-
How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
-
Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
-
J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00024
-
-
 Abstract Abstract
 PDF PDF
- Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
-
Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
-
Received February 19, 2025 Accepted May 15, 2025 Published online June 26, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00122
-
-
 Abstract Abstract
- Background
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
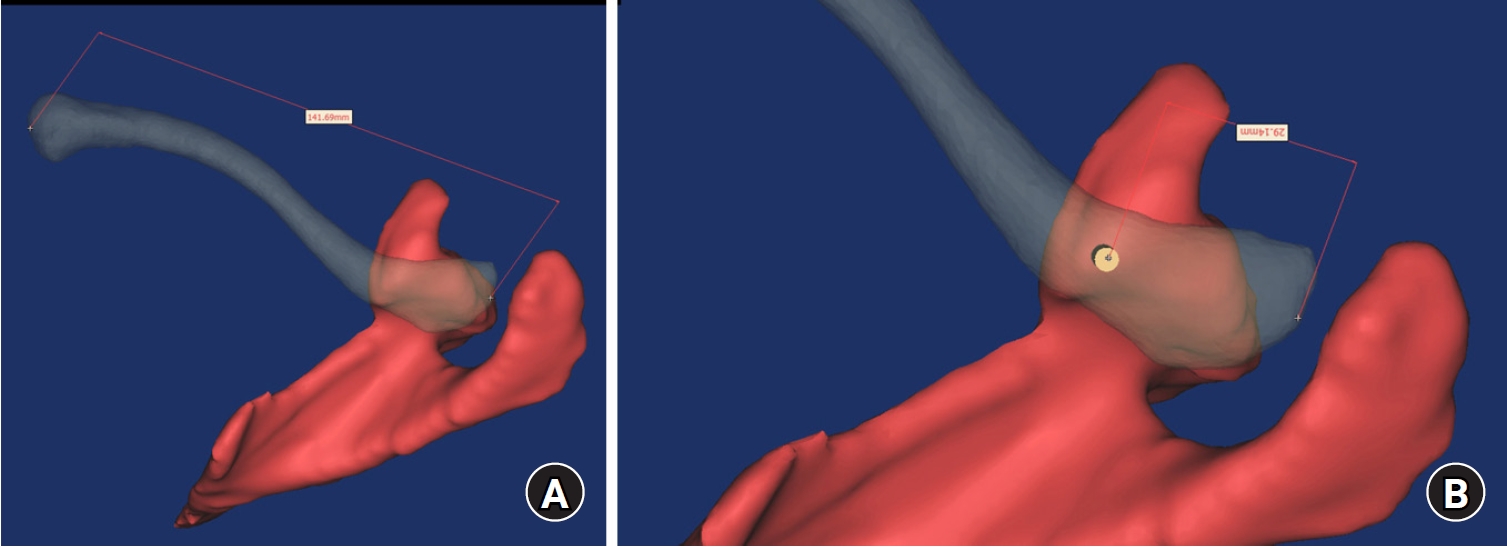
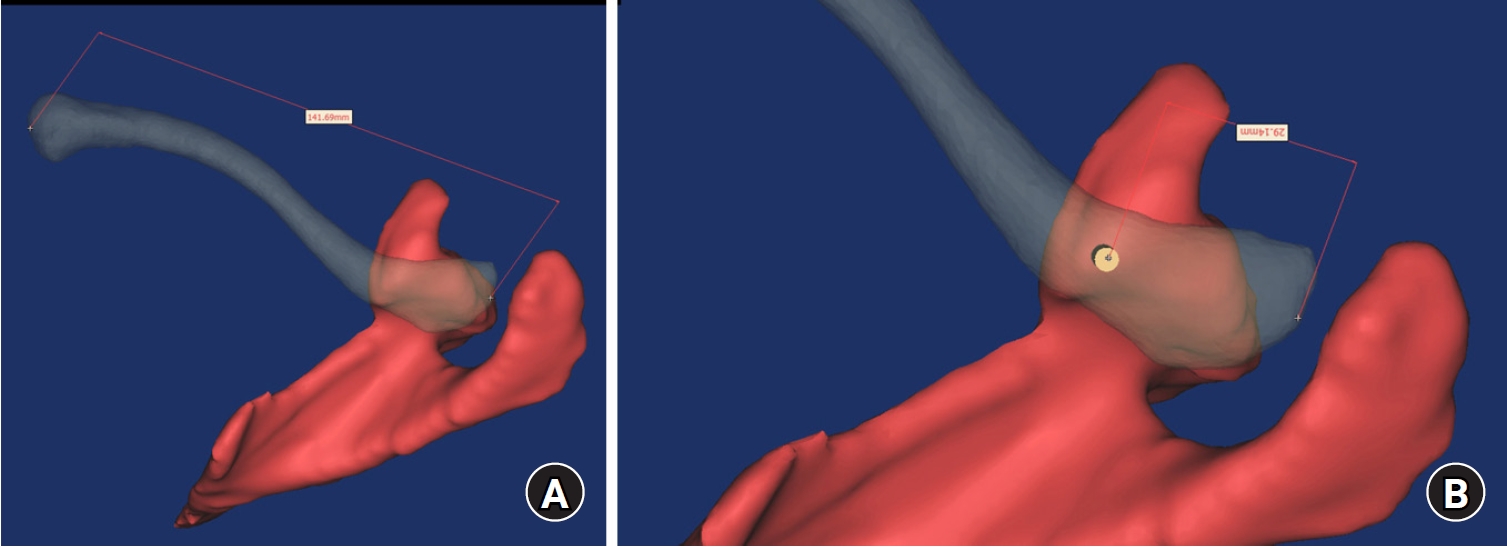
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The scan data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate. Anatomic features were assessed.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2‒62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusion
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment.
Level of evidence: IV
-
Biomechanical finite element analysis of a Femoral Neck System fixation construct for femur neck fractures and clinical implications
-
Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
-
Received February 18, 2025 Accepted April 17, 2025 Published online June 26, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00108
-
-
 Abstract Abstract
- Background
This study assessed the structural/mechanical stability of fixation constructs with a Femoral Neck System (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications of the findings.
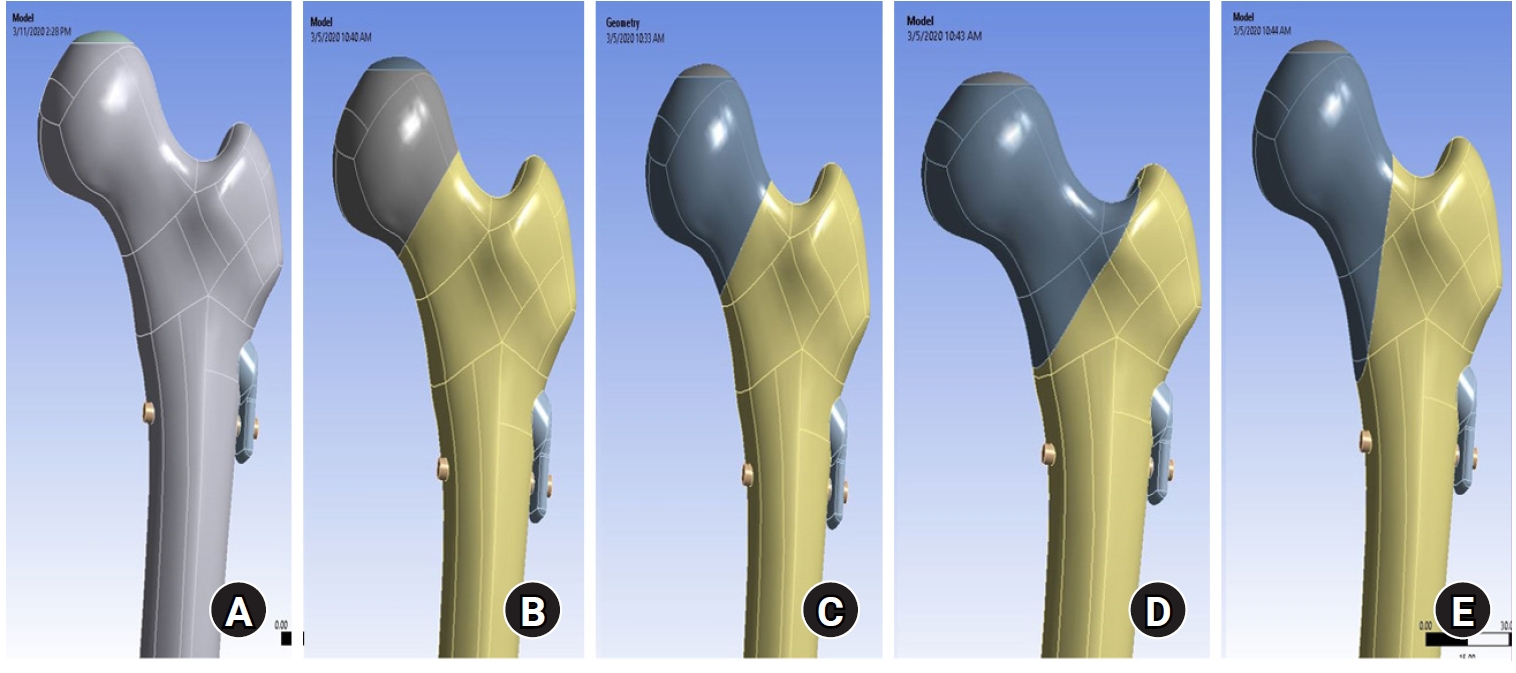
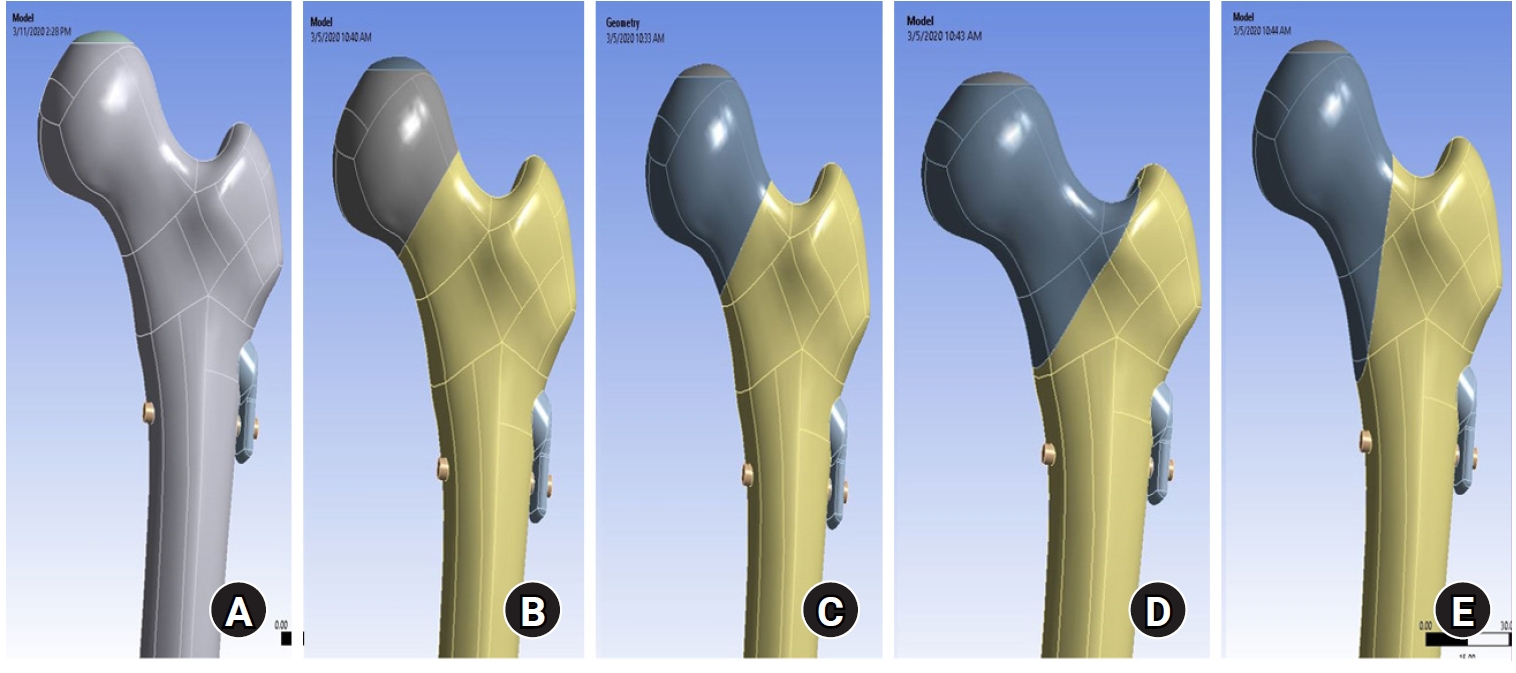
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur model (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital fracture, 68.56 MPa for a transcervical fracture, 344.54 MPa for a basicervical fracture, and 130.59 MPa for a vertical fracture. The maximum VMS of FNS was 840.34 MPa for a subcapital fracture, 637.37 MPa for a transcervical fracture, 464.07 MPa for a basicervical fracture, and 421.01 MPa for a vertical fracture. The maximum VMS of the implant corresponded to the value of the entire fixation construct; thus, FNS mainly functioned as a load-bearing implant. When we compared basicervical and vertical fractures, the stress distribution between the implant and the fracture sites differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
Considering the stress distribution of the assembly model, FNS fixation should be performed with consideration the osseous anchorage between the proximal bolt and cancellous bone of femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution.
Level of evidence: IV.
|