Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 35(4); 2022 > Article
- Original Article Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
-
Journal of Musculoskeletal Trauma 2022;35(4):162-168.
DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
Published online: October 31, 2022
- 3,639 Views
- 53 Download
- 2 Crossref
- 0 Scopus
Abstract
Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies.
Published online Oct 20, 2022.
https://doi.org/10.12671/jkfs.2022.35.4.162
Abstract
Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries using the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, respectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Additionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no significant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and shortening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies.
초록
목적
PFNA-II의 단점을 보완한 TFNA를 대퇴 전자간 골절에 적용하여 PFNA-II와 임상적 및 방사선학적 결과를 비교하였다.
대상 및 방법
PFNA-II 혹은 TFNA로 수술 받은 82명을 분석하였으며, 최소 1년 이상 추시가 가능했던 경우만 연구에 포함하였다. 방사선학적 결과 비교를 위해서 두 군의 골유합 여부, 경부의 단축 정도를 분석하였으며, 임상적으로는 재수술이 필요한 합병증의 빈도를 분석하였고, Koval score를 이용하여 수술 전후의 보행 기능을 평가하였다.
결과
PFNA-II 환자군에서 평균 추시기간은 22개월이었고, TFNA 환자군에서는 19개월이었다. 합병증은 PFNA-II군에서 대퇴 천공 2건, 내반 붕괴 1건으로 TFNA군의 대퇴 천공 1건보다 높은 모습을 보였으나, 통계적 유의성은 없었다(p=0.37). 또한 대퇴 경부의 단축 정도, 수술 후 보행기능의 감소 정도에서 TFNA군이 PFNA-II군보다 우수한 경향성을 보였으나 두 군 간 통계적 유의성은 없었다.
결론
TFNA와 PFNA-II 모두 양호한 결과를 보이며, 보행능력의 회복과 합병증 발생 빈도 및 대퇴 경부 단축 정도 측면에서 유의한 차이를 보이지 않아 두 기구 모두 대퇴골 전자간부 골절의 치료에 적절한 선택으로 판단된다.
Introduction
Femoral intertrochanteric fracture is a commonly observed fracture that occurs in 133 cases per 100,000 in Korea every year.1) Conservative treatment of femoral intertrochanteric fractures leads to a higher frequency of non-union and an increased mortality rate due to pneumonia or pressure ulcers from long-term bed rest compared to surgical treatment. Therefore, surgery is the gold standard treatment for femoral intertrochanteric fractures, and the surgical method of using an intramedullary nail is what is commonly used.2,3) The currently used intramedullary nails include the proximal femoral nail antirotation (PFNA; DePuy Synthes, Warsaw, IN, USA), Gamma3 nail (Stryker Trauma, Schönkirchen, Germany), and InterTAN (Smith & Nephew, Memphis, TN, USA); however, complications, such as cervical screw and blade cut-through as well as breakage of the nails, have also been reported.4,5) To reduce these complications, an antirotation helical blade, which allows for higher rotational stability of the femoral head and neck, is used in PFNA-II. Additionally, when the antirotation helical blade is inserted into the head, it can compress the surrounding bones, thereby increasing the fixation force and reducing the frequency of cut-out of the head. However, complications, including cut-out of the head and breakage of the intramedullary nail, are constantly observed in some patients.4,5,6) To reduce these complications, the trochanteric fixation nail-advanced (TFNA; DePuy Synthes, West Chester, PA, USA) was developed and approved for use in Korea in September 2018. TFNA was modified in general to reduce chronic pain and breakage of the intramedullary nail from cut-out of the head by the PFNA-II antirotation helical blade and lateral femoral stimulation by the protrusion of the antirotation helical blade. A set screw locking function was added, and the Lateral Relief Cut™ design of the intramedullary nail and the sloped surface design on the outer surface of the antirotation helical blade were used to reduce stimulation of the outer surface of the femur. Moreover, the Bump Cut™ design was newly added to the antirotation helical blade insertion hole to reduce the frequency of intramedullary nail breakage.7)
A titanium-molybdenum (Ti-Mo) alloy was used to increase the fatigue strength, and the curvature was increased for the overall shape of the intramedullary nail to be more anatomically suitable for Asians. In this study, we assessed and compared the functional and radiological outcomes of TFNA, which is an improved fracture fixation device compared to the previously used PFNA-II, in elderly patients with osteoporotic femoral intertrochanteric fracture.
Materials and Methods
1. Participants
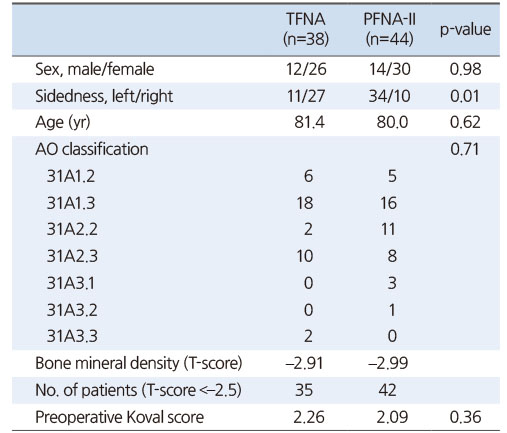
This was a single-center retrospective study and it was approved by the e-IRB (Institutional Review Board) of Inje University Haeundae Paik Hospital (No. 2020-02-035) and the informed consent was waived by the IRB. In this study, we used PFNA-II from January 2017 to October 2018 and consecutively used TFNA from November 2018 to September 2020 in patients aged 60 years or older who underwent intertrochanteric fracture surgery at our hospital. Eighty-two of 173 patients were enrolled, excluding 3 cases of pathological fractures, 9 cases of high energy injury and 79 cases of follow-up less than 1 year. A total of 38 and 44 cases of surgeries using TFNA and PFNA-II, respectively, were included in the final analysis. The mean follow-up period was 22.4 months (range, 14-43 months) and 19.3 months (range, 12-27 months) for the PNFA and TFNA groups, respectively.
Twelve male patients and 26 female patients were included in the TFNA group, while 14 male patients and 30 female patients were included in the PFNA-II group. There was no difference in the sex ratio between the two groups (p=0.98). In the TFNA group, the surgery was conducted on the left and right sides in 11 and 27 cases, respectively. In the PFNA-II group, the surgery was conducted on the left in 34 cases and the right in 10 cases. Therefore, the surgery was conducted more on the right side and the left side in the TFNA and the PFNA-II groups, respectively (p=0.01).
For the type of fractures, stable fractures (AO1.2 and AO1.3) accounted for 54.9% (45/82) of all cases, and there was no significant difference in the type of fracture between the two groups. The T-score of the lumbar spine or proximal femur obtained by dual energy X-ray absorptiometry were –2.91 and –2.99 in the TFNA and PFNA-II groups, respectively (Table 1).
Table 1
Demographic Factors and Fracture Characteristics of Patients in Both Groups
2. Evaluation method
The electronic medical records (EMR) of our hospital were searched to collect information including age, length of hospital stay, bone mineral density, and complications. Gait ability was assessed by the Koval score through EMR review and telephone interview. A score of 1 and 7 points indicated independent walking without an assistive device and incapability to walk, respectively, and gait ability was assessed in 7 different levels.8,9) Two orthopedic surgeons discussed and analyzed the images of the patients on the picture-archiving and communication system (PACS, Maroview 5.4; INFINITT Healthcare, Seoul, Korea) for the final review. Preoperative radiographs were analyzed according to the AO/OTA classification revised in 2018,10) and follow-up radiographs after surgery were analyzed to assess bone union, shortening of the femoral neck, and the tip to apex distance (TAD) of the intramedullary nail.11) Bone union was defined when cortical bone connectivity was observed in three directions in follow-up radiographs. Shortening of the femoral neck was assessed by measuring the change in length of the proximal femur on follow-up radiographs. Anteroposterior hip views were obtained at each follow-up period with neck anteversion neutralized by internal rotation of the thigh and image magnification was controlled using the length of the spiral blade of which the length was already known. The length of the proximal part of the femur was defined as the length of a line passing through the point bisecting the shortest width of the femoral neck among other lines connecting the shaft axis of the femur from the center of the femoral head.12) The stability of reduction was classified into anatomical, intramedullary and extramedullary reduction according to the degree of contact between the proximal and distal bone fragments at the fracture site.13) TAD was evaluated by observing the position of the femoral head blade in the pre- and postoperative anteroposterior and lateral radiographs.11) Fracture complications were defined as cases requiring repeat surgery due to reasons including femoral head cut-out, varus collapse, and infection.
In all surgeries, an antirotation helical blade was used for cervical fixation of the intramedullary nail. In the surgeries using TFNA, set screws were fixed in a completely static mode. Cement augmentation in the femoral head using insertion screws was not performed in all patients.
3. Statistical analysis
An independent t-test was conducted for each item after normality testing. If normality was not satisfied, the Mann–Whitney test was conducted. The chi-squared test was performed for nominal variables. Statistical analysis was conducted using the IBM SPSS Statistics (ver. 22.0.0; IBM Co., Armonk, NY, USA), and p<0.05 was considered statistically significant.
Results
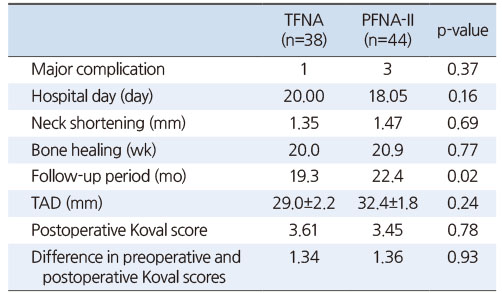
There was no significant difference in the reduction of fractures as anatomical 14 cases, intramedullary 3 cases, extramedullary 21 cases in the TFNA group, and anatomical 12 cases, intramedullary 5 cases, and extramedullary 27 cases in the PFNA-II group (p=0.23). Femoral neck shortening was 1.35 mm (range, 0-12.2 mm) in the TFNA group and 1.47 mm (range, 0-16.9 mm) in the PFNA-II group, with no significant difference between the two groups (p=0.69). TAD was 29.0 mm in the TFNA group and 32.4 mm in the PFNA-II group, and it was not significantly different between the two groups (p=0.24).
Bone union on radiographic findings was observed rather quickly within 20.0 and 20.9 weeks on mean in the TFNA and PFNA-II groups, respectively. There was no significant difference between the two groups (p=0.77).
The postoperative Koval score level was 3.61 and 3.45 in the TFNA and PFNA-II groups, respectively, and the difference between the pre and postoperative Koval score was 1.34 in the TFNA group and 1.36 in the PFNA-II group. There was no difference in the pre and postoperative Koval score in both groups (p=0.36 and p=0.78, respectively).
Complications were observed in 3 patients in the PFNA-II group and 1 patient in the TFNA group; however, there was no significant difference between the two groups (p=0.37). All 4 cases with loss of fracture reduction were intramedullary reduction.
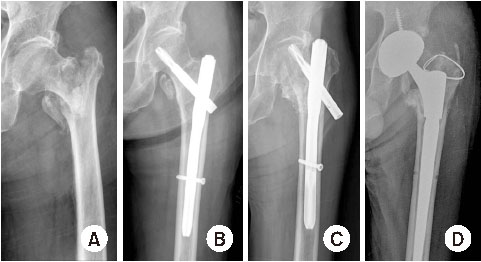
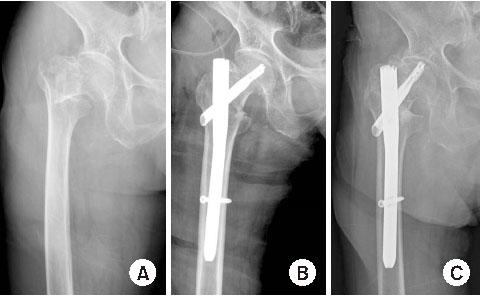
In the PFNA-II group, 2 cases of femoral head cut-out and 1 case of varus collapse were observed. Total hip arthroplasty was performed for the single case of varus collapse, and bipolar hemiarthroplasty was conducted in the 2 cases of femoral head cut-out (Fig. 1). In the TFNA group, 1 case of femoral head cut-out was observed. The patient was elderly, with a poor medical condition, and the family of the patient refused to undergo surgery. Hence, the patient was followed up regularly (Table 2,Fig. 2). No infection was observed in both groups.
Fig. 1
Postoperative complications of the PFNA-II system. (A) Preoperative radiography of a 76-year-old male patient with intertrochanteric fracture. (B) Postoperative radiography of the patient taken 24 months after surgery using PFNA-II. (C) Plain radiography showed the cut-out of the blade of the PFNA-II. (D) Conversion to total hip arthroplasty was performed.
Fig. 2
Postoperative complication of the TFNA system. (A) Preoperative radiography of a 84-year-old male patient with intertrochanteric fracture. (B) Postoperative radiography of the patient taken 11 months after surgery using TFNA. (C) Plain radiography showed the cut-out of the blade.
Table 2
Clinical and Functional Results
Discussion
For the intertrochanteric fractures, as enabling early movement through stable fixation of the fracture reduces the frequency of complications and promotes recovery, various devices have been developed for more stable fracture fixation.1) In particular, the proximal femoral nail helps to secure more stability in unstable fractures and stable intertrochanteric fractures.2,3,4) Even though it was impossible to minimize the shortening of the neck because the intramedullary nail such as PFNA-II does not have a mechanism that can effectively control the slide of the fractured area.12) Since it is possible to control the slide with the set screw function of the TFNA, it is expected that the shortening of the fracture will be prevented to some extent.
Kim and Shon14), who reported the treatment results of stable femoral intertrochanteric fractures using PFNA-II and Zimmer Natural Nail (ZNN), evaluated that the sliding distance tended to be small in ZNN with the set screw fixed. This supports the authors’ idea that set screw fixation will help prevent neck shortening.
Cut-out of the femoral head, which is a typical complication of using proximal femoral nails, is approximately 8%.15) In a computational study, the frequency of cut-out of the femoral head can be reduced by compressing the medullary bone inside the femoral head with an antirotation helical blade.16) Similar findings were observed in a biomechanical study.17) However, cut-out of the femoral head is still observed even when an antirotation helical blade is used,5) and two cases of femoral head cut-out requiring additional surgery were also observed in this study. In a study by Lenich et al.18), 120 cases were followed up for at least 6 months and femoral head cut-out was observed in 3 cases (2.3%). In a study of Korean participants using TFNA for intertrochanteric fractures, Yoon and Kim7) reported that femoral head cut-out was not observed in any of the 26 cases. Consistent with these results, this study shows that femoral head cut-out occurred in 1 in 38 cases when using TFNA. In all cases with cut-out observed in this study, the post-operative reduction was intramedullary position. As reported by Lee et al.19), varus reduction was achieved in 2 of 3 cases where cut-out occurred in the study using TFNA with helical blade. Therefore, reduction quality of fractures is considered to have an unyielding importance in the treatment of intertrochanteric fractures. In the TFNA group, there was no significant difference compared to what was observed in the PFNA-II group; however, the incidence of femoral head cut-out was low tendency.
Previous studies reported that excessive shortening of the femoral neck by 5 mm or more may impair gait function by reducing the gluteal muscle length and range of motion.20) The newly added set screw locking function to the TFNA system was expected to further preserve the length of the femoral neck; however, the difference in the postoperative length of the femoral neck between the two groups was not statistically significant.
To prevent breakage of the intramedullary nail, a Ti-Mo alloy (Ti-15Mo) was used for its greater fatigue strength than that of a titanium-6% aluminum-7% niobium alloy of PFNA. However, intramedullary nail breakage was not observed in both groups. Therefore, the effects of Ti-Mo alloy could not be further assessed.21) And Wallace et al.22) compared TFNA with other proximal femoral nails and confirmed that the proportion of nail breakages was equivalent.
The limitations of this study were as follows. First, a powerful statistical analysis was difficult due to the relatively small number of study subjects. And as a retrospective study, the follow-up period of the two groups was relatively short. In particular, the PFNA-II group had a significantly longer follow-up period than the TFNA group, which may have underestimated the frequency of complications and long-term prognosis in the TFNA group. Also, randomization of the study group was not performed.
Nevertheless, this study is considered meaningful in that it attempted to find out whether TFNA, developed by supplementing the shortcomings of PFNA-II, showed improved results by applying it to clinical practice.
Conclusion
PFNA-II and TFNA showed satisfactory clinical outcomes with no significant differences in elderly patients with femoral intertrochanteric fractures. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and shortening of the femoral neck were not different significantly, suggesting that both TFNA and PFNA-II are considered to be suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies.
Financial support:None.
Conflict of interests:None.
References
-
Bălţatu MS, Vizureanu P, Tierean MH, Minciună MG, Achiţei DC. Ti-Mo alloys used in medical applications. Adv Mat Res 2015;1128:105–111.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

