Search
- Page Path
- HOME > Search
Original Article
- Interpositional tricortical iliac bone graft in nonunion of midshaft clavicular fractures
- Eun-Seok Son, Bum-Soon Park, Chang-Jin Yon, Chul-Hyun Cho
- J Musculoskelet Trauma 2025;38(1):23-31. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00004
-
 Abstract
Abstract
 PDF
PDF - Background
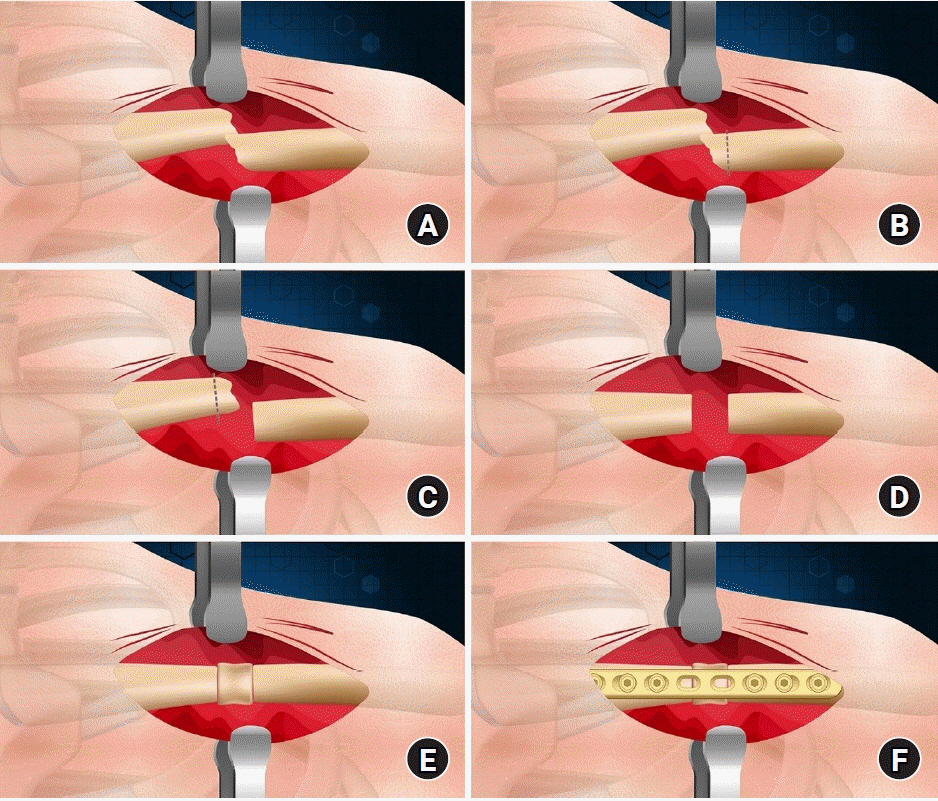
The purpose of this study was to investigate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures. Methods: Between 2007 and 2020, 17 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion combined with bone defect were investigated. The mean age was 53 years (range, 22–70 years). The mean follow-up period was 102.2 months (range, 18–193 months). Serial plain radiographs were used to evaluate radiological outcomes. The University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate clinical outcomes. Complications were also evaluated. Results: All cases achieved complete bony union with mean healing time of 17.6 weeks (range, 14–22 weeks). The mean clavicle length difference was significantly decreased from 9.1 mm preoperatively to 2.6 mm postoperatively (P<0.001). The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001), respectively. The mean final Quick-DASH score was 18.0. Three cases (17.6%) developed postoperative complications including two cases of shoulder stiffness and one case of screw irritation. Conclusions: Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length. Level of evidence: Level IV, case series.
- 2,026 View
- 44 Download

Case Report
- Rare Experience of Bilateral Femoral Neck and Shaft Fractures - A Case Report -
- DaeHyun Choe, Jae-Ho Lee, Ki-Chul Park
- J Korean Fract Soc 2020;33(3):154-158. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.154
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fractures of the femoral neck and shaft are relatively common injuries and accompany 2% to 9% of all femoral shaft fractures. On the other hand, it is extremely rare for these injuries to occur bilaterally. This paper reports the authors’ experience of a case with bilateral femoral neck and shaft fractures. The patient sustained multiple injuries, including liver laceration with hemoperitoneum, bilateral open fractures of the tibia, and bilateral femoral neck, and shaft fractures caused by a high-speed motor vehicle accident. Under the circumstances, damage-control orthopedic principles were applied, and external fixators were initially placed. After the patient’s general condition showed improvement, both femurs were fixed with a reconstruction nail. Fracture healing was achieved without complications, such as avascular necrosis of the femoral head. Despite the rare occurrence, this paper describes this case because these injuries must be managed with meticulous attention.
- 538 View
- 8 Download

Original Articles
- Analysis of the Changes in Femoral Varus Bowing and the Factors Affecting Nonunion for the Treatment of Femoral Shaft Fractures over 60 Years Old Using Piriformis Fossa Insertion Intramedullary Nailing
- Yonghan Cha, Chan Ho Park, Jun-Il Yoo, Jung-Taek Kim, WooSuk Kim, Ha-Yong Kim, Won-Sik Choy
- J Korean Fract Soc 2020;33(2):65-71. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.65
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the bony morphological changes to analyze the factors affecting bony union in the treatment of elderly femoral shaft fractures with varus bowing using piriformis fossa insertion intramedullary nailing.
Materials and Methods
This study included 26 patients over 60 years of age, who were admitted for femoral shaft fractures between January 2005 and December 2014 and treated with piriformis fossa insertion intramedullary nailing. Age, sex, height, weight, bone mineral density, injury mechanism, fracture type, diameter and length of the nail, postoperative lengthening of the femur, postoperative change in varus angle, contact between the lateral and anterior cortex, and the gap between the fracture line and the bony union were checked. The patients were divided into a varus group and nonvarus group, as well as a bone union group and nonunion group. Logistic regression analysis was performed to analyze the factors affecting nonunion.
Results
The patients were classified into 11 in the varus group and 15 in the non-varus group and 24 in the union group and 2 in the nonunion group. The varus group showed a larger increase in leg length and varus angle reduction than the non-varus group (p<0.05). The union group had more contact with the lateral cortical bone than that of the nonunion group (p<0.05). The factor affecting bone union in regression analysis was contact of the lateral cortical bone (p<0.05).
Conclusion
Treatment of a femoral shaft fracture in elderly patients with a varus deformity of the femur using piriformis fossa insertion intramedullary nail increases the length of the femur and decreases the varus deformity. For bony union, the most important thing during surgery is contact of the lateral cortical bone with the fracture site. -
Citations
Citations to this article as recorded by- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
Seong-Eun Byun, Young-Ho Cho, Young-Kyun Lee, Jung-Wee Park, Seonguk Kim, Kyung-Hoi Koo, Young Soo Byun
International Orthopaedics.2021; 45(12): 3223. CrossRef
- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
- 1,056 View
- 6 Download
- 1 Crossref

- Surgical Results of Minimally Invasive Percutaneous Plate Fixation in the Treatment of Clavicle Shaft Fracture
- Seong Ho Yoo, Suk Woong Kang, Jae Seung Seo
- J Korean Fract Soc 2019;32(1):21-26. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.21
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study analyzed the results of the midclavicle fracture treatment using the minimally invasive percutaneous plate osteosynthesis (MIPO) technique in a retrospective manner.
MATERIALS AND METHODS
Between March 2013 and March 2017, this study analyzed 40 patients who received MIPO surgery. Excluding 1 patient who underwent surgery on another body part injury, and 4 patients who were lost to follow-up over 1 year, 40 patients were analyzed for their operation time, bone union, functional American Shoulder and Elbow Surgeons score, scar lengths, pain relief (visual analogue scale), and complications.
RESULTS
All patients over a 1 year of follow-up achieved bone union, and American Shoulder and Elbow Surgeons score 97.6 (94–100) on their shoulder functional scores. Their average operation time was 42.7 minutes, and the average scar length was 6.1 cm. Eighteen patients successfully received metal removal using the previous scar without additional incision. The clavicle length was similar in the normal and operated group.
CONCLUSION
Despite its small sample size, clavicle fixation using the MIPO technique can be considered an effective treatment because of its limited number of complications, such as nonunion and rotational angulations. -
Citations
Citations to this article as recorded by- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
Woo Jin shin, Young Woo Chung, Seon Do Kim, Ki-Yong An
Clinics in Shoulder and Elbow.2020; 23(4): 205. CrossRef
- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
- 1,030 View
- 1 Download
- 1 Crossref

Case Report
- Avulsion of the Femoral Attachment of Anterior Cruciate Ligament Associated with Ipsilateral Femoral Shaft Fracture in Skeletally Mature Patient: A Case Report
- Seong Eun Byun, Taesup Kim, Bang Hyun Kim, Jae Hwa Kim, Soo Hong Han, Wonchul Choi
- J Korean Fract Soc 2016;29(3):200-205. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.200
-
 Abstract
Abstract
 PDF
PDF - Avulsion fracture at the femoral attachment of the anterior cruciate ligament (ACL) is very rare and has been reported mostly in skeletally immature patients. Authors experienced a case of avulsion fracture at the femoral attachment of ACL in a skeletally mature, a 21-year-old male associated with ipsilateral femoral shaft fracture. Here, authors report on the case with a literature review. Care should be taken because an avulsion fracture at the femoral attachment of ACL can be accompanied by ipsilateral femoral shaft fracture in skeletally mature patients.
- 452 View
- 0 Download

Original Articles
- Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
- Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
- J Korean Fract Soc 2016;29(3):185-191. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.185
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To introduce the technique of reducing displaced or comminuted clavicle shaft fracture using composite wiring and report the clinical results.
MATERIALS AND METHODS
Between March 2006 and December 2013, 31 consecutive displaced clavicle fractures (Edinburgh classification 2B) treated by anatomic reduction and internal fixation using composite wiring and plates were retrospectively evaluated. The fracture fragments were anatomically reduced and fixed with composite-wiring. An additional plate was applied. Radiographic assessments for the numbers of fragments, size of each fragment and amount of shortening and displacement were performed. The duration for fracture union and complications were investigated retrospectively. The mean fallow-up duration was 15.9 months.
RESULTS
The mean number of fragments was 1.7 (1-3) and the mean width of fracture fragment was 7.1 mm (4.5-10.6 mm). The mean shortening of the clavicle was 20.5 mm (10.3-36.2 mm). The mean number of composite wires used in fixation was 1.9 (1-3). Radiographic union was achieved in all patients with a mean time to union of 11.6 weeks. There were no complications including metal failure, pin migration, nonunion, or infection.
CONCLUSION
The composite wiring was suitable for fixation of small fracture fragment and did not interfere with the union, indicating that it is useful for treatment of clavicle shaft fracture.
- 374 View
- 1 Download

- Treatment of the Femoral Fracture Using Sirus(R) Nail: A Comparison of Complication according to the Entry Potal
- Young Yool Chung, Dong Hyuk Choi, Dae Hyun Yoon, Jung Ho Lee, Ji Hun Park
- J Korean Fract Soc 2015;28(2):103-109. Published online April 30, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.2.103
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the clinical results of fixation using Sirus(R) nail in patients with femoral subtrochanteric and shaft fracture and the difference in the frequency of complications according to the entry portal.
MATERIALS AND METHODS
From July 2006 to August 2013, at least 1-year clinical follow-up, we retrospectively analyzed 36 cases with femoral subtrochanteric (15 cases) and shaft fracture (21 cases) who underwent surgery using Sirus(R) nail. We reviewed the records of operation time, intra-operative amounts of bleeding and complications. At last follow-up, we reviewed clinical results by Ray-Sanders criteria and analyzed the periods of bone union on the radiograph. We also measured changing of the femoral neck-shaft angle in the subtrochanteric fractures and angulation in the shaft fractures, respectively. Considering anatomical variation of the trochanter and fracture position of subtrochanteric and femoral shaft, entry points were divided into subgroups, and the clinical results were compared.
RESULTS
The mean Ray-Sanders score was 27.4, 27 cases (75.0%) were good or excellent. The mean periods of bone union was 21.1 weeks in 31 cases. The mean neck-shaft angles were 135.7o preoperatively, 130.2o postoperatively. The mean angulation of the femur was 24.4o preoperatively, 2.4o postoperatively in patients of femoral shaft fractures. Despite no statistical significance, greater trochanter tip entry point and lateral entry point had a higher rate of frequency than medial entry point, with respect to the occurrence of iatrogenic fracture and malalignment.
CONCLUSION
Using Sirus(R) nail for femoral subtrochanteric and shaft fractures showed good clinical and radiographic results and a high rate of union. Medial entry point yielded slightly better results in the occurrence of iatrogenic fracture and malalignment, compared to greater trochanter tip entry point and lateral entry point.
- 627 View
- 3 Download

Case Report
- Failure to Remove a Trochanteric Entry Femoral Nail and Its Cause in Adolescent Patients: Two Cases Report
- Ji Hwan Kim, Seung Oh Nam, Young Soo Byun, Han Sang Kim
- J Korean Fract Soc 2015;28(1):71-76. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.71
-
 Abstract
Abstract
 PDF
PDF - Trochanteric entry femoral nails have been widely used for fixation of femoral shaft fractures because of easier identification of the entry point. Young patients usually request removal of the nail after healing of the fracture. We experienced a failure and difficulty in removal of the trochanteric entry nail in two adolescent patients. In the patient in which the nail could be removed with difficulty, dense compact bone was formed through the empty interlocking holes and the nail was held just like a latch. This finding was quite similar to the computed tomography findings of the patient in which the nail could not be removed. In order to remove the nail, the newly formed, dense compact bone in the interlocking holes must be broken and detached from the femur itself. We suggest that dense compact bone through the empty interlocking holes might be a clue for difficult removal of the trochanteric entry nail.
- 540 View
- 1 Download

Original Article
- Treatment for Concurrent Ipsilateral Femoral Neck and Shaft Fractures Using Reconstruction Nail with Temporary K-Wires
- Sang Joon Lee, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee
- J Korean Fract Soc 2015;28(1):23-29. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.23
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the results of operative treatment using a reconstruction nail after temporary K-wire fixation of the femoral neck for ipsilateral femoral neck and shaft fractures.
MATERIALS AND METHODS
A total of 11 cases were treated, which were followed-up for more than two years, between August 2007 and July 2012. The average age was 51 years (29-69 years) and men were dominant counting eight cases. All cases were operated with a reconstruction nail after temporary K-wire fixation of the femoral neck. Bone union periods, alignment, etc. were evaluated by radiological methods and accompanying damage and complications were also investigated. Functional evaluation was performed in accordance with Friedman and Wyman criteria at the last follow-up.
RESULTS
The average time for union of the femoral shaft was 22.5 weeks (12-32 weeks), and femoral neck was 13.1 weeks (8-20 weeks). There was no nonunion, and four femoral shaft fractures resulted in delayed union. There was one case of leg length discrepancy more than 2 cm long, but malalignment of more than 10 degrees was not observed. Avascular necrosis of the femoral head did not occur. Functional results were good in eight cases, fair in two cases, and poor in one case.
CONCLUSION
Treatment with reconstruction nailing after temporary K-wire fixation of the femoral neck is thought to be a good method which prevents neck displacement and has low complication rates.
- 662 View
- 6 Download

Case Report
- Chronic Osteomyelitis in Distraction Osteogenesis Area of Tibial Shaft: A Case Report
- Sanguk Bae, Baekyong Song, Jin Seon Moon
- J Korean Fract Soc 2014;27(4):321-326. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.321
-
 Abstract
Abstract
 PDF
PDF - Distraction osteogenesis with an Ilizarov external fixator is one of the most successful treatment options for large segmental bone defects after extensive debridement of chronic osteomyelitis in the tibial shaft. Its complications include skin irritation, pin tract infection, and non-union due to infection. There are few case reports on chronic osteomyelitis occurring in the distraction osteogenesis area. The authors experienced a chronic osteomyelitis in the distraction osteogenesis area of the tibial shaft and report this case with references.
- 592 View
- 9 Download

Original Articles
- Comparison of Greater Trochanter Versus Piriformis Entry Nail for Treatment of Femur Shaft Fracture
- Jong Hee Lee, Jong Hoon Park, Si Yeong Park, Seong Cheol Park, Seung Beom Han
- J Korean Fract Soc 2014;27(4):287-293. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.287
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to compare the clinical outcome of femoral shaft fracture treatment with intramedullary nailing performed using a greater trochanter and a piriformis entry nail.
MATERIALS AND METHODS
A total of 57 patients treated by antegrade nailing for a femoral shaft fracture between January 2008 and April 2013 were included in this study. We evaluated postoperative radiographs of 57 femoral shaft fractures stabilized with femoral intramedullary nailing at a single institutional center. The cases included 25 piriformis fossa entry nails and 32 greater trochanter entry nails. Outcome measures included the alignment, union rate and duration of union, complications, operation time, intra-operative bleeding, and a pain rating scale.
RESULTS
The alignment, union rate, and duration of union did not differ significantly between the groups with piriformis fossa and trochanteric nailing. In addition, no significant differences regarding complications and operation time were observed between the two groups. Less intra-operative bleeding was observed in the trochanteric nailing group. This difference was statistically significant (p=0.044).
CONCLUSION
Use of a femoral nail specially designed for the trochanteric insertion resulted in equally high union rates, duration of union, and low complication rates. Thus, greater trochanter entry nails were similar to conventional antegrade femoral nailing through the piriformis fossa.
- 710 View
- 0 Download

- Associated Factors of Radial Nerve Palsy Combined with Humerus Shaft Fracture
- Si Wuk Lee, Chul Hyun Cho, Ki Choer Bae
- J Korean Fract Soc 2014;27(3):185-190. Published online July 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.3.185
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to analyze associated factors of primary radial nerve palsy and to evaluate clinical outcome for its treatment in patients with humerus shaft fracture.
MATERIALS AND METHODS
We divided two groups of patients with (17 patients) and without (116 patients) primary radial nerve palsy and analyzed correlation between radial nerve injury and various parameters, including age, sex, cause of injury, AO classification, fracture type, fracture location, and presence of open fracture. We also evaluated configuration of nerve injury, presence of recovery, and recovery time.
RESULTS
The overall prevalence of primary radial nerve palsy after humerus shaft fracture was 12.8% (17 palsies in 133 fractures). Younger age, AO type B, and distal 1/3 fractures showed significantly higher correlation with radial nerve palsy. No significant correlation was observed between radial nerve palsy and other parameters, including sex, cause of injury, fracture type, and presence of open fracture. Thirteen patients (76.5%) underwent early nerve exploration with internal fixation. Intraoperatively, all patients had continuity of radial nerve except one patient with segmental loss. At the final follow-up, 16 patients (94.1%) with radial nerve palsy had made a complete recovery. The mean time to complete recovery was 6.7 months.
CONCLUSION
Primary radial nerve palsy after humerus shaft fracture was more common in young age, AO type B, distal 1/3 fractures. Early surgical exploration can be recommended to confirm the condition of the radial nerve if the fracture should be fixed. -
Citations
Citations to this article as recorded by- Treatment of Radial Nerve Palsy Associated with Humeral Shaft Fracture
Soo-Hong Han, Jin-Woo Cho, Han-Seung Ryu
Archives of Hand and Microsurgery.2020; 25(1): 60. CrossRef
- Treatment of Radial Nerve Palsy Associated with Humeral Shaft Fracture
- 1,273 View
- 21 Download
- 1 Crossref

- Ankle Fracture Associated with Tibia Shaft Fractures
- Ji Wan Kim, Hong Joon Choi, Dong Hyun Lee, Young Chang Kim
- J Korean Fract Soc 2014;27(2):136-143. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.136
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the incidence of ankle injury in ipsilateral tibial shaft fractures and to assess the risk factors for ankle injury associated with tibial shaft fractures.
MATERIALS AND METHODS
Sixty patients with tibial shaft fractures were enrolled in this retrospective study. The incidence and characteristics of ankle injury were evaluated, and fracture classification, fracture site, and fracture pattern of the tibial shaft fractures were analyzed for assessment of the risk factors for ankle injury combined with tibial shaft fractures.
RESULTS
Ankle injury occurred in 20 cases (33%). There were four cases of lateral malleolar fracture, four cases of posterior malleolar fracture, two cases of distal tibiofibular ligament avulsion fracture, and 10 cases of complex injury. Fourteen cases (70%) of 20 cases of ankle injury were diagnosed from x-ray films, and the other six cases were recognized in ankle computed tomography (CT). Ankle injury occurred in 45.1% of distal tibial shaft fractures and found in 41.4% of A type, but there was no statistical significance. Ankle injury was observed in 54% of cases of spiral pattern of tibial shaft fracture and the incidence was statistically higher than 19% of cases of non-spiral pattern tibial shaft fracture.
CONCLUSION
Ankle injury was observed in 33% of tibial shaft fractures; however, only 70% could be diagnosed by x-ray. Ankle injury occurred frequently in cases of spiral pattern of tibial shaft fracture, and evaluation of ankle injury with CT is recommended in these cases. -
Citations
Citations to this article as recorded by- Usefulness of Computed Tomography on Distal Tibia Intra-Articular Fracture Associated with Spiral Tibia Shaft Fracture
Seong-Eun Byun, Sang-June Lee, Uk Kim, Young Rak Choi, Soo-Hong Han, Byong-Guk Kim
Journal of the Korean Fracture Society.2016; 29(2): 114. CrossRef
- Usefulness of Computed Tomography on Distal Tibia Intra-Articular Fracture Associated with Spiral Tibia Shaft Fracture
- 817 View
- 7 Download
- 1 Crossref

- Treatment of Humeral Shaft Fracture with Retrograde Intramedullary Nail
- Ki Bum Choi, Soo Hwan Kang, Yoon Min Lee, Seok Whan Song, Youn Jun Kim
- J Korean Fract Soc 2013;26(4):299-304. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.299
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to report the outcome of treatment of humeral shaft fracture with retrograde intramedullary nail of advanced insertion opening.
MATERIALS AND METHODS
From April 2005 and August 2012, 22 patients with a humeral shaft fracture were treated by a single surgeon using the technique of retrograde intramedullary nail at Department of Orthopedic Surgery, Yeouido St. Mary's Hospital (Seoul, Korea). To avoid causing fractures at the insertion site, the entry point was more distally located than conventionally, and was extended proximally to include the proximal marginal cortex of the olecranon fossa. The outcome was evaluated clinically and radiologically.
RESULTS
The mean period of achievement of bony was 5.8 months (4-11 months). Additional fixations were needed in one patient with intraoperative lateral condylar fracture and 2 patients with postoperative nonunion. There were no limitations of movement or pain in the shoulder joint, and 8 cases had a 6.5degrees flexion contracture on average.
CONCLUSION
This retrograde intramedullary fixation technique using a distal entry portal near the olecranon fossa is particularly useful in humeral shaft fractures without a neurovascular injury. The risk of an intraoperative fracture (supracondylar fracture or fracture around the entry portal) can be decreased using this treatment. We recommend this technique because of the safety and the satisfactory outcome. -
Citations
Citations to this article as recorded by- HEALING PATTERN OF INTERLOCKED INTRAMEDULLARY NAILED HUMERAL SHAFT FRACTURE
Myung-Sang Moon, Dong-Hyeon Kim, Min-Geun Yoon, Sang-Yup Lee
Journal of Musculoskeletal Research.2016; 19(04): 1650018. CrossRef
- HEALING PATTERN OF INTERLOCKED INTRAMEDULLARY NAILED HUMERAL SHAFT FRACTURE
- 796 View
- 2 Download
- 1 Crossref

- Minimally Invasive Plate Osteosynthesis for Femoral Mid-Diaphyseal Fractures
- Hyoung Keun Oh, Suk Kyoo Choo, Jong In Kim, Sung Jong Woo
- J Korean Fract Soc 2013;26(2):140-146. Published online April 30, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.2.140
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the surgical outcomes of patients with femoral mid-diaphyseal fractures treated with minimally invasive plate osteosynthesis (MIPO), which were difficult to intramedullary nailing.
MATERIALS AND METHODS
We evaluated 11 patients with femoral mid-diaphyseal fractures who were treated with MIPO. There were 7 males and 4 females and the mean age was 47 years (20-85 years). According to AO/OTA classification, there were 1 type of A1, 5 types of A3, 1 of B2 and 4 of B3. The reason of plate fixation instead of intramedullary nailing is as follows: femoral vessel and severe soft tissue injuries-2 cases, polytrauma patients with chest injury-6 cases, and narrow medullary canal diameter-3 cases. Six out of 11 cases were treated with initial external fixation as a damage control orthopedics.
RESULTS
The mean union time of 6 cases was 3.7 months (3-5 months). There were 5 cases (45%) of nonunion, which should be treated with autogenous bone graft. All cases of nonunion resulted from severe soft tissue damage and polytrauma, which needed initial external fixation. There was no case of malalignment and implant-related complication.
CONCLUSION
In cases of difficult intramedullary nailing for the femoral mid-diaphyseal fractures, MIPO could be an alternative surgical option, but concurrent soft tissue injuries and multiple trauma may increase the risk of nonunion in spite of biological fixation.
- 334 View
- 2 Download

- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- Youn Soo Hwang, Kwang Yeol Kim, Hyung Chun Kim, Su Han Ahn, Dong Eun Lee
- J Korean Fract Soc 2013;26(1):14-20. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.14
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the effectiveness of optimal treatment of proximal humeral fractures and humeral shaft fractures in elderly patients with osteoporosis using the Polarus nail.
MATERIALS AND METHODS
Twenty-three patients with proximal humeral and humeral shaft fractures in elderly osteoporosis patients were treated using the Polarus intramedullary nail. Nine patients had proximal humeral fracture, 10 had humeral shaft fracture and 4 had the proximal humeral frac-ture extended diaphyseally. Radiological outcomes included the bone-union and the degree of re-sidual deformity. The residual deformities of the proximal humerus were assessed by the neck-shaft angle and the shaft angulation. Clinical outcome was assessed with the American Shoulder and Elbow Surgeons (ASES) score.
RESULTS
All cases had bony union and the mean union period was 16.5 weeks. The average neck/shaft alignment at the time of bone union was 135degrees and varus deformities of neck-shaft angle was not seen in all patients. Varus shaft angulation was seen in 5 patients. The mean ASES score after surgery was 86.7 points.
CONCLUSION
The Polarus intramedullary nail is effective for the treatment of proximal humeral and humeral shaft fractures in elderly patients with osteoporosis because it not only enables early postoperative mobilization, but also obtains bone-union without avascular necrosis and nonunion. -
Citations
Citations to this article as recorded by- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
Shankar Ramaprasad Kurpad
Indian Journal of Orthopaedics.2025; 59(8): 1053. CrossRef
- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
- 714 View
- 3 Download
- 1 Crossref

- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
- J Korean Fract Soc 2012;25(4):305-309. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.305
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Our study aimed to investigate the clinical and radiological results of humerus proximal or distal shaft fractures treated with minimally invasive plate osteosynthesis (MIPO) using a 3.5/5.0 metaphyseal locking plate.
MATERIALS AND METHODS
We reviewed the clinical and radiographic records of 17 patients with humeral proximal or distal shaft fractures who had undergone 3.5/5.0 metaphyseal locking plate osteosynthesis with a minimally invasive technique. We evaluated the results with respect to the anatomical reduction and union of the humerus shaft fracture through radiologic studies. We also evaluated the clinical results using the motion of shoulder and elbow functional outcome, American Shoulder and Elbow Surgeons (ASES) score, Mayo elbow performance score (MEPS), and postoperative complications.
RESULTS
Complete union was achieved in all cases. The mean union time was 14.2 weeks. According to the functional outcome rated by the ASES score and MEPS, 15 cases were considered excellent and 2 cases were good. There were no cases of surgically-related complications like metal failure, loss of anatomical reduction, or postoperative nerve injuries.
CONCLUSION
Using a 5.0 metaphyseal locking plate for humerus shaft fracture has the limitation that difficulties can arise in achieving sufficient screw fixation for small bony fragments. The 3.5/5.0 metaphyseal locking plate used in MIPO for humerus 1/3 proximal or distal shaft fractures was concluded to give good clinical and radiologic results. -
Citations
Citations to this article as recorded by- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
Journal of the Korean Fracture Society.2013; 26(1): 14. CrossRef
- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- 784 View
- 2 Download
- 1 Crossref

- Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
- Kyoung Hwan Koh, Min Soo Shon, Seung Won Lee, Jong Ho Kim, Jae Chul Yoo
- J Korean Fract Soc 2012;25(4):300-304. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.300
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the treatment results of anatomical reduction of all fracture fragments and internal fixation using an inter-fragmentary screw and plate in displaced mid-shaft clavicle fracture with comminution.
MATERIALS AND METHODS
Between June 2005 and August 2011, 13 consecutive displaced clavicle fractures with comminution (Edinburgh classification IIB2) treated by anatomic reduction and internal fixation using inter-fragmentary screw and plate were retrospectively evaluated. There were 11 male and 2 female patients with a mean age of 37.4 years (15~55 years). The right clavicle was injured in 4 patients and the dominant arm was involved in 46%. The mean duration from trauma to surgery was 7.0 days. The cause of injury was a traffic accident in three, a fall in two, and sports activity or direct injury in eight patients. All of the fracture pieces were anatomically reduced and fixed with inter-fragmentary screws. An additional plate was applied to maintain and reinforce the reduction of the fracture. Radiographic assessments for the numbers of fragments and the amount of shortening and displacement were performed. To verify the fracture healing and determine the time from fracture surgery to union and complications, all of the radiographs taken after surgery were evaluated.
RESULTS
The number of fragments was 2 in 7 cases, 3 in 5 cases, and 6 in one case. The mean shortening of the clavicle was 1.1 cm (0.3~2.1 cm) and mean displacement between the main fragments was 2.6 cm (1.3~4.5 cm). The mean duration of follow-up was 16.5 months (8~26 months). Radiographic union was achieved in all patients with a mean time to union of 10.8 weeks (8~14 weeks). There were no complications including metal failure, nonunion, or infection.
CONCLUSION
Anatomical reduction of all the fracture fragments and fixation using inter-fragmentary screws in addition to the usual plate fixation showed good fracture healing in displaced clavicle fracture with comminution. -
Citations
Citations to this article as recorded by- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
Woo Jin shin, Young Woo Chung, Seon Do Kim, Ki-Yong An
Clinics in Shoulder and Elbow.2020; 23(4): 205. CrossRef - Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
Journal of the Korean Fracture Society.2016; 29(3): 185. CrossRef
- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
- 843 View
- 3 Download
- 2 Crossref

Case Reports
- Delayed Brachial Artery Occlusion after Humeral Shaft Open Fracture: A Case Report
- Chul Hyun Cho, Ki Cheor Bae, Kyung Jae Lee, Si Wook Lee
- J Korean Fract Soc 2012;25(2):146-149. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.146
-
 Abstract
Abstract
 PDF
PDF - Although vascular injury after humeral fracture is very rare, it is a complication that has serious sequelae. It has been associated with proximal humeral fracture or shoulder dislocation in adults and humeral supracondylar fracture in children. However, delayed brachial artery occlusion after humeral shaft fracture has never been reported worldwide. Nevertheless, delayed brachial artery occlusion after humerus shaft fracture has the potential to cause serious complications in the short term as well as long term; therefore, it is essential to provide accurate diagnosis and prompt treatment. We report a case of delayed brachial artery occlusion after humeral shaft open fracture that was successfully treated with early diagnosis as well as effective treatment.
-
Citations
Citations to this article as recorded by- Delayed presentation of brachial artery injury following fracture shaft humerus; whether amputate or salvage: A series of two cases
Bhanu Sharma, Sibashish Metia, Kavish Kapoor, Pankaj Poswal
Journal of Orthopedics, Traumatology and Rehabilitation.2018; 10(2): 137. CrossRef
- Delayed presentation of brachial artery injury following fracture shaft humerus; whether amputate or salvage: A series of two cases
- 868 View
- 2 Download
- 1 Crossref

- Repeated Metal Breakage in a Femoral Shaft Fracture with Lateral Bowing: A Case Report
- Dong Soo Kim, Yong Min Kim, Eui Sung Choi, Hyun Chul Shon, Kyoung Jin Park, Byung Ki Cho, Ji Kang Park, Hyun Cheol Lee, Kyung Ho Hong
- J Korean Fract Soc 2012;25(2):136-141. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.136
-
 Abstract
Abstract
 PDF
PDF - Fractures of the femoral shaft with marked bowing face some obstacles in fixation of the fracture such as difficulty in insertion of the intramedullary nail (IM nail) or exact contouring plate. Locking compression plates (LCP) are an option to manage this problem. However, we experienced consecutive breakage of LCP twice and IM nail once in an 80-year-old female. Finally, union of the fracture was achieved after fixation of the IM nail and additional plate together. Fractures of the femur shaft with marked bowing are thought to have different biomechanical properties; therefore, we present this case with a review of the literature.
-
Citations
Citations to this article as recorded by- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
Milan Mitkovic, Sasa Milenkovic, Ivan Micic, Predrag Stojiljkovic, Igor Kostic, Milorad Mitkovic
Vojnosanitetski pregled.2022; 79(2): 177. CrossRef - Pre-operative planning for fracture fixation using locking plates: device configuration and other considerations
Alisdair R. MacLeod, Pankaj Pankaj
Injury.2018; 49: S12. CrossRef - Letter: Repeated Metal Breakage in a Femoral Shaft Fracture with Lateral Bowing - A Case Report -
Hae Seok Koh
Journal of the Korean Fracture Society.2012; 25(3): 240. CrossRef
- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
- 609 View
- 3 Download
- 3 Crossref

Original Articles
- Comparison of Plate Versus Threaded K-wire for Fixation of Midshaft Clavicular Fractures
- Young Jin Ko, Chul Hyun Park, Oog Jin Shon, Jae Sung Seo
- J Korean Fract Soc 2012;25(2):123-128. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.123
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare clinical outcomes of the plate and threaded K-wire for fixation of midshaft clavicular fractures.
MATERIALS AND METHODS
From 2005 Jan to 2009 May, medical records of 18 patients who underwent open reduction and internal fixation with plate (group 1) and 13 others who underwent intramedullary fixation with threaded K-wire (group 2) were reviewed. The mean follow up periods were 21.9 and 18.9months. The Functional results were evaluated with The Disabilities of the Arm, Shoulder and Hand (DASH) score and Constant shoulder score. The statistical evaluation was assessed with Paired T-test, Chi-square test.
RESULTS
The DASH score were 11.5+/-2.7 in group 1 and 12.4+/-4.3 in group 2. The constant shoulder score were 92.0+/-3.1 in group 1 and 87.1+/-2.8 in group 2. Length of surgical wound (cm) were 10.6+/-3.4 in group 1 and 4.8+/-1.5 in group 2. Postoperative pain and range of motion change were superior in group 1.
CONCLUSION
There was no significant difference between the two groups in functional and radiological results. But, there were patient's complaints about length of surgical wound in group 1 and hardware irritation in group 2. -
Citations
Citations to this article as recorded by- A Comparison between Minimally Invasive Percutaneous Plate Osteosynthesis and Plate Fixation in the Treatment of Clavicle Midshaft Fracture
Seong-Ho Yoo, Suk-Woong Kang, Bu-Hwan Kim, Moo-Ho Song, Yeong-Joon Kim, Gyu-Taek Park, Chang-Hun Kwack
Journal of the Korean Orthopaedic Association.2017; 52(1): 1. CrossRef - Plate fixation versus intramedullary fixation for midshaft clavicle fractures: Meta-analysis of complications and functional outcomes
Hao Xiao, Hengbo Gao, Tuokang Zheng, Jianhui Zhao, Yingping Tian
Journal of International Medical Research.2016; 44(2): 201. CrossRef - Meta-analysis of plate fixation versus intramedullary fixation for the treatment of mid-shaft clavicle fractures
Bing Zhang, Yanbin Zhu, Fei Zhang, Wei Chen, Ye Tian, Yingze Zhang
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.2015;[Epub] CrossRef
- A Comparison between Minimally Invasive Percutaneous Plate Osteosynthesis and Plate Fixation in the Treatment of Clavicle Midshaft Fracture
- 676 View
- 2 Download
- 3 Crossref

- The Fate of Butterfly Fragments in Extremity Shaft Comminuted Fractures Treated with Closed Interlocking Intramedullary Nailing
- Ki Chan An, Yoon Jun Kim, Jang Suk Choi, Seung Suk Seo, Hi Chul Gwak, Dae Won Jung, Dong Woo Jeong
- J Korean Fract Soc 2012;25(1):46-51. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.46
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
For conservative treatment of shaft fractures, the butterfly fragments that were somewhat larger in the closed intra-medullary (IM) nailing. The results of treatment were monitored using radiography separately for the weight-bearing femur and non-weight-bearing humerus.
MATERIALS AND METHODS
27 from Group I and 31 from Group II. In the two groups, the displacement and angulation changes in the fragments, and the degree of improvement of these two factors, were compared using follow-up radiography.
RESULTS
The mean angulation of fragments in Groups I and II were 9.2degrees and 9.6degrees, and the mean degree of displacement of the fragments in Groups I and II were 16.7 mm and 21.2 mm, respectively. Follow-up radiography showed that the above factors improved in both groups. The degree of displacement was significantly lower in the normal cases than in the complicated cases (p=0.001).
CONCLUSION
Displacement and angulation gradually improved in both groups. It was found that the degree of displacement after the initial reduction is more important than the influence of anatomical position or weight bearing. This indicates that care should be taken when inserting IM nails to prevent displacement or angulation. -
Citations
Citations to this article as recorded by- Risk Factors for Failure of Nonsurgical Management of Ulnar Shaft Fractures
Carew C. Giberson-Chen, Cassandra M. Chruscielski, Dafang Zhang, Philip E. Blazar, Brandon Earp
The Journal of Hand Surgery.2025; 50(4): 497.e1. CrossRef - The impact of the third fragment features on the healing of femoral shaft fractures managed with intramedullary nailing: a radiological study
Giovanni Vicenti, Massimiliano Carrozzo, Vincenzo Caiaffa, Antonella Abate, Giuseppe Solarino, Davide Bizzoca, Roberto Maddalena, Giulia Colasuonno, Vittorio Nappi, Francesco Rifino, Biagio Moretti
International Orthopaedics.2019; 43(1): 193. CrossRef - Reply to “Letter to the Editor on: The impact of the third fragment features on the healing of femoral shaft fractures managed with intramedullary nailing: a radiological study”
Giovanni Vicenti, Massimiliano Carrozzo, Davide Bizzoca, Biagio Moretti
International Orthopaedics.2019; 43(6): 1545. CrossRef - Letter to the Editor on “The impact of the third fragment features on the healing of femoral shaft fractures managed with intramedullary nailing: a radiological study”
Shih-Jie Lin, Kevin Liaw, Tsan-Wen Huang
International Orthopaedics.2019; 43(6): 1543. CrossRef - The impact of the third fragment features on the healing of femoral shaft fractures managed with intramedullary nailing: a radiological study
Giovanni Vicenti, Massimiliano Carrozzo, Vincenzo Caiaffa, Antonella Abate, Giuseppe Solarino, Davide Bizzoca, Roberto Maddalena, Giulia Colasuonno, Vittorio Nappi, Francesco Rifino, Biagio Moretti
International Orthopaedics.2018;[Epub] CrossRef - Comparison of the Result of the Intramedullary Nail Fixation and Plate Fixation in Humeral Shaft Fracture with Butterfly Fragments
Duk-Hwan Kho, Hyeung-June Kim, Byoung-Min Kim, Hyun-Ryong Hwang
The Korean Journal of Sports Medicine.2016; 34(2): 120. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef
- Risk Factors for Failure of Nonsurgical Management of Ulnar Shaft Fractures
- 949 View
- 9 Download
- 7 Crossref

- Surgical Techniques for Percutaneous Reduction by Towel Clips and Percutaneous Intramedullary Fixation with Steinmann Pins for Clavicle Shaft Fractures
- Ki Do Hong, Jae Chun Sim, Sung Sik Ha, Tae Ho Kim, Jong Hyun Kim, Jong Seong Lee
- J Korean Fract Soc 2012;25(1):31-37. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.31
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the clinical results of surgical treatment of clavicle shaft fracture by percutaneous reduction with towel clips and percutaneous intramedullary pin fixation.
MATERIALS AND METHODS
This study reviewed the results of 80 cases of clavicle shaft fracture treated by percutaneous reduction with towel clips and percutaneous intramedullary pin fixation with Steinmann pins from January 2002 to August 2010, after follow-up for 12 months or more. We evaluated the clinical results, such as union time and complications.
RESULTS
Bone union was evident in all cases and the mean time for bone union to appear on radiological findings was 10.3 weeks. Using Kang's criteria, 78 of the 80 patients (97.5%) showed good results and there were no severe complications.
CONCLUSION
Percutaneous reduction with towel clips and the percutaneous intramedullary pin fixation method showed good results for treating clavicle shaft fracture. -
Citations
Citations to this article as recorded by- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
Woo Jin shin, Young Woo Chung, Seon Do Kim, Ki-Yong An
Clinics in Shoulder and Elbow.2020; 23(4): 205. CrossRef - A Comparison between Minimally Invasive Percutaneous Plate Osteosynthesis and Plate Fixation in the Treatment of Clavicle Midshaft Fracture
Seong-Ho Yoo, Suk-Woong Kang, Bu-Hwan Kim, Moo-Ho Song, Yeong-Joon Kim, Gyu-Taek Park, Chang-Hun Kwack
Journal of the Korean Orthopaedic Association.2017; 52(1): 1. CrossRef
- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
- 724 View
- 2 Download
- 2 Crossref

- Minimally Invasive Anterior Plating of Humeral Shaft Fractures
- Hyun Joo Lee, Chang Wug Oh, Do Hyung Kim, Kyung Hyun Park
- J Korean Fract Soc 2011;24(4):341-346. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.341
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We evaluated the efficacy and results of minimally invasive anterior plating for humeral shaft fracture.
MATERIALS AND METHODS
Twenty-two cases of humeral shaft fracture were reviewed, including 8 cases of type A, 8 of type B and 6 of type C (AO/OTA classification). There were three open fractures. The fracture was fixed with MIPO (minimally invasive plate osteosynthesis) technique under C-arm guide. A locking compression plate was located in anterior aspect of the humerus with at least three screws fixed in each fragment. Radiologic and functional results were evaluated.
RESULTS
In 20 of 22 cases, bony union was achieved with the mean period of 17.5 weeks, including 2 cases of delayed union. There were 2 cases of nonunion, which needed the further operative procedure. Except one case of distal 1/3 fracture, all cases showed satisfactory elbow and shoulder function with the mean Mayo elbow score of 17.4 and mean UCLA shoulder score of 97.3. In complication, there was one case of radial nerve palsy due to improper traction, but it was completely improved after 3 months. Otherwise, there was no complication including infection.
CONCLUSION
Anterior MIPO for humeral shaft fracture may be another option of operative methods with high union and low complication rate. -
Citations
Citations to this article as recorded by- Minimal Invasive Plate Osteosynthesis versus Conventional Open Plating in Simple Humeral Shaft Fracture (AO Type A, B1, B2)
Boseon Kim, GwangChul Lee, Hyunwoong Jang
Journal of the Korean Fracture Society.2017; 30(3): 124. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef - Operative Treatment of Humerus Shaft Fracture: Conventional Open Plating or Minimally Invasive Plate Osteosynthesis
Hyun-Joo Lee, Chang-Wug Oh
Journal of the Korean Fracture Society.2012; 25(2): 155. CrossRef
- Minimal Invasive Plate Osteosynthesis versus Conventional Open Plating in Simple Humeral Shaft Fracture (AO Type A, B1, B2)
- 772 View
- 8 Download
- 3 Crossref

- Analysis of Risk Factors for Nonunion after Intramedullary Nailing of Femoral Shaft Fracture in Adult
- Yong Woon Shin, Yerl Bo Sung, Jeong Yoon Choi, Minkyu Kim
- J Korean Fract Soc 2011;24(4):313-320. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.313
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the union time and nonunion rate after intramedullary nailing of femoral shaft fracture in adult, we would like to analysis the operation techniques, comminution, contact surface and displacement.
MATERIALS AND METHODS
We reviewed retrospectively 53 patients undergoing femoral intramedullary nailing at least 2 years postoperatively and analysised the union time and nonunion rate by operation techniques, comminution, contact surface and displacement. Patients were operated by either antegrade or retrograde intramedullary nailing.
RESULTS
There were no differences in nonunion rate, the duration of bony union between antegrade and retrograde intramedullary nail groups. Significant differences were found in the duration of bony union between the Winquist and Hansen type I, II and the type III, IV (p<0.05). There were significant differences in the duration of bony union among simple, comminuted, and segmental fracture groups (p<0.05).
CONCLUSION
The union time is affected by not operation techniques and fracture displacement, but Winquist-Hansen classification and number of fracture fragments in intramedullary nailing of adult femoral shaft fracture. -
Citations
Citations to this article as recorded by- Extra-capsular proximal femoral fractures: a cohort comparison of union and complication rates after ballistic versus blunt trauma
Jordan Cook Serotte, Kevin Chen, Julia Nascimben, Jason Strelzow
European Journal of Orthopaedic Surgery & Traumatology.2025;[Epub] CrossRef - Factors Affecting Time to Bony Union of Femoral Subtrochanteric Fractures Treated with Intramedullary Devices
Jung-Yoon Choi, Yerl-Bo Sung, Jin-Hee Yoo, Sung-Jae Chung
Hip & Pelvis.2014; 26(2): 107. CrossRef - Augmentative Locking Plate Fixation for the Treatment of Femoral Nonunion after Intramedullary Nailing
Ki-Chul Park, Chul-Woong Kim, Kyu-Tae Hwang, Ye-Soo Park
Journal of the Korean Fracture Society.2013; 26(4): 268. CrossRef
- Extra-capsular proximal femoral fractures: a cohort comparison of union and complication rates after ballistic versus blunt trauma
- 893 View
- 7 Download
- 3 Crossref

- Clinical Outcome of Surgical Treatment for Fracture of the Femoral Shaft with Ipsilateral Fracture of the Proximal Femur
- Hee Gon Park, Jae Sung Yoo
- J Korean Fract Soc 2011;24(4):307-312. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.307
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze diagnostic process and clinical data in cases of fracture of the femoral shaft with fracture of the proximal femur.
MATERIALS AND METHODS
We reviewed 24 cases of patient who undergone surgery for fracture of the femoral shaft with ipsilateral fracture of the proximal femur and more than 1 year of examination of follow up was available. Age, sex.location and classification of the fracture, the time of diagnosis and operation, the method of operation, the associated injuries, the time of bony union and complication were investigated, postoperative function was evaluated on Friedman and Wyman criteria.
RESULTS
Bony union showed significant difference in the displacement and comminution of fracture, postoperative function revealed significant difference according to the associated injuries. The 6 cases (25%) out of 24 cases are failed early diagnosis, 4 cases out of 6 cases was detected during operation and 2cases was found after surgery. 21 cases out of 24 cases of femoral shaft fractures showed union, 23 cases out of 24 cases of femoral neck fractures showed union. There were eleven good, eleven fair, and two poor functional result according to Friedman and Wyman criteria.
CONCLUSION
Precious clinical and radiologic examination is needed not to miss the diagnosis of proximal femur fractures in ipsilateral femoral shaft fractures with proximal femur fractures. Anatomical reduction and rigid fixation of proximal femur are important to reduce avascular necrosis of femoral head and nonunion of proximal femoral fractures.
- 383 View
- 2 Download

- Intramedullary Nailing for Complex Fractures of the Proximal and Midshaft of the Humerus
- Chul Hyun Cho, Gu Hee Jung, Kyo Wook Kim
- J Korean Fract Soc 2011;24(3):237-242. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.237
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results of antegrade interlocking intramedullary nailing for complex fractures of the proximal and midshaft of the humerus.
MATERIALS AND METHODS
We retrospectively analyzed the clinical and radiologic results in 11 cases, which were treated by antegrade interlocking intramedullary nail. We assessed clinical outcomes according to ASES scoring system and radiological result.
RESULTS
All cases had bony union and the mean union period was 14.7 weeks. Postoperative complications were 1 loss of fixation, 2 proximal protrusion of nail and 2 temporary shoulder pain. A case with loss of fixation was treated open reduction and refixation and had union at 14 weeks postoperatively. The mean ASES score was 85.9 and the clinical outcomes were 4 excellent, 5 good, 1 fair and 1 poor.
CONCLUSION
Intramedullary nailing for complex fractures of the proximal and midshaft of the humerus can offer a reliable treatment option.
- 390 View
- 0 Download

- Does Interfragmentary Cerclage Wire Fixation in Clavicle Shaft Fracture Interfere the Fracture Healing?
- Jae Kwang Yum, Yong Woon Shin, Hee Sung Lee, Jae Gu Park
- J Korean Fract Soc 2011;24(2):138-143. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.138
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
A technique of cerclage wire fixation in comminuted fracture of the clavicle shaft is thought to interfere the fracture healing, so authors studied radiographically and clinically about the cases of cerclage wiring of the fracture fragments with the plate and screws fixation in the comminuted fracture of the shaft of the clavicle.
MATERIALS AND METHODS
According to following inclusion criteria, total 18 patients (male: 15, female: 3) were investigated; Patients who visited hospital due to clavicle shaft comminuted fracture from February 2005 to April 2009, who underwent surgery utilizing more than 2 cerclage wire fixation for the fragments when open reduction and plate fixation were operated and who could be follow-up over one year. The duration for fracture union, functional outcome and complications were investigated retrospectively.
RESULTS
Radiological bone union was accomplished in average 13.3 weeks (12~16 weeks) and there was no complication such as nonunion, delayed union or infection. Range of motion of ipsilateral shoulder joint was recovered in all patients except one at the final follow-up.
CONCLUSION
The clinical and radiographical results of the plate and screws fixation with cerclage wiring of the fragments in comminuted clavicle shaft fracture showed that the cerclage wiring does not interfere the fracture healing, so authors think that this method is a good alternative operation if it is performed carefully to minimize soft tissue dissection. -
Citations
Citations to this article as recorded by- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
Kyung-Tae Kim, Chung-Shik Shin, Young-Chul Park, Dong-hyun Kim, Min-Woo Kim
Journal of the Korean Orthopaedic Association.2021; 56(3): 245. CrossRef - Supplementary Technique for Unstable Clavicle Shaft Fractures: Interfragmentary Wiring and Temporary Axial K-Wire Pinning
Jinmyoung Dan, Byung-Kook Kim, Ho-Jae Lee, Tae-Ho Kim, Young-Gun Kim
Clinics in Orthopedic Surgery.2018; 10(2): 142. CrossRef - Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
Journal of the Korean Fracture Society.2016; 29(3): 185. CrossRef - TO EVALUATE THE SURGICAL OUTCOME OF NON-UNION CLAVICLE USING PLATE AND SLIVERS OF AUTOLOGOUS ILIAC CREST CORTICOCANCELLOUS BONE GRAFT
Mohammed Tauheed, Shashi Kumar Yalagach, Vivek Purushothaman, Anwar Shareef Kunnath K
Journal of Evidence Based Medicine and Healthcare.2016; 3(25): 1121. CrossRef - Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
Kyoung Hwan Koh, Min Soo Shon, Seung Won Lee, Jong Ho Kim, Jae Chul Yoo
Journal of the Korean Fracture Society.2012; 25(4): 300. CrossRef
- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
- 862 View
- 0 Download
- 5 Crossref

- Anterior Knee Pain after Intramedullary Nailing for Tibial Shaft Fractures
- Suk Kyu Choo, Hyoung Keun Oh, Hyun Woo Choi, Jae Gwang Song
- J Korean Fract Soc 2011;24(1):28-32. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.28
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the possible causes and incidence of the chronic anterior knee pain follow after closed intramedullary nailing for the tibial shaft fractures, in a retrospective aspect.
MATERIALS AND METHODS
52 patients who treated with intramedullary nailing for the tibial shaft fractures from January 2001 to October 2008 were reviewed. We analyzed the relationship between knee pain and the variables (sex, age, types of fracture, protrusion extent of intramedullary nailing on proximal tibia). The aspects of pain, its onset and relieving time, and how much it influences on daily living were analyzed retrospectively. For categorical variables, group variences were estimated using Chi-square test.
RESULTS
34 patients of 52 (65%) complaint of anterior knee pain followed after intramedullary nailing, and there were no statistical differences between pain and sex/age (p>0.05). Incidence of anterior knee pain becomes higher as the severity of fracture increases, but there was no statistical difference between pain and intramedullary nailing protrusion. Pain severity was mostly not influencing on daily living, and it mostly responded to conservative treatment.
CONCLUSION
The incidence of anterior knee pain followed after intramedullary nailing was 65%, and its severity was mostly not influencing on daily living. There were no significant differences between pain and sex, age, protrusion extent of intramedullary nailing on proximal tibia, but as the severity of frature increases, the incidence of anterior knee pain became higher. -
Citations
Citations to this article as recorded by- Pain in Anterior Knee after Locked Nailing of Diaphyseal Tibia Fractures
V. V. Pisarev
Traumatology and Orthopedics of Russia.2020; 26(1): 85. CrossRef - Stress fractures of the tibia
Jung Min Park, Ki Sun Sung
Arthroscopy and Orthopedic Sports Medicine.2015; 2(2): 95. CrossRef - Tension Band Plating for a Stress Fracture of the Anterior Tibial Cortex in a Basketball Player - A Case Report -
Chul Hyun Park, Woo Chun Lee
Journal of the Korean Fracture Society.2012; 25(4): 323. CrossRef
- Pain in Anterior Knee after Locked Nailing of Diaphyseal Tibia Fractures
- 1,404 View
- 3 Download
- 3 Crossref

Case Report
- Dislocation of the Shoulder with Ipsilateral Humeral Shaft Fracture: A Case Report
- Chul Hyun Cho, Kwang Yeung Jeong
- J Korean Fract Soc 2010;23(4):382-385. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.382
-
 Abstract
Abstract
 PDF
PDF - Dislocation of the shoulder with ipsilateral humeral shaft fracture is very rare, but serious injury that requires emergent care. There have been approximately 20 cases reported in the English literature, but it has never been reported in Korea. We report a case of dislocation of right shoulder with ipsilateral humeral shaft fracture which was successfully treated by closed reduction of the shoulder under general anesthesia and internal fixation with antegrade interlocking intramedullary nailing for the humeral shaft fracture.
-
Citations
Citations to this article as recorded by- Anterior Shoulder Dislocation With an Ipsilateral Humeral Shaft Fracture: A Case Report
Abdulmalik B Albaker , Ahmad Abdullah A Alsaleh, Mishari Malik Alshammari, Hatim Abdullah Akkasi, Hazzaa Abdullah Hazza Alharbi, Norah Ibrahim S Alqurmulah
Cureus.2023;[Epub] CrossRef
- Anterior Shoulder Dislocation With an Ipsilateral Humeral Shaft Fracture: A Case Report
- 704 View
- 1 Download
- 1 Crossref

Original Article
- Percutaneous Retrograde Intramedullary Pin Fixation for Isolated Metacarpal Shaft Fracture of the Little Finger
- Soo Hong Han, Hyung Ku Yoon, Dong Eun Shin, Seung Chul Han, Young Woong Kim
- J Korean Fract Soc 2010;23(4):367-372. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.367
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the anatomic and functional outcome of retrograde intramedullary single wire fixation for metacarpal shaft fractures of the little finger.
MATERIALS AND METHODS
hirty one consecutive patients with closed metacarpal shaft fractures of the little finger who have been treated with retrograde intramedullary single wire fixation were evaluated. Fracture union and angulation were analyzed radiologically, and clinical evaluations were performed including range of motion, DASH score and complications.
RESULTS
Fracture union was achieved in all cases and callus formation was obvious at postoperative 41 days. Average angulation of fracture site was 3degrees in the coronal plane and 1.2degrees in the sagittal plane at the last follow up and no measurable metacarpal shortening was observed. Mean TAM was 253degrees and DASH score was 2.6. There were two cases of pin migration as intermediate complications.
CONCLUSION
Closed reduction with subsequent percutaneous retrograde K-wire fixation produced good radiological and functional results. We recommend this minimally invasive technique which provides adequate fixation of displaced little finger metacarpal shaft fractures with good functional results and low morbidity. -
Citations
Citations to this article as recorded by- The Treatment Outcomes of the Metacarpal Shaft and Neck Comminuted Fractures Using Modified Percutaneous Retrograde Intramedullary Kirschner Wire Fixation
Seok Woo Hong, Young Ho Lee, Min Bom Kim, Goo Hyun Baek
Archives of Hand and Microsurgery.2018; 23(3): 175. CrossRef
- The Treatment Outcomes of the Metacarpal Shaft and Neck Comminuted Fractures Using Modified Percutaneous Retrograde Intramedullary Kirschner Wire Fixation
- 920 View
- 4 Download
- 1 Crossref

Case Report
- Bursting Fracture of the Proximal Femur during Insertion of Unreamed Femoral Nail for Femur Shaft Fracture: A Case Report
- Ji Wan Kim, Seong Eun Byun, Won Hyuk Oh, Jung Jae Kim
- J Korean Fract Soc 2010;23(2):227-231. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.227
-
 Abstract
Abstract
 PDF
PDF - When treating femur shaft fracture in adults, undreamed nail can be an option in order to avoid systemic complications. To appropriately insert unreamed intramedullary nail, an accurate entry point and sufficient reaming of the entry portal is essential. The intramedullary canal of the proximal femur must be reamed over than the diameter of the proximal end of the nail. If the proximal reaming is not sufficient, complications such as bursting fracture of proximal femur can occur. We present two cases of bursting fracture of proximal femur following insertion of undreamed intramedullary nail as well as a literature review.
-
Citations
Citations to this article as recorded by- Risk Factors Associated with Intraoperative Iatrogenic Fracture in Patients Undergoing Intramedullary Nailing for Atypical Femoral Fractures with Marked Anterior and Lateral Bowing
Yong Bum Joo, Yoo Sun Jeon, Woo Yong Lee, Hyung Jin Chung
Medicina.2023; 59(4): 735. CrossRef - Results of Intramedullary Nailing of Femoral Shaft Fracture - Trochanteric Entry Portal (Sirus Nail) versus Piriformis Entry Portal (M/DN Nail) -
Sang Ho Ha, Woong-Hee Kim, Gwang Chul Lee
Journal of the Korean Fracture Society.2014; 27(1): 50. CrossRef - Iatrogenic Femur Proximal Shaft Fracture during Nailing Using Lateral Entry Portal on Femur Shaft Fracture
Hong Moon Sohn, Gwang Chul Lee, Chae Won Lim
Journal of the Korean Orthopaedic Association.2014; 49(4): 272. CrossRef
- Risk Factors Associated with Intraoperative Iatrogenic Fracture in Patients Undergoing Intramedullary Nailing for Atypical Femoral Fractures with Marked Anterior and Lateral Bowing
- 875 View
- 2 Download
- 3 Crossref

Original Articles
- Treatment of Femoral Shaft Fracture with Interlocking Humeral Nail in Older Children and Adolescent
- Kun Bo Park, Hoon Park, Hyun Woo Kim, Hui Wan Park, Jae Young Roh
- J Korean Fract Soc 2010;23(2):206-212. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.206
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results of interlocking humeral nail for femur shaft fractures through the greater trochanter in older children and adolescent.
MATERIALS AND METHODS
Eleven femoral shaft fractures in ten patients were selected. They were consisted of 9 boys and 1 girl. Two patients had osteogenesis imperfecta and one patient had a simple bone cyst as an underlying disease. 7 cases were right side and 4 cases were left side. The mean age at the time of operation was 12 years and 7 months (8 years 11 months~15 years 7 months). The mean follow-up period was 21 months and interlocking humeral nail was inserted at the greater trochanter in all patients.
RESULTS
All patients had a complete bony union without any complication such as infection, nonunion, leg length discrepancy and metal failure. Avascular necrosis of femoral head and coxa valga were not developed in all patients.
CONCLUSION
Intramedullary nailing through the greater trochanter using interlocking humeral nail is effective and safe treatment for the femoral shaft fracture in older children and adolescents.
- 609 View
- 2 Download

- The Comparison of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing in the Treatment of the Proximal and Distal Tibia Fracture
- Joon Soon Kang, Seung Rim Park, Sang Rim Kim, Yong Geun Park, Jae Ho Jung, Sung Wook Choi
- J Korean Fract Soc 2010;23(2):172-179. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.172
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the efficacy of the surgical treatment through the comparison of Minimally Invasive Plate Osteosynthesis (MIPO) and Intramedullary (IM) nailing in the treatment of the tibial shaft fractures expended to metaphysis retrospectively.
MATERIALS AND METHODS
Patients with proximal or distal third fracture of tibial shaft from May 2003 to Aug. 2006 were divided into two groups depending on the surgical method. Group A consisted of 30 patients treated with IM nailing, Group B was 29 patients treated with MIPO. The clinical outcomes were evaluated retrospectively from the time for bone union and callus formation confirmed by X-ray, functional score of knee or ankle joint, and complications including nonunion, malalignment and infection.
RESULTS
Bone union was seen radiologically at a mean of 17.4 weeks in group A, and 17.0 weeks in group B. In postoperative complications, group A showed two nonunion, two delayed-union, six malalignment, and two wound infection while group B showed only one delayed-union and one wound infection.
CONCLUSION
There were no significant differences in the time for bony union and functional score between IM nailing and MIPO. Conventional IM nailing with only interlocking technique showed higher incidence of malalignment and deformity than MIPO for the treatment of the proximal or distal third fracture of the tibial shaft. -
Citations
Citations to this article as recorded by- Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
Jung Min Lee, Eun-Jung Lee
Journal of Korean Medicine Rehabilitation.2020; 30(3): 141. CrossRef
- Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
- 956 View
- 4 Download
- 1 Crossref

Case Report
- Repetitive Insufficiency Fractures of the Femoral Shaft: A Case Report
- Ji Hwan Kim, Young Ho Cho, Young Soo Byun, Jung Hoon Shin, Chung Yeol Lee, Tae Gyun Kim
- J Korean Fract Soc 2010;23(1):109-112. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.109
-
 Abstract
Abstract
 PDF
PDF - Stress fractures occur when the loads applied to a bone exceed the mechanical resistance and fall into two groups. Fatigue fractures, in which abnormal mechanical stress is applied to a normal bone, and insufficiency fractures, in which fracture occurs when stress of normal activity is applied to a bone that has decreased elastic resistance. Femoral shaft insufficiency fractures are reported rarely in patients with postmenopausal osteoporosis. We report a case of repetitive insufficiency fractures of the femoral shaft in 70 year-old female with marked osteoporosis.
- 486 View
- 2 Download

Original Articles
- Limited Open Reduction and Intramedullary Nailing of Proximal Femoral Shaft Fracture
- Sang Ho Ha, Jun Young Lee, Sang Hong Lee, Sung Hwan Jo, Jae Cheul Yu
- J Korean Fract Soc 2009;22(4):225-231. Published online October 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.4.225
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the result of treatment of proximal femoral shaft fracture with limited open reduction and intramedullary nailing. MATERIALS AND METHODS: Fifteen patients who had limited open reduction and intramedullary nailing due to proximal femoral shaft fracture for follow-up for more than 12 months were selected between March 2001 and December 2005. The clinical and radiologic results were analyzed. Winquist-Hansen classification and OTA/AO classification were used. RESULTS: Thirteen cases achieved bone union and 2 cases showed delayed union. The mean bone union period was 21.3 weeks (14~32). There was no postoperative infection. Nonunion was observed in 2 cases of which bone union was acquired with the exchange of intramedullary nail and bone graft in one case and with the additional plate fixation and bone graft in the other case. CONCLUSION: Treating proximal femoral shaft fracture with limited open reduction and intramedullary nailing seems to be a technique to manage proximal femoral shaft fracture that has combined fracture or ipsilateral femoral fracture or is unable to acquire acceptable reduction with closed reduction.
- 767 View
- 2 Download

- Interlocking Intramedullary Nailing of Forearm Shaft Fractures in Adults
- Sanglim Lee, Hee Sung Lee, Yerl Bo Sung, Jae Kwang Yum
- J Korean Fract Soc 2009;22(1):30-38. Published online January 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.1.30
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of interlocking intramedullary nailing for operative treatment of forearm shaft fractures in adults.
MATERIALS AND METHODS
Thirteen forearm shaft fractures in 12 patients were fixated with 13 Acumed forearm intramedullary rods (ulna: 8, radius: 5). The average age was 36.7 years and mean follow-up period was 15.2 months. The union time was measured when there was no tenderness over the fracture site and the bridging callus was evident in at least two sides of the cortex. The range of motion of the joint and the rotation of the forearm was measured and the functional results were evaluated with Grace and Eversmann's rating system.
RESULTS
Radiologic union was observed at 11.8 weeks postoperatively in 11 cases out of 13. No limitation of motion was observed. Nine had excellent or good functional results. In one Galeazzi fracture, radial shaft became displaced after nailing and should be re-stabilized with plate. Proximal interlocking screws were improperly inserted in one ulnar nail. Implants were removed in 7 cases. Removal guide screw was broken while removing the intramedullary nail in one case of ulnar shaft fracture.
CONCLUSION
Interlocking intramedullay nailing might be a treatment option for the middle 1/3 shaft fractures of the adult forearm bone with favorable results. -
Citations
Citations to this article as recorded by- Comparison of minimally invasive plate osteosynthesis (MIPO) and open reduction and internal fixation (ORIF) for the treatment of radial shaft fractures: a retrospective study
Hyun-Tak Kang, Yang-Hoon Jo, Hong-Je Kang
BMC Musculoskeletal Disorders.2025;[Epub] CrossRef - Distal blocking screw augmentation in ulnar intramedullary nail fixation of adult forearm diaphyseal fractures
Yong Woo Kim, Sang Ki Lee, Young Sun An
Journal of Orthopaedic Surgery.2024;[Epub] CrossRef - Comparison of Bending Strength among Plate, Steinmann Pin, and Headless Compression Screw Fixations for Proximal Ulnar Shaft Fracture in Sawbones
Jinyoung Han, Jin Rok Oh, Jaewoong Um
Archives of Hand and Microsurgery.2020; 25(4): 267. CrossRef
- Comparison of minimally invasive plate osteosynthesis (MIPO) and open reduction and internal fixation (ORIF) for the treatment of radial shaft fractures: a retrospective study
- 857 View
- 4 Download
- 3 Crossref

- Contributing Factors of Radial Nerve Palsy Associated with Humeral Shaft Fracture
- Tae Soo Park, Joon Hwan Lee, Tai Seung Kim, Kwang Hyun Lee, Ki Chul Park
- J Korean Fract Soc 2008;21(4):292-296. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze related factors of radial nerve palsy in patients with humeral shaft fractures.
MATERIALS AND METHODS
We reviewed 107 paients with humeral shaft fracture between January 2000 and June 2007. Thirteen patients had radial nerve palsy after trauma and 9 patients after the operation. We analyzed contributing factors of radial nerve palsy associated with humeral shaft fracture including the cause of trauma, location and pattern of fracture, surgical approach and tourniquet application in cases of plate fixation, the exploration for the nerve and the time for operation.
RESULTS
The difference in the incidences of radial nerve palsy after trauma and operation was not significant according to the location and pattern of fracture. The tendency of higher rate of radial nerve palsy after trauma in oblique or comminuted fractures, and after operation in spiral fractures was observed. The operation using intramedullary nailing and radial nerve exploration significantly reduced the incidence of radial nerve palsy after operation (p=0.01 and p=0.02). Posterior approach in open reduction and plate fixation showed a tendency of lower incidence of radial nerve palsy after operation (p=0.78). In logistic regression analysis, radial nerve exploration was the only significant factor that reduced the possibility of radial nerve palsy after operation (17.27: odds ratio, p=0.02).
CONCLUSION
In humeral shaft fractures, we should take into consideration whether intramedullary nailing is possible or not. In cases of anterior or anterolateral approach of open reduction and plate fixation, radial nerve should be carefully inspected. In most cases, we recommend radial nerve exploration in order to minimize the possibility of radial nerve palsy after operation. -
Citations
Citations to this article as recorded by- Treatment of Radial Nerve Palsy Associated with Humeral Shaft Fracture
Soo-Hong Han, Jin-Woo Cho, Han-Seung Ryu
Archives of Hand and Microsurgery.2020; 25(1): 60. CrossRef - Associated Factors of Radial Nerve Palsy Combined with Humerus Shaft Fracture
Si-Wuk Lee, Chul-Hyun Cho, Ki-Choer Bae
Journal of the Korean Fracture Society.2014; 27(3): 185. CrossRef - Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
Journal of the Korean Fracture Society.2013; 26(1): 14. CrossRef
- Treatment of Radial Nerve Palsy Associated with Humeral Shaft Fracture
- 700 View
- 0 Download
- 3 Crossref

Case Report
- Medial Transposition of Radial Nerve in Distal Humerus Shaft Fracture: A Report of Six Cases
- Sang Uk Lee, Weon Yoo Kim, Soo Hwan Kang, Yong Soo Park, Seung Koo Rhee
- J Korean Fract Soc 2008;21(3):240-243. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.240
-
 Abstract
Abstract
 PDF
PDF - Sometimes serious tension occurs in the radial nerve when doing internal fixation for distal humerus shaft fracture or neurorrhaphy for radial nerve injury. Medial transposition of radial nerve on fracture site can avoid direct radial nerve injury by fracture fragment, radial nerve tension by plating for distal humerus shaft fracture, and also safe from neural tension during neurorrhaphy of damaged radial nerve. We reported here total 6 cases of backward transposition of radial nerve including 2 cases of radial nerve injury associated with humerus fracture and 4 cases of comminuted fracture of humerus shaft.
-
Citations
Citations to this article as recorded by- Transhumeral Anterior Radial Nerve Transposition to Simplify Anticipated Future Humeral Reconstruction
David A. Muzykewicz, Reid A. Abrams
The Journal of Hand Surgery.2017; 42(7): 578.e1. CrossRef - Transfracture medial transposition of the radial nerve associated with plate fixation of the humerus
Ali Hassan Chamseddine, Amer Abdallah, Hadi Zein, Assad Taha
International Orthopaedics.2017; 41(7): 1463. CrossRef - Trans-fracture transposition of the radial nerve during the open approach of humeral shaft fractures
Ali H. Chamseddine, Hadi K. Zein, Abdullah A. Alasiry, Nader A. Mansour, Ali M. Bazzal
European Journal of Orthopaedic Surgery & Traumatology.2013; 23(6): 725. CrossRef - Humerus Shaft Fractures in Leisure Sport 'Flyfish Riding' - 4 Cases Report -
Bong Gun Lee, Ki Chul Park, Youn Ho Choi, Woo Sung Jung, Kyu Tae Hwang
Journal of the Korean Fracture Society.2012; 25(4): 327. CrossRef
- Transhumeral Anterior Radial Nerve Transposition to Simplify Anticipated Future Humeral Reconstruction
- 739 View
- 1 Download
- 4 Crossref

Original Articles
- The Treatment of IM Nailing of Femoral Shaft Fracture: Piriformis Fossa versus Trochanteric Entry Portal
- Hyun Kook Youn, Oog Jin Shon, Dong Sung Han
- J Korean Fract Soc 2008;21(3):200-206. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.200
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the results of IM nailing of femur shaft fractures using trochanteric and piriformis fossa entry portal.
MATERIALS AND METHODS
37 patients were treated with IM nail using Trochanteric (Trochanter group: TG, n=17) and piriformis fossa entry portal (piriformis group: PG, n=20) and were followed from February 2004 to 2007. The outcomes were assessed based on the clinical and radiographic findings.
RESULTS
The functional result, ROM and union time were similar in both groups. The alignment was similar in both groups but PG showed variable alignment in proximal 1/3. Incision was larger in PG (PG=8.7 cm, TG=5.8 cm, p<0.05) and there was a difference between overweight and normal weight group. Operative time was 95 minutes in PG, 87 minutes in TG (p>0.05), there was statistically significant difference in overweight groups (PG=125 minutes, TG=90 minutes, p<0.05). Blood loss was 313 cc in PG, 268 cc in TG and less in TG in overweight patients (p<0.05). There was 5.7degrees of varus angulation in PG, 2 nonunion cases in both groups.
CONCLUSION
The femoral nail specially designed for trochanteric insertion resulted in high union rates, low complication rates similar to conventional nail and the trochanteric nail can be the alternative choice especially in proximal femur fracture and overweight patients.
- 478 View
- 0 Download

- Treatment of Forearm Shaft Fracture with Modified Interlocking Intramedullary Nail
- Kwang Yul Kim, Moon Sup Lim, Shin Kwon Choi, Hyeong Jo Yoon
- J Korean Fract Soc 2008;21(2):157-164. Published online April 30, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.2.157
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the result of forearm shaft fracture treated by modified interlocking intramedullary nail (Acumed, Hillsbrough, IN, USA).
MATERIALS AND METHODS
15 patients with fracture of radius, ulna, radio-ulna shaft treated by modified interlocking intramedullary nail from December 2003 to February 2007 were analyzed. Modified interlocking intramedullary nail has paddle blade tip and fluted rod, so the distal screw fixation was not needed but had relatively firm fixation. It has advantages including short operation time, small operation scar. The average follow up period was 8.3 months (range, 5~15 months). We analyzed the results by average union time and the functional results according to Anderson's criteria.
RESULTS
The mean duration of union was 9.8 weeks in radius and 11.4 weeks in ulna. The average range of motion of forearm was 74.6 degree in supination and 72 degree in pronation.. Functional results assessed by Anderson were rated excellet in 12 cases, satisfactory in 3 cases. We found no complications such as delayed union, non-union, neurovascular injury and infection.
CONCLUSION
Modified interlocking intramedullary nail (Acumed, Hillsbrough, IN, USA) is a viable therapeutic alternative in the management of forearm shaft fracture. -
Citations
Citations to this article as recorded by- Interlocking Intramedullary Nailing of Forearm Shaft Fractures in Adults
Sanglim Lee, Hee-Sung Lee, Yerl-Bo Sung, Jae-Kwang Yum
Journal of the Korean Fracture Society.2009; 22(1): 30. CrossRef
- Interlocking Intramedullary Nailing of Forearm Shaft Fractures in Adults
- 632 View
- 0 Download
- 1 Crossref

- The Comparison of LC-DCP versus LCP Fixation in the Plate Augmentation for the Nonunion of Femur Shaft Fractures after Intramedullary Nail Fixation
- Se Dong Kim, Oog Jin Sohn, Byung Hoon Kwack
- J Korean Fract Soc 2008;21(2):117-123. Published online April 30, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.2.117
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the efficacy of the surgical treatment through the comparison of LC-DCP (Limited Contact-Dynamic Compression Plate) versus LCP (Locking Compression Plate) fixation in the plate augmentation for the nonunion of femur shaft fractures after intramedullary nail fixation.
MATERIALS AND METHODS
Twenty-four patients with the nonunion of femur shaft fractures after intramedullary nail fixation who underwent plate augmentation were evaluated from Mar. 2001 to Sept. 2005. The group with LC-DCP augmentation was done bicortical screw fixation and the group with LCP was done monocortical fixation.
RESULTS
There was one case of nail breakage in LC-DCP group, but sound bony union were achieved uneventfully in all the cases of both group. LCP fixation was slightly superior to LC-DCP fixation in view of the bony union time, operating time, postoperative Hb down, amount of postoperative transfusion, but there was no statistical difference (p>0.05). CONCLUSION: We got the satisfactory results after monocortical LCP augmentation as well as bicortical LC-DCP fixation and have concluded that monocortical LCP fixation was an effective treatment option for nonunion of femur shaft fracture occurred after Intrmedullary nail fixation. -
Citations
Citations to this article as recorded by- Delayed Union and Nonunion: Current Concepts, Prevention, and Correction: A Review
Kristin M. Bowers, David E. Anderson
Bioengineering.2024; 11(6): 525. CrossRef - RETRACTED ARTICLE: An experimental study on stress-shielding effects of locked compression plates in fixing intact dog femur
Xinwen Zhao, Wensen Jing, Zhe Yun, Xun Tong, Zhao Li, Jiajia Yu, Yaohui Zhang, Yabin Zhang, Zhixue Wang, Yanhua Wen, Heping Cai, Jun Wang, Baoan Ma, Haien Zhao
Journal of Orthopaedic Surgery and Research.2021;[Epub] CrossRef - The Treatment of IM Nailing of Femoral Shaft Fracture: Piriformis Fossa versus Trochanteric Entry Portal
Hyun Kook Youn, Oog Jin Shon, Dong Sung Han
Journal of the Korean Fracture Society.2008; 21(3): 200. CrossRef
- Delayed Union and Nonunion: Current Concepts, Prevention, and Correction: A Review
- 987 View
- 11 Download
- 3 Crossref

Case Report
- Intramedullary Plate Fixation for the Comminuted Fracture of the Femoral Shaft: A Case Report
- Ju O Kim, Mun Su Jeong, Bong Ju Park
- J Korean Fract Soc 2007;20(4):345-348. Published online October 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.4.345
-
 Abstract
Abstract
 PDF
PDF - A case of the comminuted fracture of the femoral shaft with osteoporosis is presented. The patient lacked sufficient bony stability and cortical bone-contact which allows union by conventional reconstruction method. Therefore, the authors performed a technique utilizing an intramedullary plate in combination with the standard lateral plate in order to obtain bony stabilization, early range of motion of the knee, and partial weight bearing ambulation and the technique is introduced.
- 757 View
- 10 Download

Original Articles
- Comparison of LC-DCP versus LCP for Internal Fixation of Humeral Shaft Fractures in Elderly Patient
- Chang Yong Hur, Won Yong Shon, Jun Gyu Moon, Sang Hwan Han, Jae Young Hong, Sung Kang Chun
- J Korean Fract Soc 2007;20(3):246-251. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.246
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare outcomes of humeral shaft fractures fixed with locking compression plate and those fixed with dynamic compression plate in elderly patients.
MATERIALS AND METHODS
Nineteen consecutive elderly patients with a fracture of the humeral diaphysis were evaluated retrospectively. Ten patients had been fixed with LC-DCP, and nine had been fixed with LCP. Radiological and clinical results were compared and comparison of implants was done.
RESULTS
Loosening of the plate occurred in one case each from the LCP group and the LC-DCP group. The rest of the patients achieved union uneventfully without any complications. Union rate, clinical score and hardware were not significantly different between the two groups. One patient who developed loosening in the LC DCP underwent reoperation whereas one patient with loosening in the LCP was successfully managed conservatively.
CONCLUSION
Principle of fracture fixation was more important than plate selection in humeral shaft fracture of elderly patient. -
Citations
Citations to this article as recorded by- Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates
Ashutosh Kumar Singh, Nidhi Narsaria, R. R. Seth, S. Garg
Journal of Orthopaedics and Traumatology.2014; 15(2): 117. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef
- Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates
- 1,005 View
- 4 Download
- 2 Crossref

- Comparison of Results in Two Operative Treatments for Clavicle Shaft Fractures in Adult: Comparison of Results between Open Reduction and Internal Fixation with the Plate and Percutaneous Reduction by Towel Clip and Intramedullary Fixation with Steinmann Pin
- Sung Sik Ha, Jae Chun Sim, Ki Do Hong, Jae Young Kim, Jung Ho Kang, Kwang Hee Park
- J Korean Fract Soc 2007;20(3):233-238. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.233
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results between open reduction and internal fixation with the plate and percutaneous reduction by towel clip and intramedullary fixation with Steinmann pin for clavicle shaft fractures in adult.
MATERIALS AND METHODS
We have studied the results in 33 cases with the plate, 35 cases with the Steinmann pin among total 68 cases of clavicle shaft fracture. The patients were followed up over a period of at least 12 months. The final postoperative outcome was analyzed with the clinical outcomes using Kang's criteria, radiological union time and operation time.
RESULTS
The clinical outcome that was good or excellent according to the Kang's criteria showed a distribution of 88% in the group using the plate with 29 cases out of total 33 cases, 91% in the group using the Steinmann pin with 32 cases out of total 35 cases. The mean radiological union time was 8.9 weeks in the group using the plate, 9.1 weeks in the group using Steinmann pin. The mean operation time was 72 minutes in the group using the plate, whereas was 18 minutes in the group using Steinmann pin.
CONCLUSION
In the treatment of adult clavicle shaft fracture, two groups did not show a significant statistical difference in clinical and radiological outcomes. However, the operation time and postoperative functional recovery was significantly shorter and faster in the group using Steinmann pin. Additionally economic and cosmetic aspect was more satisfactory in the group using Steinmann pin. -
Citations
Citations to this article as recorded by- Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
Kyoung Hwan Koh, Min Soo Shon, Seung Won Lee, Jong Ho Kim, Jae Chul Yoo
Journal of the Korean Fracture Society.2012; 25(4): 300. CrossRef - Does Interfragmentary Cerclage Wire Fixation in Clavicle Shaft Fracture Interfere the Fracture Healing?
Jae-Kwang Yum, Yong-Woon Shin, Hee-Sung Lee, Jae-Gu Park
Journal of the Korean Fracture Society.2011; 24(2): 138. CrossRef
- Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
- 760 View
- 1 Download
- 2 Crossref

- Result of Interlocking Intramedullary Nailing for Humeral Shaft Fracture Evaluation of Post-operative Shoulder Function
- Seung Rim Park, Tong Joo Lee, Ryuh Sub Kim, Kyoung Ho Moon, Dong Seok You
- J Korean Fract Soc 2007;20(2):166-171. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.166
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the post-operative functional reduction of the shoulder joint and the impacting factors to post-operative shoulder joint function in interlocking IM nailing treatment of humeral shaft fracture.
MATERIALS AND METHODS
From April 1999 to August 2004, 35 patients (35 cases) whom admitted to hospital for humeral shaft fracture and treated using interlocking intramedullary nail were followed up for more than 1 year. 1 year post-operative shoulder joint function were evaluated using American Shoulder Elbow Surgery Scale (ASES). Pre-operative shoulder joint pain, radiologically degenerative change and extent of nail protrusion were evaluated, and each factor was correlated with function of the shoulder joint.
RESULTS
33 cases out of 35 cases showed union and average union period was 12 weeks. Complications consisted of 2 cases of nonunion, 1 case of infection, 1 case of loosening of distal fixing screw, 1 case of radial nerve palsy and 1 case of axillary nerve palsy. Shoulder joint function 3 months after operation : mean ASES score 78.2, 12 months after operation : mean ASES score 89.6. Pre-operative shoulder joint pain and nail protrusion showed to be statistically related to shoulder joint function.
CONCLUSION
If the operation leaves no protrusion of intramedullary nail, it can be concluded to be relatively safe and effective. -
Citations
Citations to this article as recorded by- Comparison of the Result of the Intramedullary Nail Fixation and Plate Fixation in Humeral Shaft Fracture with Butterfly Fragments
Duk-Hwan Kho, Hyeung-June Kim, Byoung-Min Kim, Hyun-Ryong Hwang
The Korean Journal of Sports Medicine.2016; 34(2): 120. CrossRef - Plain Radiograph Analysis of the Distal Humerus Posterior Bowing That May Affect Interlocking Intramedullary Nailing for Humerus Shaft Fracture
Jaekwang Yum, Kyunghwan Boo, Minkyu Sung, Jiseok Jang
Journal of the Korean Orthopaedic Association.2015; 50(1): 31. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef - Surgical Treatment of Pathologic Humeral Fracture
Ho Jung Kang, Byoung Yoon Hwang, Jae Jeong Lee, Kyu Ho Shin, Soo Bong Hahn, Sung Jae Kim
Journal of the Korean Fracture Society.2010; 23(2): 187. CrossRef
- Comparison of the Result of the Intramedullary Nail Fixation and Plate Fixation in Humeral Shaft Fracture with Butterfly Fragments
- 702 View
- 0 Download
- 4 Crossref

- Cause and Treatment of the Nonunion of Femoral Shaft Fracture after Interlocking Intramedullary Nailing
- Sung Soo Kim, Sung Keun Sohn, Chul Hong Kim, Myung Jin Lee, Lih Wang
- J Korean Fract Soc 2007;20(2):141-148. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.141
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the causes and the clinical results of treatment for the nonunion of femur shaft fractures that occurred after interlocking intramedullary nail fixation.
MATERIALS AND METHODS
We reviewed 19 cases of aseptic nonunion of femur shaft fracture in 174 patients after interlocking IM nailing from March 1999 to February 2004 and followed up for more than one year. First we investigated the factors causing nonunion. For operative options, two methods about exchange nailing and exchange nailing with bone graft were performed. Finally clinical results were analyzed with bone union rate by treatment methods and compared with the nonunion factors statistically.
RESULTS
According to the causes and types of nonunion, we performed larger IM nail change in 10 cases and IM nail change with bone graft in 9 cases. Bone union was achieved in all cases. Average bone union period were 18.5 weeks in exchange group and 16.1 weeks in exchange with bone graft group. There are significant difference between treatment methods statistically (p<0.05). Compared with the nonunion factors, initial open fracture and smoking groups showed late union rate statistically.
CONCLUSION
Based on our analysis, IM nail change is a useful method for nonunion after initial IM nailing in femoral shaft fracture, and additional bone graft that according to the radiologic pattern and stability, especially the fracture gap is also a useful option for nonunion treatment. -
Citations
Citations to this article as recorded by- Results of Exchange Nailing in Hypertrophic Nonunion of Femoral Shaft Fracture Treated with Nailing
Suenghwan Jo, Gwang Chul Lee, Sang Hong Lee, Jun Young Lee, Dong Hwi Kim, Sung Hae Park, Young Min Cho
Journal of the Korean Fracture Society.2019; 32(2): 83. CrossRef - Analysis of Risk Factors for Nonunion after Intramedullary Nailing of Femoral Shaft Fracture in Adult
Yong-Woon Shin, Yerl-Bo Sung, Jeong Yoon Choi, Minkyu Kim
Journal of the Korean Fracture Society.2011; 24(4): 313. CrossRef - Limited Open Reduction and Intramedullary Nailing of Proximal Femoral Shaft Fracture
Sang Ho Ha, Jun Young Lee, Sang Hong Lee, Sung Hwan Jo, Jae Cheul Yu
Journal of the Korean Fracture Society.2009; 22(4): 225. CrossRef
- Results of Exchange Nailing in Hypertrophic Nonunion of Femoral Shaft Fracture Treated with Nailing
- 1,274 View
- 12 Download
- 3 Crossref

- Comparison of Operative Methods between Retrograde and Antegrade Nailing for Ipsilateral Femoral Shaft and Neck Fracture
- Chang Wug Oh, Jong Keon Oh, Woo Kie Min, Shin Yoon Kim, Seung Hoon Baek, Byung Chul Park, Hyung Soo Ahn, Tae Gong Kim
- J Korean Fract Soc 2007;20(2):135-140. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.135
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare retrospectively the antegrade and retrograde nailing in the management of ipsilateral femoral neck and shaft fractures.
MATERIALS AND METHODS
Thirty-two patients (thirty-three injuries) were included in this study. Mean age of patients was 38 years-old in the antegrade nailing group (16 injuries) and 44 years-old in the retrograde nailing group (17 injuries). We compared the union of fractures and complications between two groups, and investigated the influencing factors.
RESULTS
Femoral shaft fracture was united in 10 cases (63%) of antegrade group and 12 cases (71%) of retrograde group, at 28.2 and 27.3 weeks respectively. Nonunion was more prevalent in Winquist-Hansen III and IV (5 in antegrade nailing, 3 in retrograde nailing) than I and II. Femoral neck fracture was united with 1 case of nonunion in each group. Nonunion developed from Garden stage IV, but fractures of Garden stage I and II united regardless of methods.
CONCLUSION
In ipsilateral femoral neck and shaft fractures, the kinds of methods did not affect the results of shaft fractures. Minimally displaced neck fractures also were not influenced by kinds of methods, but retrograde nailing may have a benefit in fixing the displaced neck fractures -
Citations
Citations to this article as recorded by- Surgical management of bifocal femoral fractures: a systematic review and pooled analysis of treatment with a single implant versus double implants
J. D. Cnossen, Esther M. M. Van Lieshout, Michael H. J. Verhofstad
Archives of Orthopaedic and Trauma Surgery.2023; 143(10): 6229. CrossRef - Retrograde Intramedullary Nailing or the Treatment of Segmental Femoral Shaft Fracture Including Distal Part
Jong-Ho Yoon, Byung-Woo Ahn, Chong-Kwan Kim, Jin-Woo Jin, Ji-Hoon Lee, Hyun-Ku Cho, Joo-Hyun Lee
Journal of the Korean Fracture Society.2009; 22(3): 145. CrossRef - The Treatment of IM Nailing of Femoral Shaft Fracture: Piriformis Fossa versus Trochanteric Entry Portal
Hyun Kook Youn, Oog Jin Shon, Dong Sung Han
Journal of the Korean Fracture Society.2008; 21(3): 200. CrossRef
- Surgical management of bifocal femoral fractures: a systematic review and pooled analysis of treatment with a single implant versus double implants
- 737 View
- 3 Download
- 3 Crossref

- The Fractures of Humerus Shaft and Medial Epicondyle by Arm Wrestling
- Yeo Hun Yoon, Jong Kyung Ha, Kyung Eob Choi, Kwan Hee Lee, Sang Jin Shin
- J Korean Fract Soc 2006;19(4):437-442. Published online October 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.4.437
-
 Abstract
Abstract
- PURPOSE
To evaluate the mechanism of the humeral fractures induced by arm wrestling and the clinical results of its treatment.
MATERIALS AND METHOD
We reviewed 7 humeral fractures induced by arm wrestling; 3 humeral shaft fractures, 4 humeral medial epicondyle fractures. The mechanism of the fractures and the clinical results were assessed by history and radiographs.
RESULTS
Shaft fractures were produced by twist and axial compression force. Humeral medial epicondyle fractures were the avulsion fractures by excessive contraction of flexor muscles and developed in young age. We operated 6 of them and in all cases, we could obtain fracture healings without complication.
CONCLUSION
The humeral fractures induced by arm wrestling have the differences in the ages and mechanisms as to the locations of the fractures and if the proper treatment is performed, the clinical results are satisfactory. -
Citations
Citations to this article as recorded by- Distal humerus fractures caused during amateur arm wrestling-a case report and literature review
Ali A. Burhani, Shreyas B. L., Akash Bansal
International Journal of Research in Orthopaedics.2025; 11(5): 1288. CrossRef - Fractures of the humeral shaft caused by arm wrestling: a systematic review
Kiyohisa Ogawa, Atsushi Yoshida, Noboru Matsumura, Wataru Inokuchi
JSES Reviews, Reports, and Techniques.2022; 2(4): 505. CrossRef - Olecranon Fracture Sustained during Arm Wrestling in Middle-Aged Male
Chang-Yk Lee, Hyuk-Min Kwon, Han-Bit Kim
Journal of the Korean Orthopaedic Association.2022; 57(6): 520. CrossRef - Fracture-Separation of the Medial Humeral Epicondyle Caused by Arm Wrestling: A Systematic Review
Kiyohisa Ogawa, Atsushi Yoshida, Noboru Matsumura, Wataru Inokuchi
Orthopaedic Journal of Sports Medicine.2022;[Epub] CrossRef - Humerus Shaft Fractures Occurring in Fly Fishing Boat Riding: Injury Scene Analysis
Hongri Li, Wan Sun Choi, Bong-gun Lee, Jae-hoo Lee, Younguk Park, Doohyung Lee
The Korean Journal of Sports Medicine.2019; 37(4): 134. CrossRef - Humeral Shaft Fracture Sustained during Arm Wrestling in Young Males
Seung Rim Yi, Jieun Kwon, Ye Hyun Lee, Bo Kyu Yang, Young Joon Ahn, Se Hyuk Im, Joon Hee Cho, Sang Hoon Park
The Korean Journal of Sports Medicine.2017; 35(3): 149. CrossRef - Humerus Shaft Fractures in Leisure Sport 'Flyfish Riding' - 4 Cases Report -
Bong Gun Lee, Ki Chul Park, Youn Ho Choi, Woo Sung Jung, Kyu Tae Hwang
Journal of the Korean Fracture Society.2012; 25(4): 327. CrossRef
- Distal humerus fractures caused during amateur arm wrestling-a case report and literature review
- 681 View
- 0 Download
- 7 Crossref

- External Fixation of Pediatric Femur Fractures
- Yeung Jin Kim, Tae Kyun Kim, Hwan Deok Yang, Hyung Joon Kim, Jin Young Park, Sang Jin Eun
- J Korean Fract Soc 2006;19(3):369-373. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.369
-
 Abstract
Abstract
- PURPOSE
To evaluate unilateral external fixation when applied as the standard treatment of displaced femoral shaft fractures in children.
MATERIALS AND METHODS
From 2000 through 2004, we used a unilateral external fixator (Any-fix(R)) to treat 24 femoral shaft fractures. The average age of the patients was 8.3 years (range, 5.6 to 14.8). 16 fractures were isolated, and 8 were associated with polytrauma. There were 4 open fractures. Patients were followed clinically and radiologically until healing and at 1 year.
RESULTS
Average time of external fixation was 97 days (range, 57 to 130 days). All patients regained the normal range of motion of knee joint without significant residual leg length discrepancy or growth disturbance. There were no nonunion, or rotationary deformities. There were 26 pin tract infection (total pin number: 108) (24%), all of which were resolved with antibiotics. No patient developed osteomyelitis. There were two refractures after fixator removal. There was one case of reduction loss and one of valgus deformity.
CONCLUSION
The external fixation is a useful alternative for operative management of femoral shaft fractures because of minimal invasive operation, and early mobilization in prepuberty.
- 457 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


