft fracture. There were a few reports regarding treatment of the infected nonunion after clavicle fracture. We report on a case of infected clavicle nonunion successfully treated with autologous bone graft and dual plate fixation.
- 713 View
- 3 Download

Original Article
- The Surgical Outcome of Unstable Distal Clavicle Fractures Treated with 2.4 mm Volar Distal Radius Locking Plate
- Suk Kyu Choo, Ji Ho Nam, Youngwoo Kim, Hyoung Keun Oh
- J Korean Fract Soc 2015;28(1):38-45. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.38
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study evaluated the surgical outcomes of unstable distal clavicular fractures treated with a 2.4 mm volar distal radius locking plate.
MATERIALS AND METHODS
From August 2009 to August 2012, 16 patients with distal clavicle fractures underwent surgical treatment. Mean age was 36 years (18-62 years) and mean follow-up period was 12.9 months (6-32 months). Two cases were Neer type I, six cases IIa, three cases IIb, three cases III, and two cases V. For the radiologic assessment, union time and metal failure were evaluated, and coracoidiologic assessment, union time and metal failure were evaluatethe acromioclavicular joint. The clinical results were evaluated by range of motion, postoperative complication, and University of California at Los Angeles (UCLA) score.
RESULTS
Mean time to fracture union was 7.4 weeks (6-14 weeks) in all cases. No statistical difference in coracoid-clavicle distance was observed between immediate post-operation group and contra-lateral group (p=0.6), but an increase of 2.1 mm was observed in the last follow up group compared with the contra-lateral group (p<0.01). The UCLA scoring system showed excellent results in 15 cases and good results in one case. Acromial-clavicle instability occurred in one case so that metal removal and distal clavicle resection were performed.
CONCLUSION
A 2.4 mm volar distal radius locking plate can provide rigid fixation through several screw fixation in the short distal fragment and lead to satisfactory clinical outcomes in unstable distal clavicular fractures. -
Citations
Citations to this article as recorded by- Estudo retrospectivo da placa anterior superior como tratamento para fraturas instáveis da clavícula distal (tipo 2 de Neer)
Syed Ibrahim, Jimmy Joseph Meleppuram
Revista Brasileira de Ortopedia.2018; 53(3): 306. CrossRef - Retrospective study of superior anterior plate as a treatment for unstable (Neer type 2) distal clavicle fractures
Syed Ibrahim, Jimmy Joseph Meleppuram
Revista Brasileira de Ortopedia (English Edition).2018; 53(3): 306. CrossRef
- Estudo retrospectivo da placa anterior superior como tratamento para fraturas instáveis da clavícula distal (tipo 2 de Neer)
- 664 View
- 1 Download
- 2 Crossref

Case Reports
- Multiple Stress Fractures Related to Low-dose Adefovir Dipivoxil Treatment in a Patient with Chronic Hepatitis B: A Case Report
- Chul Hyun Park, Hyo Sae Ahn, Dong Chul Lee
- J Korean Fract Soc 2014;27(4):327-331. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.327
-
 Abstract
Abstract
 PDF
PDF - Stress fractures typically result from repeated abnormal mechanical loading to the bones. In particular, multiple stress fractures may occur in patients with systemic disease, such as rheumatoid arthritis, osteoporosis, or osteoarthritis. Adefovir dipivoxil (ADV), a nucleotide analogue of adenosine monophosphate, very rarely causes severe hypophosphatemia when using a low dosage of 10 mg daily for treatment of chronic hepatitis B. To the best of our knowledge, in English literature, this is the first report of multiple stress fractures in a chronic hepatitis B patient who has been treated with a low dosage of ADV. We think it is important to consider that use of ADV in a patient with chronic hepatitis B could be a risk factor for stress fractures.
- 360 View
- 0 Download

- Granulation Tissue Formed by Stimulating K-Wire Mimicking Tuberculous Cervical Lymphadenopathy: A Case Report
- Gu Hee Jung, Tae Hun Kim, Hyun Ik Cho
- J Korean Fract Soc 2014;27(3):227-231. Published online July 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.3.227
-
 Abstract
Abstract
 PDF
PDF - Pins and wires are still used frequently in surgeries of the shoulder; however, these can cause breakage or migration to surrounding tissues, leading to complications. We report on case of a patient with a neck mass who had a past history of pulmonary tuberculosis and distal clavicle fracture with internally fixated state. She was misdiagnosed as tuberculous cervical lymphadenopathy and treated for approximately one year, but was finally revealed as granulation tissue around the internally fixated distal clavicle fracture site, thus, mass excision and metal removal was performed. This case shows the importance of a proper selection device, internal fixation technique, duration, and close follow-up after the operation.
-
Citations
Citations to this article as recorded by- Kirschner Wire Migration into SpinaL Canal after Acromioclavicular Joint Fixation (Literature Review and Clinical Case)
D. A. Gulyaev, D. S. Godanyuk, T. A. Kaurova, P. V. Krasnoshlyk, S. V. Maikov
Traumatology and Orthopedics of Russia.2018; 24(4): 121. CrossRef
- Kirschner Wire Migration into SpinaL Canal after Acromioclavicular Joint Fixation (Literature Review and Clinical Case)
- 560 View
- 0 Download
- 1 Crossref

- Surgical Correction and Osteosynthesis for Cranial Displaced Pelvic Nonunion: Technical Note and Two Cases Report Regarding Anterior Correction and Osteosynthesis Following Posterior Release
- Kwang Cheon Choi, Ji Yoon Ha, Weon Yoo Kim
- J Korean Fract Soc 2014;27(2):151-156. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.151
-
 Abstract
Abstract
 PDF
PDF - Nonunion of an unstable pelvic fracture with cranial displacement pelvic surgery is technically difficult due to a large amount of bleeding and the risk of nerve damage. In addition, surgical correction of leg length discrepancy by reduction of a dislocated sacroiliac joint is in high demand. Nevertheless, when a patient is strongly disabled by a pelvic deformity, surgical correction may be necessary. Two patients with pelvic deformity were treated successfully by surgical correction and osteosynthesis.
- 441 View
- 0 Download

Original Article
- Tension Band Wiring for Distal Clavicle Fracture: Radiologic Analysis and Clinical Outcome
- Seong Cheol Moon, Chul Hee Lee, Jong Hoon Baek, Nam Su Cho, Yong Girl Rhee
- J Korean Fract Soc 2014;27(2):127-135. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.127
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the radiologic and clinical outcomes after tension band wire fixation of Neer type II distal clavicle fractures.
MATERIALS AND METHODS
Twenty-six patients with Neer type II distal clavicle fractures who underwent tension band wire fixation from March 2002 to May 2011 were included in the study. Fifteen cases were classified as Neer type IIa and 11 cases as type IIb. The postoperative mean follow-up period was 14.3 months. Clinical and radiologic evaluation was performed at two weeks, six weeks, three months, six months, and 12 months postoperatively.
RESULTS
Bony union on X-rays was observed at an average of 11.7 weeks (range 8-20 weeks) postoperatively. The overall visual analogue scale score for pain was 1.23+/-2.75 postoperatively. The overall postoperative University of California at Los Angeles score increased to 33.5+/-2.15 from the preoperative score of 21.6+/-1.91 (p<0.05).
CONCLUSION
Among various methods of treatment for Neer type II distal clavicle fracture, K-wire and tension band fixation was used and relatively satisfactory radiological and clinical results were obtained. This surgical method yields excellent clinical results, owing to its relatively easy technique, fewer complications, and allowance of early rehabilitation. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcomes of Acute Acromioclavicular Joint Dislocation: Comparison of Kirschner's Wire Transfixation and Locking Hook Plate Fixation
Yong Girl Rhee, Jung Gwan Park, Nam Su Cho, Wook Jae Song
Clinics in Shoulder and Elbow.2014; 17(4): 159. CrossRef
- Clinical and Radiologic Outcomes of Acute Acromioclavicular Joint Dislocation: Comparison of Kirschner's Wire Transfixation and Locking Hook Plate Fixation
- 897 View
- 7 Download
- 1 Crossref

Case Report
- Acute Rupture of Subclavian Artery Pseudoaneurysm after Delayed Osteosynthesis of Clavicular Fracture: A Case Report
- Oog Jin Shon, Jee Hoon Kim, Kang Hyun Park
- J Korean Fract Soc 2014;27(1):82-87. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.82
-
 Abstract
Abstract
 PDF
PDF - Subclavian vessels are well protected by muscles, fascia and sheaths, so vascular complications associated with clavicular fractures are rare. Pseudoaneurysms after clavicular fractures have been reported, and the occurrence or rupture of pseudoaneurysm has been reported rarely as a late complication. However, cases of pseudoaneurysm after rupture of the clavicular fracture following delayed osteosynthesis of the clavicular fracture have not been reported. A 58-year-old female that presented with a right clavicular shaft fracture obtained conservative treatment. Surgery was performed after 4 months because of non-union in the local medical center. After operation, rupture of the subclavian pseudoaneurysm occurred following osteosynthesis of the clavicular shaft fracture. We report this case here with a review of the literature.
- 489 View
- 1 Download

Original Articles
- Neurologic Injury within Pelvic Ring Injuries
- Ji Wan Kim, Dong Hoon Baek, Jae Hyun Kim, Young Chang Kim
- J Korean Fract Soc 2014;27(1):17-22. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.17
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the incidence of neurologic injury in pelvic ring injuries and to assess the risk factors for neurologic injury related to pelvic fractures.
MATERIALS AND METHODS
Sixty-two patients with the pelvic ring injury were enrolled in the study from March 2010 to May 2013. When the neurologic injury was suspected clinically, the electro-diagnostic tests were performed. Combined injuries, fracture types, and longitudinal displacements were examined for correlations with the neurologic injury.
RESULTS
There were 7 cases of AO/OTA type A, 37 cases of type B, and 18 cases of type C. Among them, 25 patients (40%) had combined spine fractures, and the average of longitudinal displacement was 7 mm (1-50 mm). Of the 62 patients, 13 (21%) had neurologic injury related with pelvic fractures; 5 with lumbosacral plexus injury, 5 with L5 or S1 nerve injury, 2 with obturator nerve injury, and 1 case of lateral femoral cutaneous nerve injury. There were no relationships between the neurologic injuries and fracture types (p=0.192), but the longitudinal displacements of posterior ring and combined spine fractures were related to the neurologic injury within pelvic ring injury (p=0.006, p=0.048).
CONCLUSION
The incidence of neurologic injury in pelvis fracture was 21%. In this study, the longitudinal displacements of posterior ring and combined spine fractures were risk factors for neurological injury in pelvic ring injury. -
Citations
Citations to this article as recorded by- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
Journal of the Korean Fracture Society.2018; 31(1): 9. CrossRef
- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
- 627 View
- 5 Download
- 1 Crossref

- Treatment of Unstable Sacral Fractures Related to Spino-Pelvic Dissociations
- Hong Sik Kim, Jung Hwan Lee, Ki Chul Park, Ye Soo Park
- J Korean Fract Soc 2013;26(3):178-183. Published online July 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.3.178
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the outcomes of surgical treatment modality in unstable sacral fractures combined with spinal and pelvic ring injury depending on the presence of spino-pelvic dissociations.
MATERIALS AND METHODS
The subjects were 16 patients, with unstable sacral fractures combined with spinal and pelvic ring injuries, were operated from July 2004 to January 2011. The patients were divided into 2 groups depending on the presence of spino-pelvic dissociations: those with dissociations were group 1, and those without dissociations were group 2. Group 1 was treated with spino-pelvic fixations using iliac screw, while group 2 was treated with percutaneous iliosacral screw fixations. The availability of the radiological bony union with its application periods, and clinical results using visual analogue scale (VAS) and oswestry disability index (ODI) were evaluated, retrospectively.
RESULTS
Out of 16 patients, 8 patients in group 1 were treated with spino-pelvic fixation using iliac screw, and 8 patients in group 2 were treated with percutaneous iliosacral screw fixation. The mean bony union period was 17.4 weeks in group 1, and 19.6 weeks in group 2. The Mean VAS and ODI scores on the last follow-up were 2.5 points and 15.6 points in group 1, 2 points and 18.8 points in group 2, respectively. Both groups had favorable clinical results at the last follow-up.
CONCLUSION
For surgical treatments of unstable sacral fractures, spino-pelvic fixation using iliac screws is advised for cases with combined spino-pelvic dissociation, while percutaneous iliosacral screw fixation is advised for cases without combined dissociation. -
Citations
Citations to this article as recorded by- Integrative Korean Medicine Treatment for Sacral Fracture: Two Clinical Cases
Yeon Soo Kang, Pil Je Park, So Jeong Kim, Hyun Jin Jang, Min Ju Kim, Hyeon Kyu Choi, Jeong Kyo Jeong, Ju Hyun Jeon, Young Il Kim
Journal of Acupuncture Research.2023; 40(3): 281. CrossRef - Spino-Pelvic Fixation in Unstable Sacral Fracture: A Case Report
Jung-Hwan Choi, Kyu-Tae Hwang, Seung Gun Lee, Chang-Nam Kang
Journal of the Korean Fracture Society.2018; 31(4): 145. CrossRef
- Integrative Korean Medicine Treatment for Sacral Fracture: Two Clinical Cases
- 699 View
- 1 Download
- 2 Crossref

Case Reports
- Costoclavicular Syndrome Secondary to Nonunion of a Displaced Fracture of the Clavicle, Misdiagnosed as a Simple Muscle Strain: A Case Report
- Ho Seung Jeon, Haeng Kee Noh, Seo Goo Kang, Jong Min Kim, Seung Ju Jeon
- J Korean Fract Soc 2013;26(1):60-64. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.60
-
 Abstract
Abstract
 PDF
PDF - Thoracic outlet syndrome is a relatively common disease. However, costoclavicular syndrome as a condition secondary to nonunion of a displaced fracture of the clavicle is very rare. Most clavicular fractures in adults are united with no or minimal persistent symptoms. Also, symptomatic nonunion of a displaced fracture of the clavicle is rare. A 55-year-old male initially presented with persistent forearm pain after slip-down was initially diagnosed with simple muscle strain. However, he was given a delayed diagnosis of costoclavicular syndrome, caused by compression of the subclavian artery due to trauma in the fibrotic nonunion of the right clavicle without apparent symptoms. We obtained satisfactory results by surgical treatment. Here we report this case with a review of the literature.
- 417 View
- 0 Download

- Treatment of Traumatic Posterior Dislocation of the Sternoclavicular Joint: A Case Report
- Dong Hee Kim, Do Hoon Kim, Seok Kwon Kang, Eui Chul Lee
- J Korean Fract Soc 2013;26(1):56-59. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.56
-
 Abstract
Abstract
 PDF
PDF - Compared with acromioclavicular dislocation, dislocation of the clavicle at its sternal end is uncommon and accounts for 3% of all injuries to the shoulder girdle. Furthermore, the posterior dislocation of the sternoclavicular joint is relatively a rare injury compared to the other types of sternoclavicular dislocation. We report this case since we have experience with similar cases of traumatic posterior dislocation at the sternoclavicular joint, which were successfully treated with x-ray guided reduction.
-
Citations
Citations to this article as recorded by- Posterior Sternoclavicular Dislocation: A Case Report
So Hwa Yoon, Sun Ki Kim, Ki Jun Kim
Journal of the Korean Society of Radiology.2015; 72(2): 128. CrossRef
- Posterior Sternoclavicular Dislocation: A Case Report
- 682 View
- 3 Download
- 1 Crossref

Original Article
- Anatomical Study of Symphysis Pubis Using 3 Dimensional Computed Tomography in Koreans
- Ji Wan Kim, Jung Min Park, Jae Suk Chang
- J Korean Fract Soc 2013;26(1):32-36. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.32
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To acquire anatomical data for the normal pelvic bone structure using three-dimensional computed tomography (3D CT) and to propose the most appropriate angle and screw length for safe screw insertion during symphysis pubis plating.
MATERIALS AND METHODS
We performed 3D CT analysis in 52 patients who required plating and selected a medial and lateral insertion point between the symphysis pubis and the pubic tubercle. Using a three-dimensional medical image analysis program, we evaluated the appropriate screw length, sagittal angle, and oblique angle at each point in this cohort.
RESULTS
At the medial point, the sagittal angle was determined to be 49.1degrees with an average screw length of 49.4 mm. At the lateral point, we calculated an average screw length of 49.1 mm, oblique angle of 23.2degrees, and sagittal angle of 45.7degrees. The screw length was longer in men than in women (4.6 mm and 7.3 mm, respectively) at the medial and lateral point.
CONCLUSION
At the symphysis pubis diastasis, we can insert the screw caudally at 49degrees with a minimal length of 37 mm at the medial point. We can insert the screw caudally at 46degrees, medially at 23degrees, with a minimal 34 mm length at the lateral point.
- 555 View
- 3 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


