Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(4); 2013 > Article
-
Original Article
- Treatment of Humeral Shaft Fracture with Retrograde Intramedullary Nail
- Ki-Bum Choi, M.D., Soo-Hwan Kang, M.D., Ph.D., Yoon-Min Lee, M.D., Seok-Whan Song, M.D., Ph.D., Youn-Jun Kim, M.D.
-
Journal of the Korean Fracture Society 2013;26(4):299-304.
DOI: https://doi.org/10.12671/jkfs.2013.26.4.299
Published online: October 18, 2013
Department of Orthopedic Surgery, The Catholic University of Korea Yeouido St. Mary's Hospital, Seoul, Korea.
*Department of Orthopedic Surgery, The Catholic University of Korea St. Paul's Hospital, Seoul, Korea.
- Address reprint requests to: Seok-Whan Song, M.D., Ph.D. Department of Orthopedic Surgery, The Catholic University of Korea Yeouido St. Mary's Hospital, 10 63-ro, Yeongdeungpo-gu, Seoul 150-713, Korea. Tel: 82-2-3779-1192, Fax: 82-2-783-0252, sw.song@catholic.ac.kr
• Received: December 27, 2012 • Revised: July 16, 2013 • Accepted: August 22, 2013
Copyright © 2013 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 794 Views
- 2 Download
- 1 Crossref
Abstract
-
Purpose
- The purpose of this study was to report the outcome of treatment of humeral shaft fracture with retrograde intramedullary nail of advanced insertion opening.
-
Materials and Methods
- From April 2005 and August 2012, 22 patients with a humeral shaft fracture were treated by a single surgeon using the technique of retrograde intramedullary nail at Department of Orthopedic Surgery, Yeouido St. Mary's Hospital (Seoul, Korea). To avoid causing fractures at the insertion site, the entry point was more distally located than conventionally, and was extended proximally to include the proximal marginal cortex of the olecranon fossa. The outcome was evaluated clinically and radiologically.
-
Results
- The mean period of achievement of bony was 5.8 months (4-11 months). Additional fixations were needed in one patient with intraoperative lateral condylar fracture and 2 patients with postoperative nonunion. There were no limitations of movement or pain in the shoulder joint, and 8 cases had a 6.5° flexion contracture on average.
-
Conclusion
- This retrograde intramedullary fixation technique using a distal entry portal near the olecranon fossa is particularly useful in humeral shaft fractures without a neurovascular injury. The risk of an intraoperative fracture (supracondylar fracture or fracture around the entry portal) can be decreased using this treatment. We recommend this technique because of the safety and the satisfactory outcome.
- 1. Barnes CE, Shuler TE. Complications associated with the Seidel nail. Orthop Rev, 1993;22:699-706.
- 2. Blum J, Janzing H, Gahr R, Langendorff HS, Rommens PM. Clinical performance of a new medullary humeral nail: antegrade versus retrograde insertion. J Orthop Trauma, 2001;15:342-349.
- 3. Brumback RJ. The rationales of interlocking nailing of the femur, tibia, and humerus. Clin Orthop Relat Res, 1996;(324):292-320.
- 4. Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma, 2008;65:94-102.
- 5. Crates J, Whittle AP. Antegrade interlocking nailing of acute humeral shaft fractures. Clin Orthop Relat Res, 1998;(350):40-50.
- 6. Flinkkilä T, Hyvönen P, Lakovaara M, Linden T, Ristiniemi J, Hämäläinen M. Intramedullary nailing of humeral shaft fractures. A retrospective study of 126 cases. Acta Orthop Scand, 1999;70:133-136.
- 7. Ingman AM, Waters DA. Locked intramedullary nailing of humeral shaft fractures. Implant design, surgical technique, and clinical results. J Bone Joint Surg Br, 1994;76:23-29.PDF
- 8. Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br, 1966;48:105-111.PDF
- 9. Lin J. Treatment of humeral shaft fractures with humeral locked nail and comparison with plate fixation. J Trauma, 1998;44:859-864.
- 10. Lin J, Hou SM. Locked nailing of severely comminuted or segmental humeral fractures. Clin Orthop Relat Res, 2003;(406):195-204.
- 11. McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br, 2000;82:336-339.
- 12. Scheerlinck T, Handelberg F. Functional outcome after intramedullary nailing of humeral shaft fractures: comparison between retrograde Marchetti-Vicenzi and unreamed 4 AO antegrade nailing. J Trauma, 2002;52:60-71.
- 13. Seidel H. Humeral locking nail: a preliminary report. Orthopedics, 1989;12:219-226.
- 14. Zagorski JB, Latta LL, Zych GA, Finnieston AR. Diaphyseal fractures of the humerus. Treatment with prefabricated braces. J Bone Joint Surg Am, 1988;70:607-610.
REFERENCES
Fig. 1
(A) The skin was incised curvilinearly from the midline of the distal humerus to the lateral condyle.
(B) After using the triceps splitting approach, (C) a cortical window was made at the superior margin of the olecranon fossa and was extended proximally about 3 cm.
(D) Nail and locking screws were inserted, without an iatrogenic supracondylar fracture occurring.
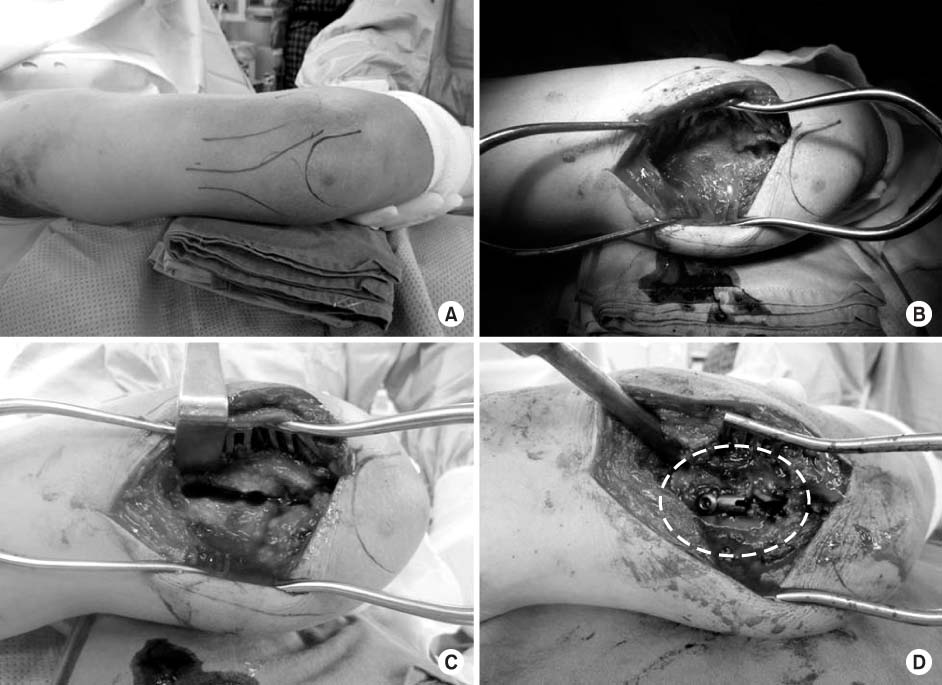
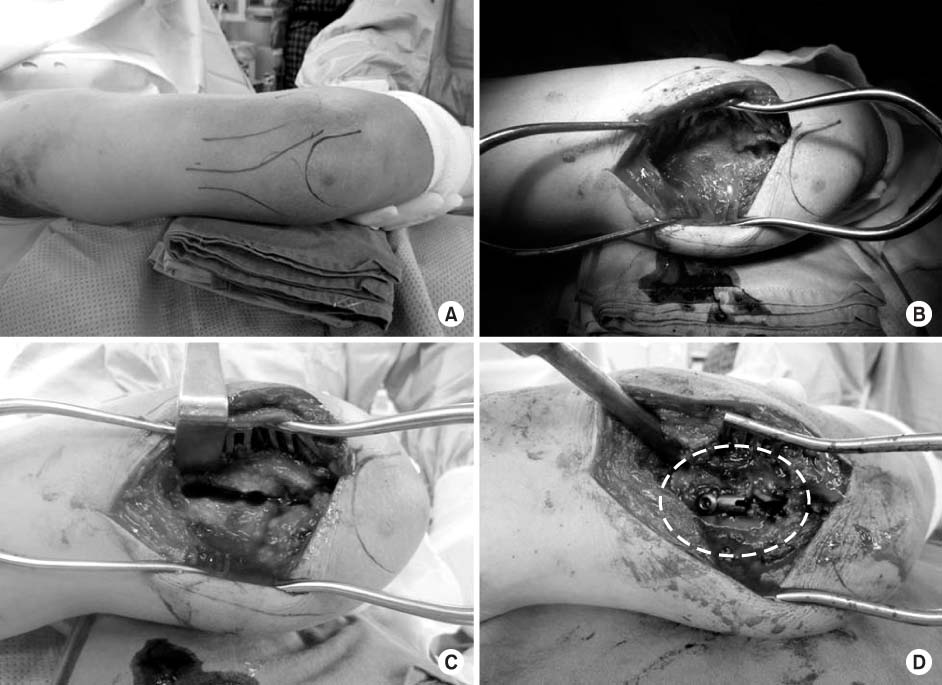
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- HEALING PATTERN OF INTERLOCKED INTRAMEDULLARY NAILED HUMERAL SHAFT FRACTURE
Myung-Sang Moon, Dong-Hyeon Kim, Min-Geun Yoon, Sang-Yup Lee
Journal of Musculoskeletal Research.2016; 19(04): 1650018. CrossRef
Treatment of Humeral Shaft Fracture with Retrograde Intramedullary Nail

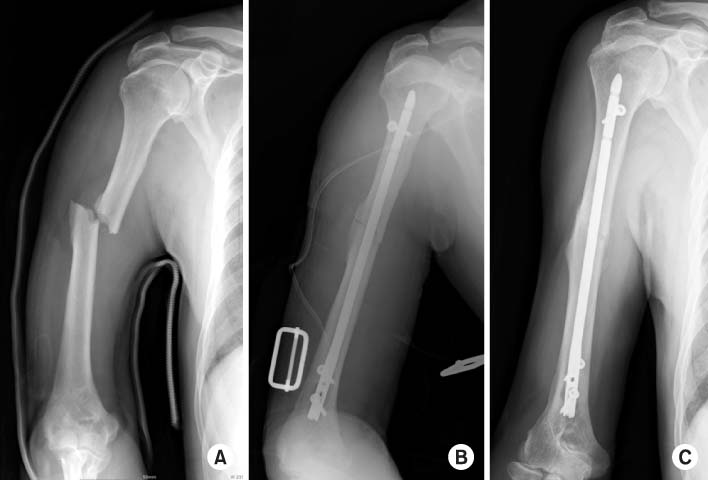
Fig. 1
(A) The skin was incised curvilinearly from the midline of the distal humerus to the lateral condyle.
(B) After using the triceps splitting approach, (C) a cortical window was made at the superior margin of the olecranon fossa and was extended proximally about 3 cm.
(D) Nail and locking screws were inserted, without an iatrogenic supracondylar fracture occurring.
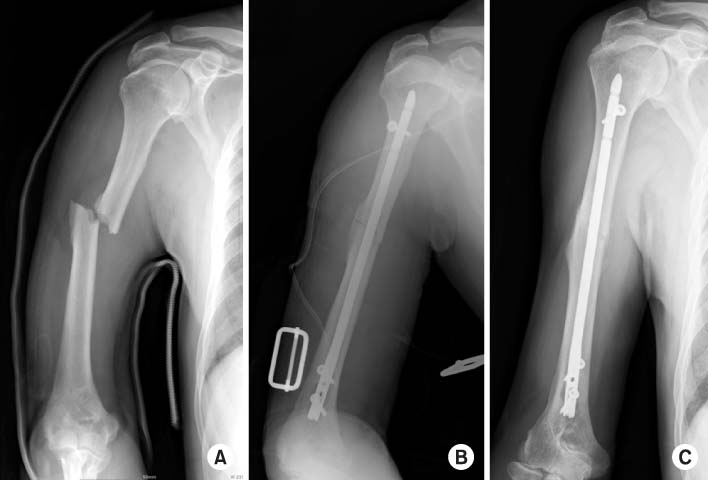
Fig. 2
(A) Initial radiographs show a short oblique fracture of the humeral shaft area.
(B) After fixation by a retrograde intramedullar nail, the fracture site was reduced, with a minimal gap.
(C) At postoperative 5 months, the fracture site was completely united.
Fig. 1
Fig. 2
Treatment of Humeral Shaft Fracture with Retrograde Intramedullary Nail
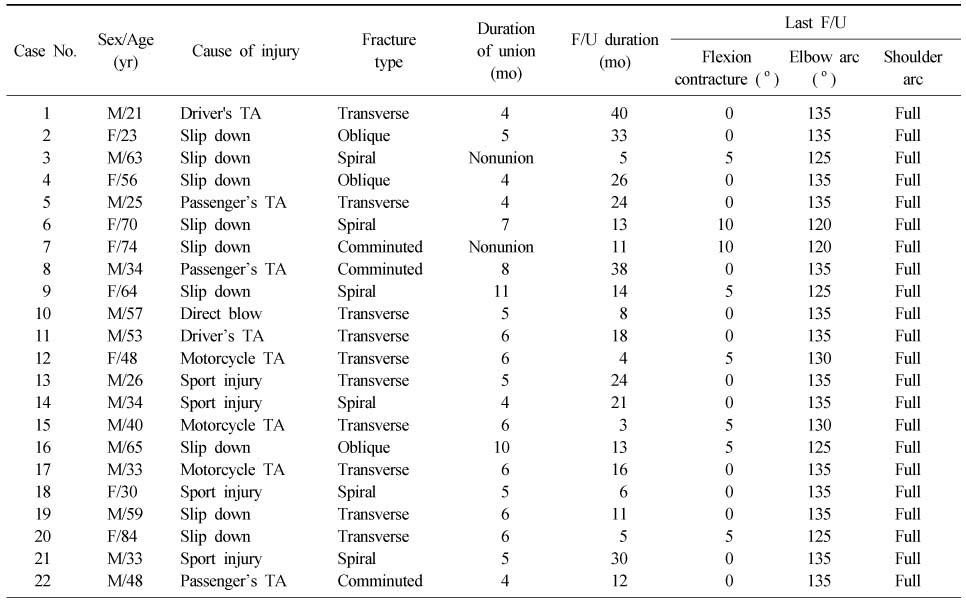
Summary of Cases
M: Male, F: Female, TA: Traffic accident, F/U: Follow up.
Table 1
Summary of Cases
M: Male, F: Female, TA: Traffic accident, F/U: Follow up.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

