Search
- Page Path
- HOME > Search
Original Articles
- Hook plate fixation for volar plate avulsion fractures of the middle phalanges in Korea: a case series
- Kang-San Lee, Sang-Woo Son, Hee-June Kim, Hyun-Joo Lee, Dong Hee Kim
- J Musculoskelet Trauma 2026;39(1):48-53. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00339

-
 Abstract
Abstract
 PDF
PDF - Background
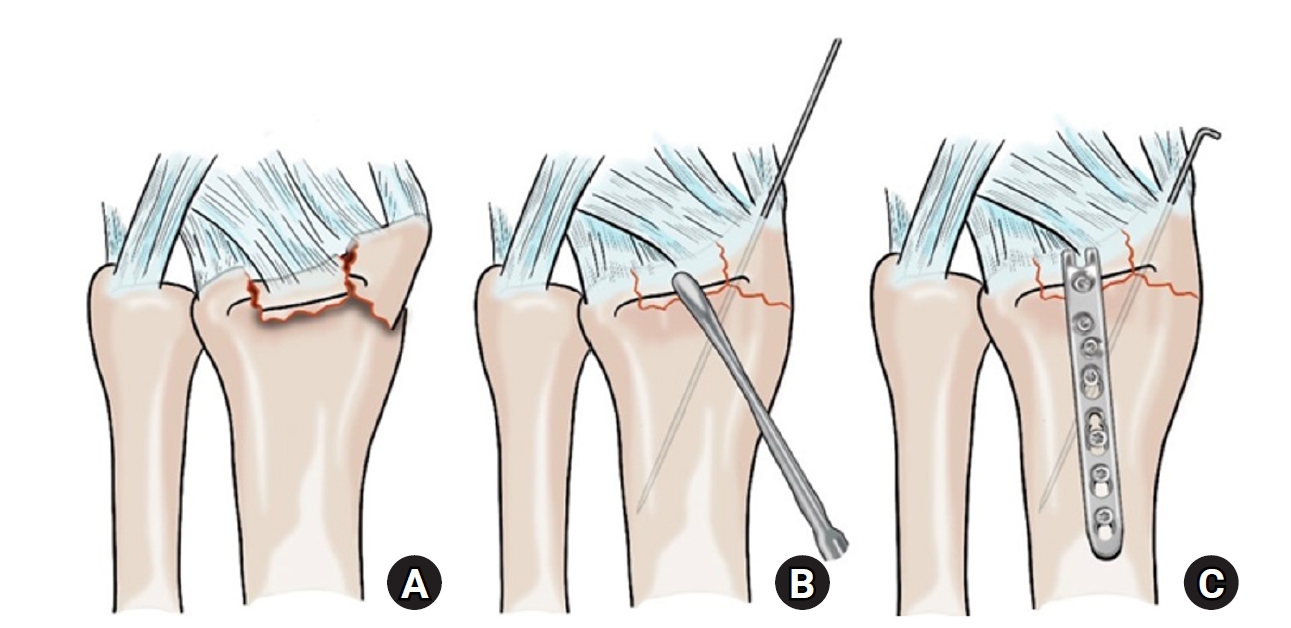
Volar plate avulsion fractures in phalanges are relatively common injuries. While surgical treatment can help reduce limitations in motion after injury, the small size of the fracture fragment can make the procedure challenging. In this study, we used hook plate fixation as a surgical technique for treating volar avulsion fractures in phalanges and evaluated its radiological and clinical outcomes.
Methods
The medical records of eight patients (nine digits) with volar plate avulsion fractures of the middle phalanx were retrospectively reviewed. All fractures were treated with a 1.5-mm hook plate after open reduction. Radiologic evaluations were performed using simple radiographs, and clinical outcomes were assessed through range of motion, instability, and pain.
Results
The mean follow-up period was 4.89 months (range, 1–9 months). All nine digits achieved bone union at the final follow-up. The mean union time was 2.2 months (range, 1–4 months). In all patients, the range of motion in the proximal interphalangeal joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. All patients demonstrated no joint instability and no residual pain.
Conclusion
Using a hook plate for volar plate avulsion fractures presents a promising alternative to existing fixation methods. Its biomechanical advantages and ease of fabrication make it a valuable tool in hand surgery. Level of evidence: IV.
- 191 View
- 8 Download

- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
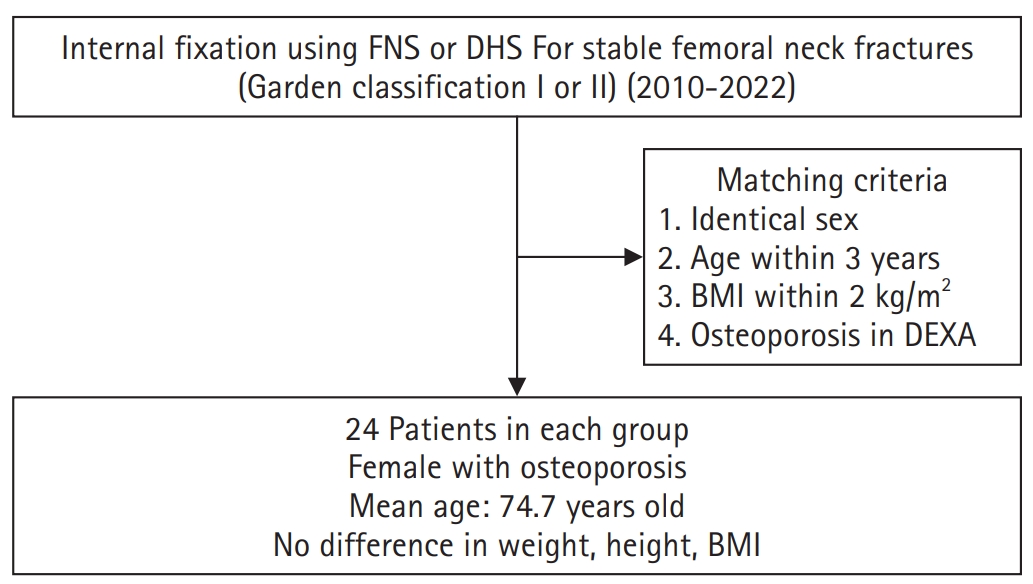
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,682 View
- 21 Download

Review Article
- Current concepts and applications of bone graft substitutes in orthopedic surgery
- Jae Ho Cho, Hyung Keun Song
- J Musculoskelet Trauma 2025;38(4):169-177. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00248
-
 Abstract
Abstract
 PDF
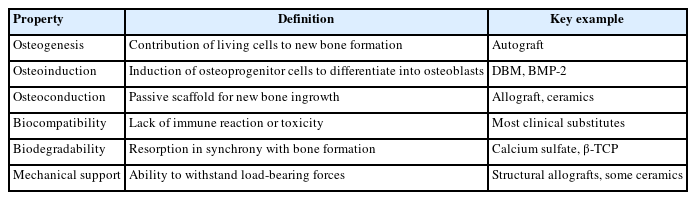
PDF - Bone defects, which often arise from high-energy injuries, infections, tumor resections, or nonunions, represent a persistent challenge in orthopedic trauma surgery. Autologous bone grafting remains the gold standard due to its unique combination of osteogenic, osteoinductive, and osteoconductive properties. However, issues such as donor site morbidity, limited graft volume, and increased surgical time have driven the development of bone graft substitutes. These substitutes vary widely in origin, composition, biological activity, and mechanical characteristics, encompassing allografts, xenografts, synthetic materials, and biologically enhanced constructs. This review outlines the fundamental biological principles underlying bone regeneration—including osteogenesis, osteoinduction, and osteoconduction—and addresses additional key factors such as biocompatibility, biodegradability, and mechanical strength. Current bone graft materials are classified by biological origin and functional characteristics, with an emphasis on their use in trauma surgery. Particular attention is given to the clinical applications, indications, and limitations of allograft-based solutions (such as structural allografts and demineralized bone matrix), synthetic ceramics (including calcium phosphate and bioactive glass), and biologically enhanced options, such as recombinant growth factors and stem cell therapies. In trauma settings, graft selection must be tailored to the characteristics of the defect, mechanical demands, the biological environment, and patient-specific factors. Integration with surgical technique and fixation is crucial for optimizing outcomes. Although modern substitutes show promise, none fully replicate the complex biology of autografts. Looking ahead, emerging technologies such as 3D printing, nanotechnology, and smart biomaterials offer exciting possibilities but face translational challenges. This review aims to provide practicing orthopedic surgeons with a concise, evidence-based overview of bone substitute options and their roles in trauma care. By applying core biological principles and clinical judgment, surgeons can better navigate the expanding array of graft materials to improve outcomes for patients with complex skeletal defects.
-
Citations
Citations to this article as recorded by- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
Seungyeob Sakong, Seokjun Hong, Wonseok Choi, Seonghyun Kang, Jae-Woo Cho, Whee Sung Son, Jeong-Seok Choi, Chang-Jin Yon, Won-Tae Cho, Jong-Keon Oh
Journal of Clinical Medicine.2026; 15(3): 1176. CrossRef
- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
- 4,318 View
- 100 Download
- 1 Crossref

Original Article
- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- Hyun-Jae Park, Joo-Hak Kim
- J Musculoskelet Trauma 2025;38(4):221-228. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00241
-
 Abstract
Abstract
 PDF
PDF - Background
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures. Level of evidence: IV.
- 382 View
- 11 Download

Review Articles
- Atypical ulnar fractures: a narrative review of current concepts and a case of bilateral surgical management
- Chi-Hoon Oh, Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):124-132. Published online July 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00227
-
 Abstract
Abstract
 PDF
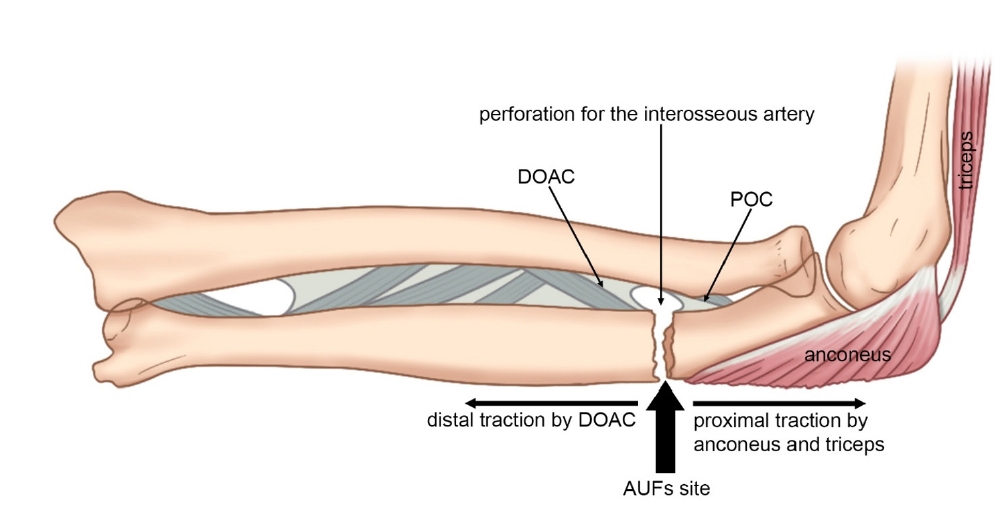
PDF - Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
- 1,522 View
- 47 Download

- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00024

-
 Abstract
Abstract
 PDF
PDF - Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Citations
Citations to this article as recorded by- Rigid intramedullary nailing with suprapatellar approach for tibial shaft fractures in adolescents with open physes
Jong Wha Lee, Jae Ho Cho, Tae Hun Kim, Hyung Keun Song, Won-Tae Cho, Seungyeob Sakong, Hyunil Choi, Sumin Lim
Injury.2026; : 113130. CrossRef - Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
Jungtae Ahn, Dae-Cheol Nam, Gu-Hee Jung
Clinics in Orthopedic Surgery.2025; 17(6): 1062. CrossRef
- Rigid intramedullary nailing with suprapatellar approach for tibial shaft fractures in adolescents with open physes
- 2,954 View
- 56 Download
- 2 Crossref

Original Articles
- Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(2):96-101. Published online February 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059
- Correction in: J Musculoskelet Trauma 2025;38(3):168

-
 Abstract
Abstract
 PDF
PDF - Background
Mayo type IIIB olecranon fractures are characterized by significant displacement and comminution, presenting a challenge in selecting the appropriate fixation technique. This study compared the clinical and radiographic outcomes, complications, and reoperation rates of reinforced tension band wiring (TBW) and precontoured plate and screw fixation (PF) in the surgical treatment of Mayo type IIIB olecranon fractures.
Methods
This retrospective review analyzed 24 patients diagnosed with Mayo type IIIB olecranon fractures, who were treated between 2005 and 2023. Of these, 11 patients underwent reinforced TBW, and 13 received precontoured PF. Clinical outcomes were assessed using Disabilities of the Arm, Shoulder, and Hand (DASH) scores and the Mayo Elbow Performance Score (MEPS). Radiographic outcomes focused on fracture union. Operative times, complication rates, and reoperation rates were compared between the groups.
Results
Both the reinforced TBW and PF groups achieved satisfactory clinical outcomes, with no significant between-group differences in DASH and MEPS scores (P>0.05). Radiographic union was achieved in all patients. The reinforced TBW group demonstrated a significantly shorter operative time than the PF group (93.6±7.4 min vs. 132.3±13.7 min; P<0.001). Complication rates were similar between the two groups (reinforced TBW, 38.4%; PF, 36.3%), but hardware-related irritation occurred more frequently in the reinforced TBW group. Reoperations were required in 15.8% of the reinforced TBW group due to hardware irritation, whereas no reoperations were necessary in the PF group.
Conclusions
Reinforced TBW and PF are both effective surgical options for managing Mayo type IIIB olecranon fractures, yielding comparable clinical and radiographic outcomes. While reinforced TBW offers shorter operative times and lower costs, PF is associated with fewer hardware-related complications. Further prospective studies are needed to optimize treatment strategies for these complex fractures. Level of Evidence: Level III. -
Citations
Citations to this article as recorded by- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
Reva Qiu, Mallika Makkar, Richard Buckley
Injury.2025; 56(11): 112769. CrossRef
- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
- 2,292 View
- 51 Download
- 1 Crossref

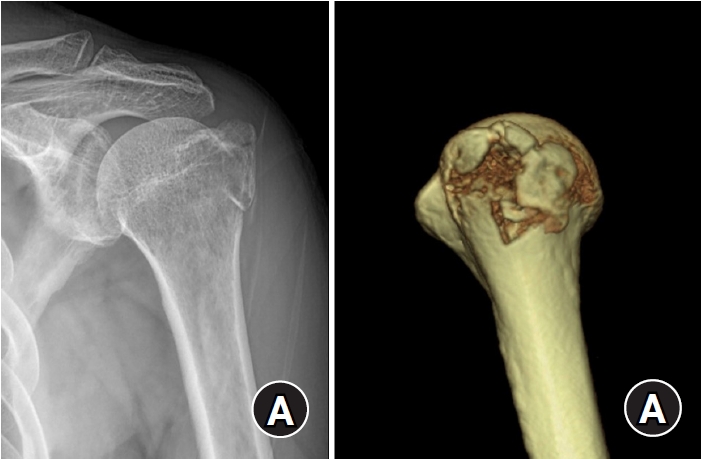
- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005
-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 2,048 View
- 59 Download

- Comparison of the Radiological Outcomes of an Anatomical Quadrilateral Surface Plate with a Pelvic Reconstruction Plate in Acetabulum Fractures
- Sung Hyun Yoon, Hee Gon Park, Dong Uk Lee
- J Korean Fract Soc 2024;37(2):95-101. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.95
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the radiological outcomes of fixation using an anatomical quadrilateral surface plate with those using a traditional pelvic reconstruction plate for fractures involving the quadrilateral surface or superomedial wall of the acetabulum.
Materials and Methods
From 2015 to 2022, 47 patients who met the inclusion and exclusion criteria were analyzed retrospectively. Internal fixation of an acetabular fracture was achieved with a pelvic reconstruction plate (n=28) or an anatomical quadrilateral surface plate (n=19). The ability to achieve immediate postoperative anatomical reduction and the long-term outcomes were assessed by confirming the arthritic changes. Immediate postoperative reduction quality and long-term radiological outcomes for post-traumatic arthritis were assessed using the Matta scoring system on standard radiographs.
Results
The assessment of immediate postoperative reduction in the pelvic reconstruction plate group was satisfactory in 16 patients (57.1%) and unsatisfactory in 12 patients (42.9%). In the anatomical quadrilateral surface plate group, the results were satisfactory in 16 patients (84.2%) and unsatisfactory in 3 patients (15.8%). When evaluating over an extended follow-up period in the pelvic reconstruction plate group, 19 patients (67.9%) demonstrated satisfactory, while 9 patients (32.1%) had unsatisfactory outcomes. In the anatomical quadrilateral surface plate group, 12 patients (63.2%) achieved satisfactory, and 7 patients (36.8%) had unsatisfactory outcomes. The immediate postoperative reduction quality was superior in the anatomical quadrilateral surface plate group (p=0.03). Comparing longterm results, the anatomical quadrilateral surface plate group did not have statistically more favorable outcomes (p=0.49).
Conclusion
In this study, the anatomical quadrilateral surface plate achieved sufficiently good radiological results without significant difference from the existing pelvic reconstruction plate. It was concluded that it is a useful option that can replace the existing metal plate in the selection of surgery for acetabular fractures.
- 923 View
- 10 Download

- Bone Union Time of Simple Distal Femur Fractures in the Elderly according to Fracture Gap after Treated with Minimally Invasive Plate Osteosynthesis
- Young Ho Cho, Sangwoo Kim, Jaewook Koo
- J Korean Fract Soc 2023;36(4):133-138. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.133
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the difference in bone union time according to the fracture gap after minimally invasive plate osteosynthesis (MIPO) for simple distal femoral fractures in elderly patients.
Materials and Methods
From January 2010 to December 2019, patients aged 60 years or older who underwent surgical treatment for distal femoral fractures due to a low-energy injury were investigated retrospectively. Forty patients were enrolled in the study. The patients were divided into two groups according to the fracture gap after reduction: no more than 2 mm (Group A) and more than 2 mm (Group B) in the anteroposterior and lateral plane. The demographic, operation time, presence or absence of cerclage wiring, plate screw density, plate span ratio, plate length, bone union period, non-union, and complications were evaluated.
Results
No statistical differences in operation time, cerclage wiring, plate screw density, plate span ratio, and plate length were observed between the two groups, and the bone union was achieved in all patients without complication. The bone union period was 17.24±1.48 weeks in Group A and 24.53± 5.20 weeks in Group B, which was statistically significant (p<0.001).
Conclusion
The bone union time in treating geriatric simple distal femur fractures using the MIPO tech-nique was significantly shorter in the 2 mm or less fracture gap than in the greater than 2 mm group.
- 760 View
- 5 Download

- Risk Factors of Fixation Failure in Femoral Neck Fractures
- Sung Hyun Yoon, Kyu Beom Kim, Hyung Jun Lee, Kyung Wook Kim
- J Korean Fract Soc 2023;36(4):118-124. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.118
-
 Abstract
Abstract
 PDF
PDF - Purpose
Internal fixation after a femoral neck fracture (FNF) is one of the conventional treatment options for the young and active elderly patients. However, fixation failure of internal fixation is a probable complication. The treatment of fixation failure after a primary internal fixation of the FNF remains a challenge.
Materials and Methods
Between July 2002 and March 2017, 83 patients who underwent internal fixation after FNF were retrospectively analyzed. Radiological assessments, including Pauwels’ angle, fracture level, reduction quality, and bone union, were measured, preoperatively and postoperatively. Moreover, intraoperative variables such as time to surgery, surgical time, and estimated blood loss were also evaluated.
Results
The patients were divided into the fixation failure and the non-failure groups. Among the 83 patients, 17 cases (20.5%) of fixation failure after the primary internal fixation of the FNF were identi-fied. When comparing the two groups according to the radiographic data, Pauwels’ angle and the reduction quality based on Garden’s angle showed significant differences (p<0.001). Moreover, when comparing the intraoperative variables, unlike the surgical time and estimated blood loss, significant differences were noted in the time interval from injury to surgery and specifically in whether the surgery was performed within 12 hours after injury (p<0.001).
Conclusion
Pauwels’ angle, reduction quality, and time to surgery are the major factors that can predict the possibility of internal fixation failure of the FNF. Early and accurate anatomical reduction is needed to decrease complications after the internal fixation of the FNF.
- 2,637 View
- 37 Download

Case Report
- Irreducible Ankle Fracture Dislocation due to Dislocated Tibialis Posterior Tendon - A Case Report -
- Seungyup Shin, Bum-Soo Kim, Ji-Won Lee, Euisun Yoon
- J Korean Fract Soc 2023;36(2):52-56. Published online April 30, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.2.52
-
 Abstract
Abstract
 PDF
PDF - An irreducible ankle dislocation is a rare injury. The cause is a dislocation of the distal fibula anteriorly or posteriorly or the insertion of soft tissue, such as the deltoid ligament or posteromedial tendon. The tibialis posterior tendon can be dislocated through distal tibiofibular diastasis and prevent reduction of the ankle joint. The authors experienced anterolateral ankle fracture dislocation with a diastasis of the distal tibiofibular joint, and reduction was impossible because of impingement of the tibialis posterior tendon dislocated anteriorly through the distal tibiofibular diastasis. This paper reports the treatment of this injury.
- 589 View
- 12 Download

Review Article
- Fragility Fractures of the Pelvis and Sacrum
- Se-Won Lee, Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):29-38. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.29
-
 Abstract
Abstract
 PDF
PDF - The incidence of fragility fractures of the pelvis (FFP) has increased significantly due to the aging popu-lation and improved diagnostic modalities. The evaluation and treatment of these patients differ from that of high-energy pelvic ring injuries typically seen in younger patients. Therefore, it is important to classify the FFP by patterns of the classification system to standardize optimal treatment criteria and appropriate treatment strategy. However, some cases are not classifiable according to the FFP classifi-cation. A newly proposed classification that can be verified by comparing existing FFP classifications is needed to overcome the weak points. Non-operative treatment is usually considered first and should focus on early mobilization. Operative fixation should focus on stabilizing the minimally invasive pelvic ring than the reduction of fractures to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility.
- 1,908 View
- 33 Download

Technical Note
- Usefulness of Reduction and Internal Fixation Using a 2.4 mm Hand Plating System in Type AO 33-A3 Distal Femur Fracture - Technical Note -
- Bong-Ju Lee, Ja-Yeong Yoon, Seungha Woo
- J Korean Fract Soc 2023;36(1):25-28. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.25
-
 Abstract
Abstract
 PDF
PDF - Open reduction in an AO 33-A3 class distal femur transverse and comminuted fracture is often difficult due to frequent reduction loss during surgery, leading to longer operative time and increased blood loss intra-operation. In this study, the authors report a case in which the use of an offset grid plate (OsteoMed, USA) using 2.4 mm HPS (hand plating system) eased the process of fracture reduction and achieved a stable internal fixation, ultimately leading to successful osteosynthesis. The authors experienced no need for temporary fixation devices such as K-wires or screws, which are otherwise required to stabilize the reduction. The fracture reduction was stable throughout the primary fixation of the fracture using a locking plate and screws. The authors report that the advantage of the HPS plate is fitting into the cortical contour and providing stable maintenance of fracture reduction intra-operation, which would be beneficial in certain distal femoral fracture patterns.
- 536 View
- 9 Download

Original Article
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
- J Korean Fract Soc 2022;35(4):162-168. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
-
 Abstract
Abstract
 PDF
PDF - Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies. -
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 3,644 View
- 53 Download
- 2 Crossref

Review Article
- Surgical Treatment of Distal Radius Fractures and Treatment of Common Accompanying Lesions
- Joo-Hak Kim
- J Korean Fract Soc 2022;35(3):120-127. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.120
-
 Abstract
Abstract
 PDF
PDF - There have been major advances in the treatment of distal radius fractures over the past 20 years. Specifically, the development of the volar locking plate in 2001 and the subsequent improvements in its design and performance have enabled the treatment of distal radius fractures that were previously considered difficult to treat. The volar plate is used for fractures and shows good results with anatomical reduction and firm fixation. However, when trying to apply it to more complex fractures, there are still difficulties related to the unique anatomical structure of the distal radius, and there are also several factors that can impair joint function and cause pain after surgery. In this review, the factors to be considered to ensure better outcomes during ORIF (open reduction and internal fixation), and external fixation in the treatment of distal radial fractures are described. The review also details the common accompanying injuries and management methods.
- 743 View
- 18 Download

Case Report
- Two-Year Follow-Up Results after Tendon Graft and Corrective Osteotomy for the Delayed Rupture of the 2nd-5th Flexor Tendons due to a Malunion of a Distal Radius Fracture - A Case Report -
- Jeung-Hwan Seo, Hyun-Gon Gwak, Jae Hoon Lee
- J Korean Fract Soc 2022;35(2):63-67. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.63
-
 Abstract
Abstract
 PDF
PDF - The delayed rupture of the flexor tendons is a rare complication of malunited distal radius fractures after nonoperative management. The known cause of a flexor tendon rupture is attrition between the palmarly displaced ulnar head and the involved tendons. Sharp bony spurs on the volar side of the malunited distal radius can also cause flexor tendon rupture. About 30 cases have been reported in literature. There were only four case reports about the delayed rupture of the 2nd, 3rd, 4th, and 5th flexor tendons. In this case, we experienced flexor digitorum superficialis and flexor digitorum profundus tendon ruptures of the index, middle, ring, and little fingers, after 8 months following the malunion of a distal radius fracture. At two years follow-up after tendon graft and corrective osteotomy, the range of motion and motor weakness of the 2nd, 3rd, 4th, and 5th fingers improved.
- 461 View
- 2 Download

Original Articles
- Surgical Treatment of AO/OTA 33-C Intra-Articular Distal Femoral Fractures through Parapatellar Approach
- Suk Kyu Choo, Sung Tan Cho, Hyoung Keun Oh
- J Korean Fract Soc 2022;35(1):1-8. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To report the surgical results of the parapatellar approach for AO/OTA 33-C distal femoral intra-articular fractures.
Materials and Methods
Twenty-one patients with AO/OTA 33-C distal femoral intra-articular fracture were included. There were 11 cases of C2 and 10 cases of C3 fractures. The time of union and the coronal alignment were radiographically investigated. The complications related to surgery were clinically investigated, and a functional evaluation using the range of motion and Oxford knee score was performed to compare the surgical results according to fracture classification.
Results
In all cases, sufficient articular exposure and anatomical reduction were achieved with the parapatellar approach. No cases of coronal malalignment, loss of reduction, and plate failure were noted. On the other hand, in four cases (19.0%), an autogenous bone graft was performed due to delayed union on the meta-diaphyseal fracture site. There were no differences in the radiological and clinical outcomes of the C2 and C3 fractures. The knee joint pain and Oxford knee score were poorer in the delayed union group than the normal union group.
Conclusion
The parapatellar approach is useful for achieving an anatomical reduction of the articular surface of the distal femur and minimally invasive plating technique. Although satisfactory surgical results could be obtained regardless of the degree of articular comminution, a study of the risk factors of delayed metaphyseal fusion may be necessary.
- 532 View
- 5 Download

- Comparing Outcomes of Retrograde Intramedullary Nail and Locking Plate Fixation in Distal Femoral Fractures
- Byung-Ho Yoon, Bo Kwon Hwang, Hyoung-Keun Oh, Suk Kyu Choo, Jong Min Sohn, Yerl-Bo Sung
- J Korean Fract Soc 2021;34(4):131-136. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.131
-
 Abstract
Abstract
 PDF
PDF - Purpose
We compared the radiological and clinical results of fixation for distal femoral fracture (DFF) using a locking compression plate (LCP) or a retrograde intramedullary nail (RIN).
Materials and Methods
From October 2003 to February 2020, 52 cases of DFF with a minimum 1-year follow-up (with a mean follow-up of 19.1 months) were included: 31 were treated with LCP and 21 with RIN. The operation time, blood loss, and hospitalization period were compared, and the incidence of postoperative nonunion, malunion, delayed union and metal failure and other post-operative complications were evaluated and compared.
Results
There was no significant difference in the operating time between the two groups, but the mean blood loss was significantly higher in the LCP group (LCP 683.5 ml vs RIN; 134.9 ml; p=0.015). In 49 out of 52 cases, bone union was achieved without additional surgery in an average of 6.8 months, and a complete union was achieved after additional surgery in three cases of nonunion (LCP 2 cases vs RIN 1 case; p=0.065). One case of malunion and superficial infection was confirmed in each group.
Conclusion
Internal fixation using LCP and RIN give good outcomes with a low complication rate and can therefore be considered useful surgical treatments for DFF.
- 480 View
- 6 Download

Review Articles
- Current Concepts of Vitamin D and Calcium in the Healing of Fractures
- Jihyo Hwang
- J Korean Fract Soc 2021;34(3):117-121. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.117
-
 Abstract
Abstract
 PDF
PDF - Fragile fractures, also known as osteoporosis fractures, insufficiency fractures, and senile fractures are a significant problem encountered by orthopedic surgeons. Calcium and vitamin D are essential for maintaining bone health and deficiencies in calcium and vitamin D are major risk factors for the development of osteoporosis. Sufficient amounts of calcium are also required for fracture-callus mineralization. Hence, compromised bone repair that is frequently observed in osteoporotic patients might be attributed to calcium and vitamin D deficiencies. Consequently, calcium and vitamin D supplementation represents a potential strategy for treating compromised fracture healing in osteoporotic patients. There is some clinical evidence of the positive effect of supplementation in fracture healing and posttraumatic bone turnover, but research in this area is ongoing. Calcium and vitamin D should be the primary treatment of choice in osteopenic patients with an insufficiency of calcium and vitamin D and for the prevention of secondary osteoporotic fractures. Calcium and vitamin D can also be used as addition to other primary osteoporotic medications such as antiresorptive or bone-forming agents. The role of calcium and vitamin D in fracture healing and the therapeutic potential of calcium and vitamin D supplementation is summarized in this context.
- 6,903 View
- 81 Download

- Pediatric Femoral Neck Fracture
- Joo Hyung Han, Hoon Park
- J Korean Fract Soc 2021;34(1):34-43. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.34
-
 Abstract
Abstract
 PDF
PDF - Pediatric femoral neck fracture is an uncommon injury with a high complication rate, regardless of the appropriate diagnosis and management. The bony anatomy and blood supply of the proximal femur in a skeletally immature patient differ from those in adult patients. Generally, these fractures result from high-energy trauma, but pathologic hip fractures also occur, usually from low-energy trauma. Pediatric femoral neck fractures are categorized using the Delbet classification system. This classification guides management and aids clinicians in determining the risk of avascular osteonecrosis. The ideal surgical treatment is determined by the fracture type and the age of the patient. Reduction, which is achieved using a closed or open procedure, combined with stable fixation and/or cast immobilization, is recommended for most of these fractures. Anatomical reduction within 24 hours from the injury may result in a good surgical outcome. Although the effects of capsular decompression after reduction and fixation have not been established, decompression is easy to perform and may reduce the risk of avascular necrosis. Despite appropriate management, osteonecrosis can occur after all types of pediatric femur neck fractures. Other complications include coxa vara, nonunion, and premature physeal arrest.
- 1,412 View
- 29 Download

Original Articles
- Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
- Jae Youn Yoon, Ji Wan Kim
- J Korean Fract Soc 2020;33(4):189-195. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.189
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical results and implant safety of a newly developed implant, Trochanteric Fixation Nail-Advanced (TFNA; DePuy Synthes), in the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective cohort study of 26 patients diagnosed with proximal femur fracture and treated surgically with TFNA. The patients’ demographic data, surgical data, radiologic findings, and functional outcomes, including complications, were evaluated.
Results
The mean age of the patients was 71.2 years (95% confidence interval [CI], 68.2-74.2); 65.4% were female. The mean Carlson comorbidity index score was 5.4, and the mean Koval grade before fracture was 2.1. Fracture classification included four cases of AO/OTA 31.A1, nine cases of A2, six cases of A3, and seven cases of 32A including six cases of atypical femoral fractures. The mean operating time was 53.3 minutes (95% CI, 43.6-63.1). There were no early postoperative complications, such as postoperative infection, deep vein thrombosis, pulmonary embolism, or in-hospital death, except one case of pneumonia. The mean Koval score at the postoperative six-month follow-up was 2.9. EuroQol-5 Dimension (EQ-5D) increased from 0.05 to 0.54 after three months and 0.72 at six months postoperatively. Bone union was observed in all cases with a mean union time of 12.9 weeks. No implant failure occurred, and no cases required secondary revision surgery.
Conclusion
A new intramedullary nail system, TFNA, showed excellent outcomes and safety in the surgical treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
Daniel Scott Horwitz, Ahmed Nageeb Mahmoud, Michael Suk
Journal of the American Academy of Orthopaedic Surgeons.2025; 33(19): 1071. CrossRef - Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef - Prospective randomized multicenter noninferiority clinical trial evaluating the use of TFN-advancedTM proximal femoral nailing system (TFNA) for the treatment of proximal femur fracture in a Chinese population
Lidan Zhang, Zhijun Pan, Xiaohui Zheng, Qiugen Wang, Peifu Tang, Fang Zhou, Fan Liu, Bin Yu, Frankie K. L. Leung, Alex Wu, Suzanne Hughson, Zhuo Chen, Michael Blauth, Anthony Rosner, Charisse Sparks, Manyi Wang
European Journal of Trauma and Emergency Surgery.2023; 49(3): 1561. CrossRef - Risk of shortening in operatively treated proximal femur fractures with cephalomedullary nails with dynamically versus statically locked helical blades
Nathan Cherian, Lasun Oladeji, Cole Ohnoutka, Dan Touhey, Madeline Sauer, Kyle A. Schweser, Mauricio Kfuri, James L. Cook, Gregory J. Della Rocca, Brett D. Crist
Injury.2023; 54(2): 669. CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
Journal of the Korean Fracture Society.2022; 35(4): 135. CrossRef - Conventional versus helical blade screw insertion following the removal of the femoral head screw: a biomechanical evaluation using trochanteric gamma 3 locking nail versus PFN antirotation
Hong Man Cho, Kwang Min Park, Tae Gon Jung, Ji Yeon Park, Young Lee
BMC Musculoskeletal Disorders.2021;[Epub] CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef
- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
- 2,452 View
- 24 Download
- 10 Crossref

- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 966 View
- 6 Download
- 1 Crossref

- Surgical Treatment of Pediatric Intra-Articular Proximal Phalangeal Head Fracture of the Big Toe
- Yeun Soo Kim, Geunwu Gimm, Il ung Hwang, Goo Hyun Baek, Jihyeung Kim
- J Korean Fract Soc 2020;33(1):9-15. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.9
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Pediatric intra-articularproximal phalangeal head fractures of the big toe are very rare and few studies on this have been published. The purpose of this study is to present the diagnostic approach and surgical management of these extremely rare fractures, which might be easily underestimated or misdiagnosed.
MATERIALS AND METHODS
The study retrospectively reviewed all the patients who were diagnosed as intra-articular proximal phalangeal head fracture of the big toe and who underwent surgical intervention in our institution. The size of the bony fragment and hallux valgus interphalangeus angle were measured on the preoperative X-rays. The size and rotation of the osteochondral fragment, the presence of avascular necrosis, ligamentous injury and soft tissue entrapment were assessed on the preoperative magnetic resonance images (MRIs). The radiologic and functional evaluation were performed at 1 year postoperatively.
RESULTS
The average size of the bony fragments measured on the X-rays was 4.1 mm in width and 2.3 mm in length. Two cases showed hallux valgus interphalangeus. Preoperative MRI was performed in four cases and the average size of any osteochondral lesion was 5.3 mm in width, 3.9 mm in length, and 4.7 mm in height. Rotation of the osteochondral fragment was observed in one patient, and soft tissue entrapment was noted in two patients. Postoperatively, successful bony union was achieved in all the patients and the average time to union was 74.4 days.
CONCLUSION
Intra-articular proximal phalangeal head fractures of the big toe are very rare and often neglected due to incomplete ossification in the pediatric population. It is important to suspect the presence of this intra-articular fracture and to appropriately implement further evaluation. Nonunion of chronic cases as well as acute fractures can be successfully treated through open reduction and internal fixation using multiple K-wires.
- 1,000 View
- 10 Download

Case Report
- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
- Yongun Cho, Jai Hyung Park, Se Jin Park, Ingyu Lee, Eugene Kim
- J Korean Fract Soc 2019;32(4):222-226. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.222
-
 Abstract
Abstract
 PDF
PDF - This paper reports the use of a traction device for the treatment of neglected proximal interphalangeal fracture dislocations. A 44-year-old man with a fracture dislocation of a right ring finger proximal interphalangeal joint was admitted 17 days after the injury. Closed reduction and external fixation were performed using a dynamic traction device and C-arm under a brachial plexus block. Passive range of motion exercise was started after two weeks postoperatively and active range of motion exercise was started after three weeks. The traction device was removed after five weeks. No infection occurred during the traction period. No subluxation or displacement was observed on the X-ray taken two months postoperatively. The active range of motion of the proximal interphalangeal joint was 90°. The patient was satisfied with the functional result of the treatment with the traction device. The dynamic traction device is an effective treatment for neglected fracture dislocations of the proximal interphalangeal joint of a finger.
- 1,484 View
- 9 Download

Original Articles
- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
- Jong Ryoon Baek, Yong Cheol Yoon, Seung Hyun Baek
- J Korean Fract Soc 2019;32(4):204-210. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.204
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study investigated the clinical and radiological outcomes of patients undergoing provisional fixation in conjunction with locking plate fixation. Miniplates were used as the reduction plates for the surgical treatment of severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius.
MATERIALS AND METHODS
The radial length, radial inclination, volar tilt, and radial intra-articular step-off were measured preoperatively, postoperatively, and at one year after surgery in 12 patients (eight males, four females, mean age 55.4 years old). The patients underwent volar locking plate fixation with miniplate as a reduction plate for severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius. Clinical evaluations were conducted using the modified Mayo wrist score (MMWS).
RESULTS
Bone union was achieved in all cases. The mean MMWS was 81.8 points, including two excellent, three good, and seven fair cases. Radiological improvements were observed in the average radial length (preoperative, 6.4 mm; postoperative, 11.8 mm), average radial inclination (10.2° to 22.4°), average volar tilt (−4.5° to 10.6°), and average radial intra-articular step-off (4.8–0.8 mm) (all, p<0.05). Radiographic measurements obtained immediately after surgery and at the final follow-up revealed insignificant decreases in radial length (0.6 mm), radial inclination (0.4°), and volar tilt (0.9°) (all, p>0.05).
CONCLUSION
Miniplate fixation can be an effective treatment option as a reduction plate for the treatment of distal radial fractures, which is challenging to reduce and maintain due to severely comminuted metadiaphysis fractures with the intra-articular fracture.
- 745 View
- 4 Download

- Open Reduction and Internal Fixation in Comminuted Radial Head Fracture
- Jun Ku Lee, Tae Ho Kim, Choongki Kim, Soo Hong Han
- J Korean Fract Soc 2019;32(4):173-180. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Radial head fractures, which account for 33% of all fractures, are treated depending on the Mason classification. In comminuted type 3 fractures, open reduction internal fixation (ORIF), and radial head arthroplasty are the treatment options. This study examined the clinical outcome of modified Mason type 3 radial head fractures using ORIF with a plate.
MATERIALS AND METHODS
The medical records and image of 33 patients, who underwent ORIF for modified Mason type 3 radial head fractures, were reviewed retrospectively. The preoperative plain radiographs and computed tomography images were used to examine the location of the fracture of the radial head, the number of fragments, union, joint alignment, and traumatic arthritis at the final follow-up. The range of motion (ROM) of the elbow at the last follow-up, pain score (visual analogue scale), modified Mayo elbow score (MMES), and complications were analyzed for the clinical outcome.
RESULTS
Of the 33 cases, 14 were men and 19 were women. The mean age was 41.8 years and the average follow-up period was 19 months. The functional ROM was divided into three groups according to the number of bone fragments: 141.2°±9.3° of 3 (n=20), 123.8°±18.5° of 4 (n=7), 100.7°±24.4° of more than 4 (n=6). Furthermore, the MMES were 88.2±2.9, 83.7±4.3, and 77.3±8.4, respectively (p=0.027). Depending on the radial head fracture location, the ROM and MMES were 130.7°±7.5° and 82.1±4.7, respectively, with poor outcomes on the ulnar aspect compared to 143.1°±3.8° and 89.9±3.2 on the radial aspect.
CONCLUSION
Various factors, such as the degree of crushing and location involved in the clinical outcome. In particular, the result was poor in the case of more than four comminuted fragments or chief position located in the ulnar aspect. In this case, radial head arthroplasty may be considered in the early stages. -
Citations
Citations to this article as recorded by- Does the coronoid fracture in terrible triad injury always need to be fixed?
Yeong-Seub Ahn, Seong-Hwan Woo, Sungmin Kim, Jun-Hyuk Lim, Tae-Hoon An, Myung-Sun Kim
BMC Surgery.2024;[Epub] CrossRef - Results of the Use of Bioabsorbable Magnesium Screws for Surgical Treatment of Mason Type II Radial Head Fractures
Chul-Hyung Lee, Seungha Woo, Hyun Duck Choi
Clinics in Orthopedic Surgery.2023; 15(6): 1013. CrossRef
- Does the coronoid fracture in terrible triad injury always need to be fixed?
- 1,052 View
- 5 Download
- 2 Crossref

- Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Osteoporotic Sacral Fracture
- Cheol hwan Kim, Young yool Chung, Seung woo Shim, Sung nyun Baek, Choong young Kim
- J Korean Fract Soc 2019;32(4):165-172. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.165
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The prevalence of osteoporotic sacral fractures is increasing. Traditionally, conservative treatment is the 1st option, but it can increase the risk of comorbidity in the elderly. To reduce the complications and allow early mobility, iliosacral screw fixation with cement augmentation will be one of the treatment options for patients with osteoporotic sacral fractures.
MATERIALS AND METHODS
This study reviewed 25 patients (30 cases) who had undergone percutaneous iliosacral screw fixation with cement augmentation for osteoporotic sacral fractures from July 2012 to December 2018 with a minimum follow up of six months. The clinical outcomes were assessed using the measures of pain (visual analogue scale [VAS] score), hospital stay and the date when weight-bearing started. All patients were evaluated radiologically for pull-out of screw, bone-union, and cement-leakage.
RESULTS
Bone union was achieved in 30 cases (100%). The mean duration of the hospital stay was 24 days (4–66 days); weight-bearing was performed on an average nine days after surgery. The VAS scores immediately (3.16) and three months after surgery (2.63) were lower than that of the preoperative VAS score (8.3) (p<0.05). No cases of cement-leakage or neurologic symptoms were encountered. Two patients (6.7%) experienced a pulling-out of the screw, but bone-union was accomplished without any additional procedures.
CONCLUSION
Percutaneous iliosacral fixation with cement augmentation will be an appropriate and safe surgical option for osteoporotic sacral fractures in the elderly in terms of early weight-bearing, pain reduction, and bone-union. -
Citations
Citations to this article as recorded by- Role of Augmentation in the Fixation of Osteoporotic Fractures
Chinmoy Das, Partha Pratim Das
Indian Journal of Orthopaedics.2025; 59(3): 294. CrossRef
- Role of Augmentation in the Fixation of Osteoporotic Fractures
- 990 View
- 4 Download
- 1 Crossref

- Surgical Outcomes of the Monteggia Type 2 Fracture Dislocation in Adults
- Sung Choi, Daegeun Jeong, Youngsoo Byun, Taehoe Gu, Sungsoo Ha, Dongju Shin
- J Korean Fract Soc 2019;32(1):6-13. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.6
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study examined clinical outcomes of Monteggia fracture type 2, which is the most common in adults with a high rate of accompanied injuries.
MATERIALS AND METHODS
From June 2004 to November 2015, a retrospective study was performed on 12 patients diagnosed with Monteggia fracture type 2 with a follow-up period of at least 6 months after surgery. The clinical outcomes were evaluated using the Mayo elbow performance score (MEPS), and the existence of accompanied injures, radiological result, and complications were analyzed.
RESULTS
Posterior instability was confirmed in all patients and accompanied fractures were detected in 9 patients (75.0%) on the radial head, whereas 10 patients (83.3%) were found on the coronoid process. The average arc of motion was 107° (70°–130°) and the mean MEPS was 89 (45–100). Additional re-operation due to re-dislocation, radioulnar synostosis, elbow instability, ulna nonunion, and radial head nonunion were performed in 4 cases (33.3%).
CONCLUSION
The Monteggia fracture type 2 is more commonly associated with radial head fractures and coronoid process fractures rather than other types, which causes elbow instability. Because the rate of additional surgery due to complications is high, the treatment of Monteggia fracture type 2 requires careful assessments.
- 950 View
- 5 Download

- Treatment of the Proximal Femoral Fracture Using the New Design Cephalomedullary Nail: Prospective Outcomes Study
- Young Ho Roh, Joseph Rho, Kwang Woo Nam
- J Korean Fract Soc 2019;32(1):35-42. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.35
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study is to investigate the clinical performance and safety of Zimmer® natural nail cephalomedullary nail (ZNN CM nail) in the treatment of proximal femur fractures.
MATERIALS AND METHODS
The following research was conducted as a prospective, non-comparative, single center outcome study. Upon providing written informed consent, enrolled patients' data were collected and analyzed. Postoperative follow-up visits were scheduled at 6 weeks, 3 months, 6 months, and 1 year. Follow-up evaluation included radiographic assessment, physical examination, and quality of life and adverse events reports.
RESULTS
Thirty-nine patients were available for evaluation at one year postoperative. The patients reported the mean EuroQol-5 Dimension score increased after surgery: from 0.4 points at discharge (n=49) to 0.6 points at 1-year post-surgery (n=39). The mean Harris hip score also increased after surgery: from 56.3 points at discharge (n=49) to 72.1 points at 1 year (n=12). Bone union was seen in 64% (n=16) in 6 months and 95% (n=37) in 1 year.
CONCLUSION
The results of this 1-year follow-up study affirmed the effectiveness and safety of the ZNN CM nail in the treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
Jae Youn Yoon, Ji Wan Kim
Journal of the Korean Fracture Society.2020; 33(4): 189. CrossRef
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- 909 View
- 0 Download
- 2 Crossref

Review Article
- Atypical Femoral Fractures: What Do We Know about Them?
- Beom Seok Lee, Young Kyun Lee, Heejae Won, Hyungkook Kim, Kyung Hoi Koo
- J Korean Fract Soc 2018;31(4):159-164. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.159
-
 Abstract
Abstract
 PDF
PDF - Recently, atypical femoral fractures (AFFs) have been found in patients who were prescribed bisphosphonate to prevent osteoporotic fractures. Although the occurrence of AFF is rare, there are some concerns, such as a higher risk of delayed or non-union of AFF. This paper reviews the treatment of AFF and suggests some considerations during surgery.
-
Citations
Citations to this article as recorded by- How to Improve Fracture Healing in Atypical Femoral Fractures
Sang-Jin Jeong, Chan-Woo Park, Seung-Jae Lim
Journal of the Korean Orthopaedic Association.2024; 59(1): 9. CrossRef - Atypical Femoral Fracture Occurring at a Proximal Screw Insertion Site after Plate Removal in a Distal Femoral Fracture
Jin Woo Jin, Sung Jin Shin, Jong Min Jeon
Journal of the Korean Orthopaedic Association.2024; 59(4): 314. CrossRef - Position Statement: Atypical Femoral Fracture from the Korean Society for Bone and Mineral Research in 2023
Jae-Hwi Nho, Byung-Woong Jang, Dong Woo Lee, Jae-Hyun Kim, Tae Kang Lim, Soo Min Cha, Dong-Kyo Seo, Yong-Geun Park, Dong-Geun Kang, Young-Kyun Lee, Yong-Chan Ha
Journal of Bone Metabolism.2023; 30(3): 209. CrossRef
- How to Improve Fracture Healing in Atypical Femoral Fractures
- 581 View
- 5 Download
- 3 Crossref

Case Report
- Arthroscopic Assisted Bioabsorbable Screw Fixation for Radial Head Fractures: A Report of Two Cases
- Bong Ju Park, Ki Yong An, Yong Suk Choi
- J Korean Fract Soc 2017;30(1):35-39. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.35
-
 Abstract
Abstract
 PDF
PDF - Most radial head fractures occur as the result of low-energy mechanisms, such as a trip or fall on the outstretched hand. These fractures typically occur when an axial load is applied to the forearm, causing the radial head to hit the capitellum of the humerus. Good results are shown with nonsurgical treatments for Mason type 2 fractures. However, if there is a limitation of elbow joint exercise or displacement of more than 2 mm, an operative treatment should be considered. We treated two patients with arthroscopic assisted bioabsorbable screw (K-METâ„¢; U&I Corporation, Uijeongbu, Korea) fixation for radial head fractures to prevent complications of open reduction and minimize radiation exposure.
-
Citations
Citations to this article as recorded by- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
Woo-Jin Shin, Young-Woo Chung, Ki-Yong An, Jae-Woong Seo
Journal of Korean Foot and Ankle Society.2018; 22(4): 181. CrossRef
- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
- 690 View
- 3 Download
- 1 Crossref

Original Articles
- Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
- Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
- J Korean Fract Soc 2016;29(3):185-191. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.185
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To introduce the technique of reducing displaced or comminuted clavicle shaft fracture using composite wiring and report the clinical results.
MATERIALS AND METHODS
Between March 2006 and December 2013, 31 consecutive displaced clavicle fractures (Edinburgh classification 2B) treated by anatomic reduction and internal fixation using composite wiring and plates were retrospectively evaluated. The fracture fragments were anatomically reduced and fixed with composite-wiring. An additional plate was applied. Radiographic assessments for the numbers of fragments, size of each fragment and amount of shortening and displacement were performed. The duration for fracture union and complications were investigated retrospectively. The mean fallow-up duration was 15.9 months.
RESULTS
The mean number of fragments was 1.7 (1-3) and the mean width of fracture fragment was 7.1 mm (4.5-10.6 mm). The mean shortening of the clavicle was 20.5 mm (10.3-36.2 mm). The mean number of composite wires used in fixation was 1.9 (1-3). Radiographic union was achieved in all patients with a mean time to union of 11.6 weeks. There were no complications including metal failure, pin migration, nonunion, or infection.
CONCLUSION
The composite wiring was suitable for fixation of small fracture fragment and did not interfere with the union, indicating that it is useful for treatment of clavicle shaft fracture.
- 374 View
- 1 Download

- Orthogonal Locking Compression Plate Fixation for Distal Humeral Intraarticular Fractures
- Hyoung Keun Oh, Suk Kyu Choo, Kyoung Hwan Koh, Ji Woong Yeom
- J Korean Fract Soc 2016;29(3):178-184. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.178
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the surgical outcomes of orthogonal locking compression plate fixation for distal humeral intraarticular fractures.
MATERIALS AND METHODS
This study included 18 patients presenting a distal humeral intraarticular fracture who were treated with orthogonal locking compression plate fixation. According to the AO/OTA classification, there were eight C2 and ten C3 fractures. We evaluated radiologic outcomes, clinical results with range of motion, operation-related complications, and functional score by Mayo elbow performance score (MEPS).
RESULTS
The a verage u nion t ime was 3.5 months, and there was no c ase of r eduction l oss of a rticular f racture at t he last follow-up. Additional surgical procedures were needed in the three cases of C3 fractures. There was one case of heterotrophic ossification and one case of K-wire irritation. The average range of motion of elbow joint was 7° to 122°, and functional results were graded as 14 excellent, three good, and one fair by MEPS.
CONCLUSION
Anatomical reduction and internal fixation with orthogonal locking compression plate could provide satisfactory surgical outcomes for the treatment of distal humeral intraarticular fracture.
- 420 View
- 0 Download

- Hypoesthesia after Open Reduction and Plate Fixation of Clavicular Midshaft Fractures: Correlation with Plate Location and Clinical Features of Hypoesthesia
- Seong Hun Kim, Joon Yub Kim, Kyoung Hwan Koh, Myung Gon Jung, Jae Ho Cho
- J Korean Fract Soc 2016;29(2):121-127. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.121
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study is to evaluate the correlation between the location of the plate and the incidence of clavicular hypoesthesia and the clinical features of patients with clavicular hypoesthesia after open reduction and internal fixation of clavicular midshaft fractures.
MATERIALS AND METHODS
Seventy-eight patients who underwent open reduction and plate fixation for clavicle midshaft fractures between March 2013 and October 2014 were assessed for eligibility. The total clavicular length (A), the distance to the medial end of the plate from the sternoclavicular joint (B), and the distance to the lateral end of the plate from the sternoclavicular joint (C) were measured. Correlation between the location of the clavicular plate and the incidence of clavicular hypoesthesia was evaluated. In addition, the severity, and recovery of hypoesthesia were evaluated. Patient satisfaction, pain visual analogue scale were evaluated regarding hypoesthesia.
RESULTS
The incidence of hypoesthesia was 32.1% (25/78 patients). No correlation was observed with respect to the location of the clavicular plate and the incidence of clavicular hypoesthesia (p=0.666 at the medial end, p=0.369 at the lateral end). Recovery from hypoesthesia was observed in 23 out of 25 patients (p=0.008). Patient satisfaction and pain showed negative correlation with the incidence of hypoesthesia (p=0.002 and p=0.022).
CONCLUSION
There was no correlation between clavicular hypoesthesia and the plate location. Although most cases of hypoesthesia were recovered, we should try to avoid hypoesthesia due to the negative 'correlation' with patient satisfaction and pain.
- 488 View
- 0 Download

- The Usefulness of Poller Screw with Antegrade Nailing in the Initial Treatment of Infraisthmal Femur Shaft Fracture
- Jeong Hyun Yoo, Hyoung Soo Kim, Chang Geun Kim, Ho Il Kwak, Sang Heon Song
- J Korean Fract Soc 2015;28(4):230-236. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.230
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the radiologic and clinical outcomes after intramedullary nailing with Poller screw insertion at initial stage in infraisthmal femur shaft fractures.
MATERIALS AND METHODS
Seven consecutive patients (7 femurs) treated with antegrade intramedullary nailing with Poller screw insertion for the infraisthmal femur shaft fracture were reviewed retrospectively. There were 4 male and 3 female patients. Mean age was 46.1 years (20-72 years). Operative time including Poller screw insertion, time for union, malalignment, and range of motion were evaluated.
RESULTS
All 7 cases had primarily healed successfully. Mean time for radiologic union was 19.1 weeks (16-24 weeks) postoperatively. One case had 5 degree valgus malalignment. One case of 15 mm shortening was reported and he required shoe lift orthosis. All cases had a full range of motion in hip and knee joint.
CONCLUSION
Antegrade intramedullary nailing with Poller screw insertion is useful in the initial treatment of infraisthmal femur shaft fracture, because it could provide additional stability. An additional 20 minutes were required but a Poller screw should be considered according to the anatomic location of a femur shaft fracture.
- 514 View
- 4 Download

- Steinmann Pin Assisted Reduction of Subtrochanteric Femoral Fracture
- Seung Wan Lim, Oog Jin Shon
- J Korean Fract Soc 2015;28(1):17-22. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.17
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Nail insertion is the treatment of choice for subtrochanteric femoral fracture, but displacement of proximal bone fragment makes it difficult to find an ideal entry point. Therefore, in this study we aimed to determine the usefulness of treatment of subtrochanteric femoral fracture using Steinmann pin assisted reduction, internal fixation, and insertion of intramedullary nails.
MATERIALS AND METHODS
We evaluated 33 patients who were followed-up more than a year with a displaced subtrochanteric femoral fracture treated with closed reduction and intramedullary nail fixation between January 2008 and March 2013. In addition, we studied postoperative bone union time, postoperative reduction status, change of the femur neck shaft angle, evaluation of hip joint function, return to daily life, and complications.
RESULTS
All fractures with Steinmann pin assisted reduction were united but they included three cases of delayed union. In Fogagnolo classification, all cases were up to acceptable states and the varus change of femur neck shaft angle was 0.94degrees+/-3.1degrees; no significant difference in Harris hip score was observed between preoperative and last follow-up (p>0.05).
CONCLUSION
There were satisfactory results in bone union and reduction state with Steinmann pin assisted reduction. Therefore, Steinmann pin assisted reduction is a useful surgical technique for subtrochanteric femoral fracture. -
Citations
Citations to this article as recorded by- Percutaneous acetabular anchoring pin-assisted cephalomedullary nailing for subtrochanteric and unstable intertrochanteric fractures
Keong-Hwan Kim, Youngsik Yoon, Eic Ju Lim
Injury.2020; 51(3): 769. CrossRef
- Percutaneous acetabular anchoring pin-assisted cephalomedullary nailing for subtrochanteric and unstable intertrochanteric fractures
- 934 View
- 16 Download
- 1 Crossref

- A Retrospective Comparative Study of Internal Fixation with Reconstruction Plate Versus Anatomical Locking Compression Plate in Displaced Intercondylar Fractures of Humerus
- Tong Joo Lee, Young Tae Kim, Dae Gyu Kwon, Ju Yong Park
- J Korean Fract Soc 2014;27(4):294-300. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.294
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the clinical result of a conventional reconstruction plate (CRP) fixation and locking compressive plate (LCP) fixation on the surgical treatment of an adult's displaced intercondylar fracture of humerus.
MATERIALS AND METHODS
A total of 40 patients enrolled in the study were treated between August 2002 and May 2012. Fixation with a CRP was performed in 20 patients (group A) and anatomical locking compression plate fixation was performed in 20 patients (group B). The clinical and functional evaluation was performed according to the Mayo elbow performance score and Cassebaum classification of elbow range of motion (ROM), disabilities of the arm, shoulder and hand score.
RESULTS
The Mayo elbow functional evaluation scores, eight cases were excellent, 10 cases were good, and two cases were fair in group A, and 12 cases were excellent, seven cases good, and one case fair in group B; both groups showed satisfactory results. The durations of attaining 90 to 120 degrees of the ROM of joints postoperatively were 8.3 days on average (6 to 15 days) in group A and 5.5 days on average (5 to 9 days) in group B, demonstrating a significant difference between the two groups (p=0.04). Although the correlations of clinical results according to the difference of bone mineral densities (BMDs) were not statistically significant between the two groups (p=0.35), loss of fixation occurred due to loosening of screws in two patients with low BMDs in whose operations reconstruction plates were used.
CONCLUSION
The use of locking compressive plate on the surgical treatment of an diaplaced intercondylar fracture of humerus have a good clinical results because that permits early rehabilitation through good fixation and reduces the complications such as loosening of screws.
- 413 View
- 0 Download

- Treatment of Humeral Shaft Fracture with Retrograde Intramedullary Nail
- Ki Bum Choi, Soo Hwan Kang, Yoon Min Lee, Seok Whan Song, Youn Jun Kim
- J Korean Fract Soc 2013;26(4):299-304. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.299
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to report the outcome of treatment of humeral shaft fracture with retrograde intramedullary nail of advanced insertion opening.
MATERIALS AND METHODS
From April 2005 and August 2012, 22 patients with a humeral shaft fracture were treated by a single surgeon using the technique of retrograde intramedullary nail at Department of Orthopedic Surgery, Yeouido St. Mary's Hospital (Seoul, Korea). To avoid causing fractures at the insertion site, the entry point was more distally located than conventionally, and was extended proximally to include the proximal marginal cortex of the olecranon fossa. The outcome was evaluated clinically and radiologically.
RESULTS
The mean period of achievement of bony was 5.8 months (4-11 months). Additional fixations were needed in one patient with intraoperative lateral condylar fracture and 2 patients with postoperative nonunion. There were no limitations of movement or pain in the shoulder joint, and 8 cases had a 6.5degrees flexion contracture on average.
CONCLUSION
This retrograde intramedullary fixation technique using a distal entry portal near the olecranon fossa is particularly useful in humeral shaft fractures without a neurovascular injury. The risk of an intraoperative fracture (supracondylar fracture or fracture around the entry portal) can be decreased using this treatment. We recommend this technique because of the safety and the satisfactory outcome. -
Citations
Citations to this article as recorded by- HEALING PATTERN OF INTERLOCKED INTRAMEDULLARY NAILED HUMERAL SHAFT FRACTURE
Myung-Sang Moon, Dong-Hyeon Kim, Min-Geun Yoon, Sang-Yup Lee
Journal of Musculoskeletal Research.2016; 19(04): 1650018. CrossRef
- HEALING PATTERN OF INTERLOCKED INTRAMEDULLARY NAILED HUMERAL SHAFT FRACTURE
- 796 View
- 2 Download
- 1 Crossref

- The Character of Reverse Obliquity Intertrochanteric Fractures in Elderly Patients
- Ji Wan Kim, Jae Suk Chang, Jung Hwan Sung, Jung Jae Kim
- J Korean Fract Soc 2013;26(3):173-177. Published online July 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.3.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To discriminate the characteristics between reverse obliquity fractures in the elderly and that of young adults using three-dimensional computed tomography (3D CT).
MATERIALS AND METHODS
Eighteen patients who had reverse obliquity intertrochanteric fractures were enrolled from January 2007 to March 2012. The fracture pattern was analyzed using the 3D CT. The area showing low density (bone defect) of trochanter and femoral neck region was measured. Patients were divided into two groups: Group I, less than 65 years old and Group 2, 65 years and over.
RESULTS
In all 9 cases of group 1, the proximal fragment had a 'V' shape with an average of 5.6 cm below the vastus ridge; however, the fracture of 8 cases (88.97%) in group 2 had a 'Lambda' shape of the distal fragment at the level of vastus ridge and an additional fracture line extending to the greater trochanter tip. The bone defect volume of the trochanter and femoral neck region was larger significantly in group 2 than in group 1.
CONCLUSION
Reverse obliquity intertrochanteric fracture in the elderly demonstrated a pattern of bursting fracture with 4 parts, which had different patterns from that of young patients. We believe that the larger volume of bone defects resulted in the difference of fracture patterns between the two groups. -
Citations
Citations to this article as recorded by- A Comparison of Internal Fixation and Bipolar Hemiarthroplasty for the Treatment of Reverse Oblique Intertrochanteric Femoral Fractures in Elderly Patients
Bong-Ju Park, Hong-Man Cho, Woong-Bae Min
Hip & Pelvis.2015; 27(3): 152. CrossRef
- A Comparison of Internal Fixation and Bipolar Hemiarthroplasty for the Treatment of Reverse Oblique Intertrochanteric Femoral Fractures in Elderly Patients
- 791 View
- 9 Download
- 1 Crossref

Case Report
- Surgical Management of Comminuted Avulsion Fracture of the Proximal Fibula with Lateral Collateral Ligament Injury: Technical Note
- Jong Min Kim, Byeong Mun Park, Sang Hoo Lee, Seung Ju Jeon, Jun Beum Shin, Kyeong Seop Song
- J Korean Fract Soc 2013;26(1):77-80. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.77
-
 Abstract
Abstract
 PDF
PDF - Anteromedial force to the knee in an extended position can cause an avulsion fracture of the proximal fibula with combined injuries to the posterolateral ligaments. Avulsion fractures of the proximal fibula are rare and current management of these fractures is based on few descriptions in literature. Various surgical methods of fixation for these fractures have been reported, but there is still no standard treatment modality. Anatomic reduction of these fractures is technically difficult, and failure of reduction may cause posterolateral instability, secondary arthritis and other complications. We present our experience with two such cases of comminuted avulsion fractures of the proximal fibular with posterolateral ligament ruptures surgically fixated with a locking compression hook plate and non absorbable sutures.
-
Citations
Citations to this article as recorded by- Fixation of fibular head avulsion fractures with the proximal tibiofibular screw: Technique guide and clinical experience
Ryan A. Paul, Shu Yang Hu, Ananya Pathak, Ryan Khan, Daniel B. Whelan
Trauma Case Reports.2025; 57: 101175. CrossRef - Treatment of avulsion fractures around the knee
Jeong-Hyun Koh, Hyung Keun Song, Won-Tae Cho, Seungyeob Sakong, Sumin Lim
Journal of Musculoskeletal Trauma.2025; 38(2): 63. CrossRef - Treatment of Avulsion Fractures around the Knee
Sumin Lim
Journal of the Korean Fracture Society.2024; 37(2): 117. CrossRef
- Fixation of fibular head avulsion fractures with the proximal tibiofibular screw: Technique guide and clinical experience
- 1,277 View
- 27 Download
- 3 Crossref

Original Articles
- Intermittent Parathyroid Hormone Treatment for Stimulation of Callus Formation in Elderly Patients
- Hyung Keun Song, Sung Jun Kim, Jae Hoo Lee, Kyu Hyun Yang
- J Korean Fract Soc 2012;25(4):295-299. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.295
- Correction in: J Musculoskelet Trauma 2013;26(2):170
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the effect of parathyroid hormone (PTH) on fracture healing in elderly patients.
MATERIALS AND METHODS
We analyzed the radiologic results in 14 patients. Group I (n=7) was administrated intermittent PTH after surgical treatment and group II (n=7) was treated only with surgery. We checked the time of initial callus formation, bridging callus formation, and bone union through periodic follow-up radiographs by a radiologist who did not know the patient's information.
RESULTS
The mean time to initial callus formation was 6 weeks for group I, compared with 6.7 weeks for group II. The mean time to bridging callus formation was 15.9 weeks for group I, compared with 23.0 weeks for group II. The mean time to bone union was 28.7 weeks for group I, compared with 41.9 weeks for group II. The difference in the cumulative detection rate (CDR) of the initial callus formation of group I and II was not statistically significant (p=0.793). However, the CDR of the bridging callus formation and bone union for group I were higher than those of group II (p=0.008, p=0.001, respectively).
CONCLUSION
The intermittent PTH administration after surgical treatment and maximum possible preservation of the periosteum in elderly patients accelerates fracture healing. -
Citations
Citations to this article as recorded by- Advances in Parathyroid Hormone-based medicines
Anne-Laure Bonnet, Lizaveta Aboishava, Michael Mannstadt
Journal of Bone and Mineral Research.2025; 40(11): 1195. CrossRef - Effects of Extracts from Cnidium officinale and Angelica sinensis on Bone Fusion in Mice with Femoral Fracture
Sang Woo Kim, Min-Seok Oh
Journal of Korean Medicine Rehabilitation.2024; 34(2): 1. CrossRef - Timing of osteoporosis therapies following fracture: the current status
Rajan Palui, Harsh Durgia, Jayaprakash Sahoo, Dukhabandhu Naik, Sadishkumar Kamalanathan
Therapeutic Advances in Endocrinology and Metabolism.2022;[Epub] CrossRef - Effect of Postoperative Parathyroid Hormone Administration on Osteoporotic Intertrochanteric Fractures of Females
Hyun Cheol Oh, Ju Hyung Yoo, Joong Won Ha, Yung Park, Sang Hoon Park, Han Kook Yoon
Journal of the Korean Orthopaedic Association.2020; 55(3): 237. CrossRef - The role of teriparatide in tuberosity healing after reverse shoulder arthroplasty in complex proximal humeral fragility fracture
Bancha Chernchujit, Renaldi Prasetia
Journal of Orthopaedic Surgery.2018;[Epub] CrossRef - Bone Substitutes and the Advancement for Enhancing Bone Healing
Dong-Hyun Lee, Ji Wan Kim
Journal of the Korean Fracture Society.2017; 30(2): 102. CrossRef - Current Role and Application of Teriparatide in Fracture Healing of Osteoporotic Patients: A Systematic Review
Sang-Min Kim, Kyung-Chung Kang, Ji Wan Kim, Seung-Jae Lim, Myung Hoon Hahn
Journal of Bone Metabolism.2017; 24(1): 65. CrossRef - The Effect of Teriparatide on Fracture Healing of Osteoporotic Patients: A Meta-Analysis of Randomized Controlled Trials
Shenghan Lou, Houchen Lv, Guoqi Wang, Licheng Zhang, Ming Li, Zhirui Li, Lihai Zhang, Peifu Tang
BioMed Research International.2016; 2016: 1. CrossRef - A systematic review on the use of daily subcutaneous administration of teriparatide for treatment of patients with osteoporosis at high risk for fracture in Asia
J.F. Chen, K. H. Yang, Z.L. Zhang, H.C. Chang, Y. Chen, H. Sowa, S. Gürbüz
Osteoporosis International.2015; 26(1): 11. CrossRef
- Advances in Parathyroid Hormone-based medicines
- 737 View
- 8 Download
- 9 Crossref

- Alteration of the Patella Tendon Length after Intramedullary Nail in Tibial Shaft Fractures
- Dong Eun Shin, Ki Shik Nam, Jin Young Bang, Ji Hoon Chang
- J Korean Fract Soc 2012;25(4):283-287. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.283
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare and analyze length change of patella tendon after intramedullary nailing of tibial shaft fracture using transtendinous approach.
MATERIALS AND METHODS
Thirty-two cases were analyzed from December, 1999 to December, 2005. Insall Salvati ratios were estimated. Severity of initial trauma, duration of nail retension, knee function and pain on change of length of patellar tendon was evaluated.
RESULTS
Mean duration of nail retention was twenty-two months. The shortening of patella tendon was observed in 25 cases (p<0.001). The effect of AO type and the duration of nail retension on the decrease of Insall Salvati ratio was not significant (p>0.05, p=0.778). Lysholom score decrease to 89.5. There was no significant difference between the shortening of patellar tendon length and knee pain (p=0.058).
CONCLUSION
After intramedullary nailing for closed tibia fracture, shortening of patellar tendon length is observed. That is irrelevant to the fracture type and the duration of nail retension. The shortening of patella tendon length may contribute to decreasing of knee function, but it was no significance of knee pain after intramedullary nailing.
- 513 View
- 0 Download

- Operative Treatment in the Delayed Diagnosed Fracture and Dislocation of Hamatometacarpal Joint
- Suk Ha Lee, Jong Wong Park, Jin Il Kim, Seoung Joon Lee
- J Korean Fract Soc 2011;24(3):249-255. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.249
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose is to evaluate and report the results that treated with open reduction and internal fixation in delayed diagnosed fracture and dislocation of the hamatometacarpal joint.
MATERIALS AND METHODS
We evaluated 12 cases that had been treated with open reduction and internal fixation in delayed diagnosed fracture and dislocation of the hamatometacarpal joint. The mean interval between injury and operation was 34 days (21~60 days), the mean age of 12 cases was 28.1 years old, and mean follow-up period was 18 months. The computer tomography was done in all cases and the fracture and dislocation types were classified by Cain's classification. For the evaluation of results, pain scale, grasping power, range of motion of wrist and metacarpophalangeal joint were analyzed preoperatively and at final follow up, and the arthritic change of the hamatometacarpal joint was also checked.
RESULTS
According to Cain's classification, type Ia was one case, type Ib was two, type II was six, and type III was three. The pain scale was improved from 7.75 preoperatively to 0.92 at last follow up. The mean grasping power was improved up to 97.5% of normal. The preoperative range of motion of the wrist joint measured to be 60 degrees in extension and 70 degrees in flexion; the final range of motion indicated to be 75 degrees in extension and 80 degrees in flexion. The preoperative range of motion of the metacarpophalangeal joint measured to be 0 degrees in extension and 70 degrees in flexion; the final range of motion indicated to be 0 degrees in extension and 85 degrees in flexion. Carpometacarpal arthritis was developed in two cases.
CONCLUSION
The open reduction and internal fixation is considered as one of good treatment option in the delayed diagnosed hamatometacarpal fracture and dislocation. -
Citations
Citations to this article as recorded by- Reliability of classification of ring and little finger carpometacarpal joint fracture subluxations: a comparison between two-dimensional computed tomography and three-dimensional computed tomography classifications
J. H. Kim, S.-S. Kwon, S. J. Moon, J. S. Choe, H. I. Kwak, S. Y. Lee, H. J. Le, J. Y. Kim
Journal of Hand Surgery (European Volume).2016; 41(4): 448. CrossRef - Fourth and Fifth Metacarpal Base Arthrodesis for Posttraumatic Arthritis of Fifth Carpometacarpal Joint
Chul-Hyung Kang, Eun-Sok Son, Chul-Hyun Cho
Journal of the Korean Society for Surgery of the Hand.2013; 18(4): 184. CrossRef
- Reliability of classification of ring and little finger carpometacarpal joint fracture subluxations: a comparison between two-dimensional computed tomography and three-dimensional computed tomography classifications
- 703 View
- 1 Download
- 2 Crossref

- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
- Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
- J Korean Fract Soc 2011;24(3):217-222. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.217
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the results of intertrochanteric fractures treatment with proximal femoral nail antirotation (PFNA) without using fracture tables and thereby prevent complications.
MATERIALS AND METHODS
Forty cases of intertrochanteric fracture of 39 patients that were treated with PFNA without using fracture tables between January 2008 to December 2009 were analyzed. There were 13 males and 27 females. The mean age was 76 years old. Using AO classification, 6 cases were A1, 25 cases were A2 and 9 cases were A3. The operation was done without using fracture tables at supine position. Operation time, intraoperative bleeding were checked. For the result, Cleveland index, tip apex distance, fracture site sliding rate, change of femur neck and shaft angle were evaluated. Bone union time and complications were also estimated from the follow up radiograph. Statistics were analyzed using Independent T-test.
RESULTS
The mean operation time was 40 minutes (25 to 70 minutes) and mean intraoperative bleeding was 113 cc (40 to 250 cc). The Cleveland index was shown 94% of 5, 6, 8 and 9 zone, the tip apex distance was 12.96 mm (6 to 22 mm), the fracture sliding distance was 1.9 mm (0 to 6 mm), the change of femur neck and shaft angle was 2.5 degree (0~10 degree) and the average bone union time was 15 weeks (8 to 24 weeks). The complication include 2 cases of delayed union and 2 cases of varus deformities.
CONCLUSION
We have shortened the operation time by closed reduction methods without using the fracture tables, and the complication were minimized with using simple tools like a reduction forcep or bone hook at PFNA blade insertion. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
Journal of the Korean Fracture Society.2013; 26(4): 284. CrossRef
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- 780 View
- 2 Download
- 2 Crossref

- Does Interfragmentary Cerclage Wire Fixation in Clavicle Shaft Fracture Interfere the Fracture Healing?
- Jae Kwang Yum, Yong Woon Shin, Hee Sung Lee, Jae Gu Park
- J Korean Fract Soc 2011;24(2):138-143. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.138
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
A technique of cerclage wire fixation in comminuted fracture of the clavicle shaft is thought to interfere the fracture healing, so authors studied radiographically and clinically about the cases of cerclage wiring of the fracture fragments with the plate and screws fixation in the comminuted fracture of the shaft of the clavicle.
MATERIALS AND METHODS
According to following inclusion criteria, total 18 patients (male: 15, female: 3) were investigated; Patients who visited hospital due to clavicle shaft comminuted fracture from February 2005 to April 2009, who underwent surgery utilizing more than 2 cerclage wire fixation for the fragments when open reduction and plate fixation were operated and who could be follow-up over one year. The duration for fracture union, functional outcome and complications were investigated retrospectively.
RESULTS
Radiological bone union was accomplished in average 13.3 weeks (12~16 weeks) and there was no complication such as nonunion, delayed union or infection. Range of motion of ipsilateral shoulder joint was recovered in all patients except one at the final follow-up.
CONCLUSION
The clinical and radiographical results of the plate and screws fixation with cerclage wiring of the fragments in comminuted clavicle shaft fracture showed that the cerclage wiring does not interfere the fracture healing, so authors think that this method is a good alternative operation if it is performed carefully to minimize soft tissue dissection. -
Citations
Citations to this article as recorded by- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
Kyung-Tae Kim, Chung-Shik Shin, Young-Chul Park, Dong-hyun Kim, Min-Woo Kim
Journal of the Korean Orthopaedic Association.2021; 56(3): 245. CrossRef - Supplementary Technique for Unstable Clavicle Shaft Fractures: Interfragmentary Wiring and Temporary Axial K-Wire Pinning
Jinmyoung Dan, Byung-Kook Kim, Ho-Jae Lee, Tae-Ho Kim, Young-Gun Kim
Clinics in Orthopedic Surgery.2018; 10(2): 142. CrossRef - Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
Journal of the Korean Fracture Society.2016; 29(3): 185. CrossRef - TO EVALUATE THE SURGICAL OUTCOME OF NON-UNION CLAVICLE USING PLATE AND SLIVERS OF AUTOLOGOUS ILIAC CREST CORTICOCANCELLOUS BONE GRAFT
Mohammed Tauheed, Shashi Kumar Yalagach, Vivek Purushothaman, Anwar Shareef Kunnath K
Journal of Evidence Based Medicine and Healthcare.2016; 3(25): 1121. CrossRef - Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
Kyoung Hwan Koh, Min Soo Shon, Seung Won Lee, Jong Ho Kim, Jae Chul Yoo
Journal of the Korean Fracture Society.2012; 25(4): 300. CrossRef
- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
- 862 View
- 0 Download
- 5 Crossref

- Effect of Fracture Gap on Biomechanical Stability of Compression Bone-Plate Fixation System after Bone Fracture Augmentation
- Duk Young Jung, Sung Jae Lee, Seon Chil Kim, Jong Keon Oh
- J Korean Fract Soc 2010;23(2):220-226. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.220
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The goal of this study using the biomechanical test was to evaluate the mechanical stability of the bone-plate fixation system according to changes of the fracture gap sizes and widths.
MATERIALS AND METHODS
For mechanical test, four types with different fracture models simulating the clinical situations were constructed depending on the gap size (FGS, mm) and the gap width (FGW, %) at the fracture site: 0 mm/0%, 1 mm/100%, 4 mm/100%, 4 mm/50%. For analyzing the effects of fracture gap on the biomechanical stability of the bone-plate fixation system, 4-point bending test was performed under all same conditions.
RESULTS
It was found that the fracture gap sizes of 1 and 4 mm decreased mechanical stiffness by about 50~60% or more. Furthermore, even without fracture gap size, 50% or more fracture gap width considerably decreased mechanical stiffness and suggested the possibility of plate damage through strain results.
CONCLUSION
Our findings suggested that at least 50% contact of the fracture faces in a fracture surgery would be maintained to increase the mechanical stability of the bone-plate fixation system.
- 662 View
- 5 Download

- Results of Osteoporotic Treatment Drug after Periarticular Fracture of Hip
- Soo Jae Yim, Young Koo Lee, Cheong Kwan Kim, Hyun Seok Song, Hee Kyung Kang
- J Korean Fract Soc 2010;23(2):167-171. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.167
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The Purpose of the study is to know patients' compliance of drug treatment of osteoporosis after operation of fracture and to compare of accompanying fractures between patients who diagnosed with osteoporosis itself and had the drug treatment of osteoporosis after surgery of periarticular fracture of hip.
MATERIALS AND METHODS
In experimental group, consecutive 60 patients who had fracture of femoral neck and trochanter. And in control group, 61 patients diagnosed osteoporosis with drug treatment within the same period in orthopedic department from July 2006 to July 2007. The average age is 73.8 (+/-6.7) year in experimental group, and 66.6 (+/-7.46) year in control group. Both groups had at least a year follow-up with drug treatment and had BMD again at least a year later.
RESULTS
BMD test in experimental group showed -3.05 (+/-1.35) preoperatively and -2.74 (+/-1.50) in last follow-up. BMD test in control group showed -3.55 (+/-0.52) in initial administration and -3.10 (+/-0.87) in last follow-up. The results showed a significant improvement in statistical analysis (p=0.0002, p<0.0001).
CONCLUSION
The compliance of drug treatment of osteoporosis after operation of periarticular fracture of hip is the same as in patients' diagnosed osteoporosis. -
Citations
Citations to this article as recorded by- Does the Time of Postoperative Bisphosphonate Administration Affect the Bone Union in Osteoporotic Intertrochanteric Fracture of Femur?
Yoon Je Cho, Young Soo Chun, Kee Hyung Rhyu, Joon Soon Kang, Gwang Young Jung, Jun Hee Lee
Hip & Pelvis.2015; 27(4): 258. CrossRef - Sequential Hip Fractures in Elderly Osteoporotic Patients
Soojae Yim, Yuseok Seo, Sanghyok Lee, Joonghyun Ahn
Hip & Pelvis.2012; 24(4): 309. CrossRef
- Does the Time of Postoperative Bisphosphonate Administration Affect the Bone Union in Osteoporotic Intertrochanteric Fracture of Femur?
- 619 View
- 0 Download
- 2 Crossref

- A Finite Element Analysis of Biomechanical Stability of Compression Plate Fixation System in according to Existing of Fracture Gap after Bone Fracture Augmentation
- Duk Young Jung, Bong Ju Kim, Jong Keon Oh
- J Korean Fract Soc 2010;23(1):83-89. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.83
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study using the finite element analysis (FEA) focused on evaluating the biomechanical stability of the LC-DCP in accordance with existing of the fracture gap at the facture site after bone fracture augmentation.
MATERIALS AND METHODS
For FEM analysis, total eleven types with different fracture models considering clinical fracture cases were constructed according to the fracture gap sizes (0, 1, 4 mm)/widths (0, 25, 50, 75, 100%). Limited contact dynamic compression plate (LC-DCP) fixation system was used in this FEM analysis, and three types of load were applied to the bone-plate fixation system: compressive, torsional, bending load.
RESULTS
The results in FEM analysis showed that the 1, 4 mm fracture gap sizes and 75% or more fracture gap widths increased considerably the peak von Mises stress (PVMS) both the plate and the screw under all loading conditions. PVMS were concentrated on the center of the LC-DCP bone-plate, and around the necks of screws.
CONCLUSION
Based on the our findings, we recommend at least 50% contact of the fracture faces in a fracture surgery using the compression bone-plate system. Moreover, if x-ray observation after surgery finds 100% fracture gap or 50% or more fracture gap width, supplementary measures to improve biomechanical stability must be taken, such as restriction of walking of the patient or plastering. -
Citations
Citations to this article as recorded by- Application of Patient-Specific 3D-Printed Orthopedic Splint for Bone Fracture in Small Breed Dogs
Kwangsik Jang, Eun Joo Jang, Yo Han Min, Kyung Mi Shim, Chunsik Bae, Seong Soo Kang, Se Eun Kim
Journal of Veterinary Clinics.2023; 40(4): 268. CrossRef
- Application of Patient-Specific 3D-Printed Orthopedic Splint for Bone Fracture in Small Breed Dogs
- 685 View
- 1 Download
- 1 Crossref

- Treatment of Failed Intertrochanteric Fractures to Maintain the Reduction in Elderly Patients
- Soon Yong Kwon, Hyun Woo Park, Sang Uk Lee, Soo Hwan Kang, Jae Young Kwon, Jung Hoon Do, Seung Koo Rhee
- J Korean Fract Soc 2008;21(4):267-273. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.267
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study was to evaluate and report the new method with a cement augmented screw fixation again to treat the failed intertrochanteric fracture in elderly which were treated with ordinary compression hip screw initially.
MATERIALS AND METHODS
From Mar. 1988 to May 2007, 10 patients (mean age 69 years) with the failed intertrochanteric fracture which were treated with initial hip screw, were treated with a cement augmented compression hip screw again. The mean follow-up after surgery was over 18 months. The cause of failure, the period upto the reoperation, the neck-shaft angle after the reoperation, the position of lag screw in the femoral head, and the degree of union at last follow-up were analyzed. The change in the functional hip capacity were evaluated by the classification of Clawson.
RESULTS
Causes of failure were superior cutting-out in 6 cases, cortical anchorage failure in 3, and nonunion in one case. The period upto the reoperation was average 7.8 months. Valgus reduction of average 5.7degrees was achieved, and the positions of lag screw were postero-inferior in 6 cases, center in 3, infero-center in one case. We obtained complete union in 9 cases. The functional outcome showed moderate in 6 cases, good in 3 and poor degree in one case.
CONCLUSION
Cement augmented compression hip screw treatment will possibly reduce cutting-out of screw and bring more stability in fixation for intertrochanteric fractures in old osteoporotic patients, as well, even in failed cases treated with initial compression hip screw, but proper selection of patients is important. -
Citations
Citations to this article as recorded by- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
So Young Kim
Journal of the Korean Fracture Society.2019; 32(2): 89. CrossRef
- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
- 712 View
- 1 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


