Abstract
-
Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
-
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
-
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
-
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery.
-
Level of evidence
III.
-
Keywords: Femoral neck fractures, Femur neck, Femoral neck system, FNS, Complication
Introduction
Femoral neck fracture (FNF), a prevalent type of orthopedic injury, poses unresolved challenges [
1]. The femoral neck system (FNS; DePuy Synthes), introduced for the dynamic fixation of the femoral neck with angular stability, has largely replaced traditional fixation methods. Compared with multiple cannulated cancellous screws (CCS), FNS facilitates the achievement of stronger fixation owing to the presence of the screw-plate construct [
2]. Furthermore, the integration of a blade and an anti-rotation screw in this method enhances the axial and rotational stability [
3]. In contrast to dynamic hip screws (DHS), the FNS technique involves minimal soft tissue stripping. Thus, it is a minimally invasive technique with a reduced risk of bleeding [
4,
5].
FNF classified as Pauwel types 1 and 2 were fixed with three CCS as a minimally invasive strategy initially. In contrast, FNF classified as Pauwel type 3 were fixed with an angular stable device to overcome shear force caused by the vertical fracture line. Because FNS provides angular stability with minimally invasive feature [
2], theoretically, it can be used for the management of all Pauwel types.
Several studies have compared FNS with traditional fixation implants [
2,
4-
7]. However, to the best of our knowledge, studies exploring the complications associated with FNS are limited. Therefore, this study used the random forest technique, a machine learning method, to identify the factors associated with the incidence of complications following surgical fixation with FNS.
Methods
Ethics Statement
The study was approved by the Institutional Review Board (IRB) of Asan Medical Center (Asan Institute for Life Science, approval no.: 2016-0932) and performed in accordance with the principles of the Declaration of Helsinki. The need for written informed consent was waived by the IRB.
Study Population
The medical records of patients aged ≥18 years who had presented to two university teaching hospitals with FNFs between July 2019 and February 2024 were retrospectively analyzed in this retrospective observational study. Only patients who had undergone surgical treatment using FNS were included in the present study. Patients who presented with pathologic or neglected fractures were excluded. Finally, 57 patients were included in the analysis. The patients were divided into two groups, the control and complication groups, according to the presence of complications—specifically, osteonecrosis of the femoral head (ONFH), nonunion, and peri-implant fracture—in univariate analysis.
Study Variables
The demographic data, perioperative profiles, and postoperative and radiographic outcomes were evaluated to identify the risk factors for the incidence of complications following the fixation of FNS.
The demographic characteristics evaluated included age, sex, fracture site, mechanism of injury, body mass index (BMI), smoking, Charlson comorbidity index (CCI) [
8], American Society of Anesthesiologists (ASA) classification [
9], preoperative Koval score [
10], Garden type [
11], Pauwels classification [
12], AO classification [
13] and follow-up length.
The perioperative profiles and outcomes evaluated comprised the time to surgery, length of stay, implant profile, the position of the bolts, neck-shaft alignment, tip-apex distance (TAD), neck shortening, and complications. The implant profile included the number of plate holes and the length of the bolt. The bolt position was measured in the anteroposterior (AP) and lateral views [
14]. The bolt position in the AP view was classified as follows: superior, center, and inferior. The bolt position in the lateral view was classified as follows: anterior, center, and posterior. The preoperative neck-shaft angle (NSA), postoperative NSA [
15], and deviation in the Garden alignment index (GAI) [
16] were measured to determine the neck-shaft alignment. GAI was measured by the angle between trabecular line in the femoral head and the longitudinal axis of the femoral shaft’s medial cortex. The difference between the affected and contralateral sides was defined as the deviation of GAI, which was used to evaluate the quality of fracture reduction.
The TAD was measured in the AP and lateral views, and the sum of the TAD values in both views was calculated using the methods described by Geller et al. [
17]. Neck shortening at the final follow-up visit was measured using the methods described by Zheng et al. [
7]. As described in the methods of Geller et al. [
17] and Zheng et al. [
7], the magnification of radiographs was considered when measuring the TAD and neck shortening with the diameter of the bolt fixed at 10 mm. Complication was evaluated as ONFH, nonunion, and peri-implant fracture during the follow-up period. For cases of ONFH, the presence of sclerotic lesions was assessed on simple AP and translateral radiographic views up to the final follow-up visit. If ONFH of Ficat-Arlet classification stage I [
18] or higher was suspected, additional magnetic resonance imaging (MRI) was performed to confirm the lesion. Nonunion was defined as fixation failure, characterized by implant breakage, loss of reduction, or a persistent fracture line visible on radiographs at a minimum of 6 months postoperatively. The incidence of complications such as ONFH, cut-out or through penetration, and peri-implant fracture during the follow-up period was evaluated.
Univariate analysis was conducted using SPSS ver. 23.0 (IBM Corp.). Categorical variables were assessed using the chi-square test or Fisher exact test, whereas categorical variables were assessed using the independent t-test. Continuous data are presented as the means and standard deviations. Statistical significance was set at P<0.05. Bonferroni correction was applied for multiple comparisons.
The machine learning method random forest was implemented using Python programming language (ver. 3.8, Python Software Foundation) for risk factor analysis [
19-
21]. The analysis aimed to identify the key predictors associated with complications. Age, sex, fracture site, mechanism of injury, BMI, smoking, CCI, ASA, preoperative Koval score, Garden type, Pauwels type, AO classification, time to surgery, length of hospital stay, implant profiles, bolt position, neck-shaft alignment, TAD, and neck shortening were included as independent variables. This left a set of variables that represent potential demographic, procedural, and clinical factors contributing to complications. A stratified sampling approach was used to split the dataset into training (80%) and testing (20%) subsets. This approach ensured that both classes of the target variable (complication, 1 and complication, 0) were proportionally represented in each subset.
A random forest classifier comprising 100 decision trees with default hyperparameters was employed. The Gini impurity criterion was used to optimize node splits, thereby maximizing the class purity within each split. The feature importance scores were computed based on the mean decrease in impurity across all decision trees to facilitate the identification of the variables most strongly associated with the outcome. A comprehensive set of metrics, encompassing accuracy, precision, recall, F1 score, and area under the receiver’s operating curve (ROC-AUC), was used to assess model performance.
Results
Univariate Analysis
The control and complication groups comprised 47 and 10 patients, respectively (
Table 1). Comparisons are presented as ‘control vs. complication group’ throughout the manuscript. No significant differences were observed between the groups in terms of age (58.0±14.0 vs. 55.1±11.2; P=0.542), distribution of female patients (62% and 50%; P=0.504), or other demographic data such as injury mechanism, BMI, smoking, CCI, ASA, preoperative Koval score, and follow-up length. Severe type of fracture pattern (Garden type 3 and 4, 41% vs. 70%; Pauwels type 3, 47% vs. 60%) was more prevalent in the complication group; however, the differences did not reach statistical significance.
Table 2 presents the perioperative profile and outcomes. No significant differences were observed between the groups in terms of time to surgery or length of stay. Similarly, no significant differences were observed between the groups in terms of the number of holes (2-hole, 30% vs. 40%; P=0.709) or bolt length (86.0±7.1 vs. 91.5±12.0; P=0.189). The bolt was positioned at the center in the AP view in 70% and 50% of cases in the control and complication groups, respectively (P=0.193). The bolt was positioned at the center in the lateral view in 87% and 90% of cases in the control and complication groups, respectively (P=0.530). In addition to greater GAI deviation (4.3±4.4 vs. 9.5±11.1; P=0.177), greater preoperative (137.6°±12.0° vs. 134.9°±12.0°; P=0.514) and postoperative (135.8°±5.6° vs. 132.8°±16.7°; P=0.595) varus-NSA were observed in the complication group; however, these differences did not reach statistical significance. The TAD in the AP view (8.4±2.6 mm vs. 5.9±2.3 mm; P=0.008) and the sum of TAD (16.7±5.3 mm vs. 12.1±4.0 mm; P=0.012) were significantly lower in the complication group. Greater neck shortening was observed in the complication group (2.3±3.0 mm vs. 4.9±2.3 mm; P=0.011). ONFH, cut-out or through penetration, and peri-implant fracture were observed in six patients, three patients, and one patient, respectively (
Table 3).
Surgical Complication Analysis
The random forest model achieved moderate performance in predicting the incidence of complications, with an accuracy of 83.3%. The model achieved a precision of 50.0%, indicating that only half of the predicted positive cases were correct. The model achieved a recall of 50.0%, indicating that some true positive cases were overlooked. The F1 score, which represents the harmonic mean of precision and recall, was 50.0%. This finding indicated that the ability of the model to balance precision and recall was limited. The ROC-AUC score was 0.95, indicating that the model possesses strong discriminative ability. However, the real-world predictive power of the model may have been limited owing to the low recall and precision.
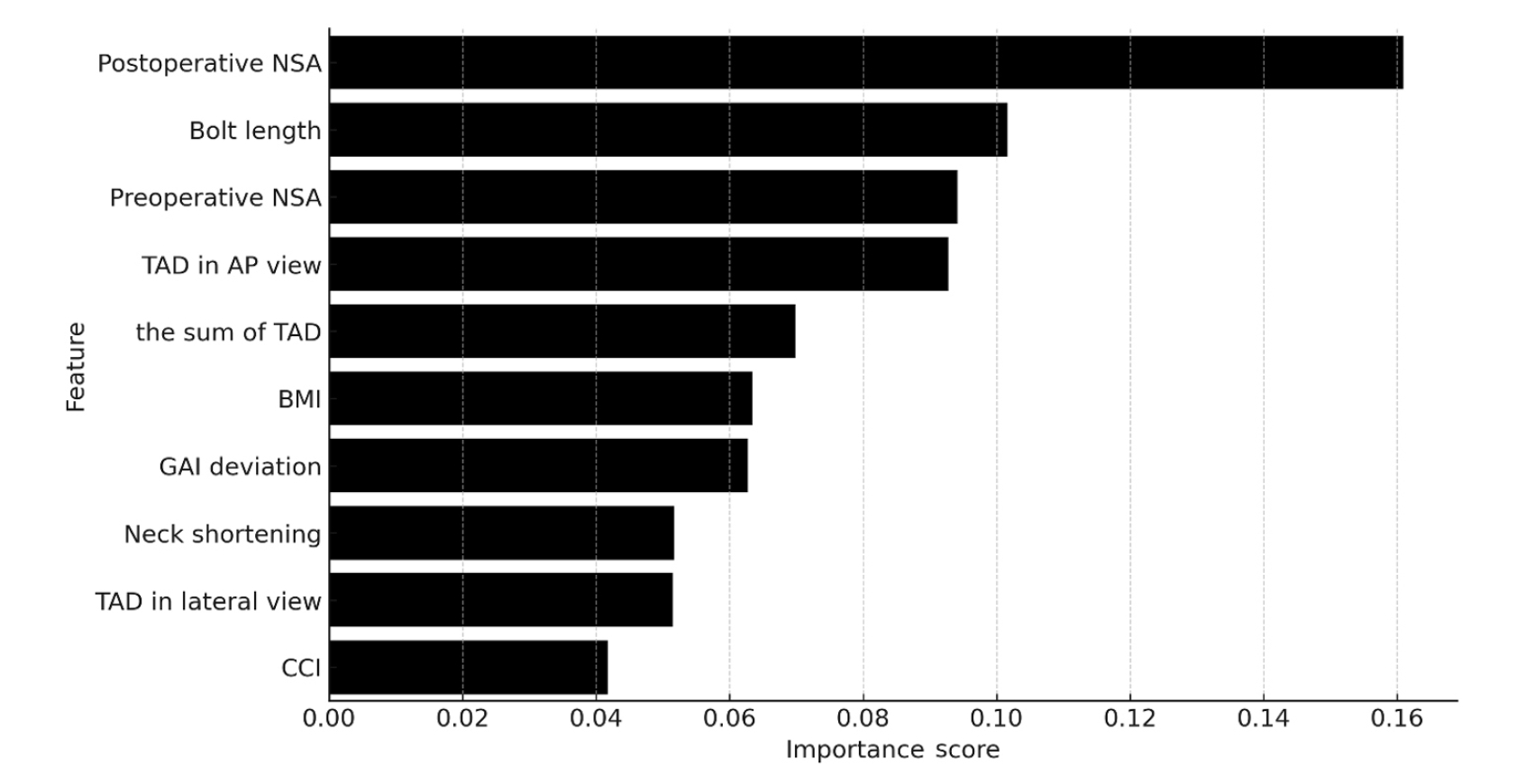
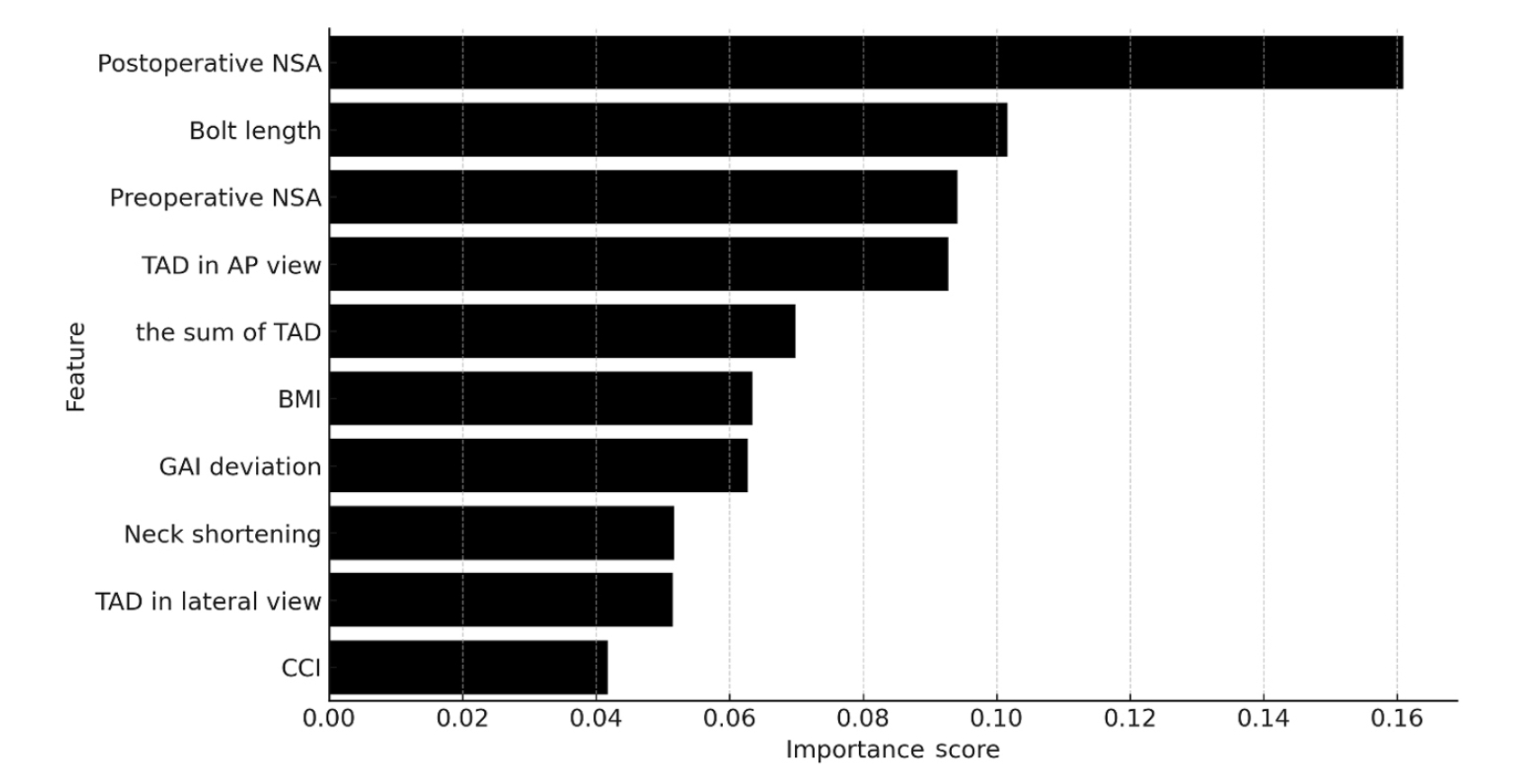
Feature importance analysis identified postoperative NSA (0.161) as the most significant predictor, followed by the length of the bolt (0.102) and preoperative NSA (0.094). A bar chart ranking the 10 most important features was generated to visualize the importance scores, highlighting the relative impact of each variable (
Fig. 1).
Discussions
Univariate comparative analysis revealed that a shorter TAD and greater neck shortening were observed in the complication group. However, risk factor analysis using the random forest model identified postoperative NSA as the most important predictor of complications.
Although TAD, neck shortening, and NSA are clinically significant, the postoperative NSA warrants particular attention, given its relationship with other factors. However, the relatively small sample size of the present study complicated the application of the random forest model. Thus, further studies with a larger dataset must be conducted in the future.
Traditionally, classification systems such as the Garden classification system and Pauwels classification system were used to classify FNF [
11,
12]. However, these classification systems did not exert a statistically significant impact on prognosis in the present study. Pauwels classification helps identify clearer treatment pathways, as vertically oriented fractures (Pauwel type 3) can be managed relatively well by selecting an appropriate fixation construct. DHS and anti-rotation screws, which were traditionally used for its management, have been replaced with FNS in recent years [
22]. Garden classification can indicate the disruption of blood supply to femoral neck related with initial injury, which is difficult to address through surgical procedures. Although not statistically significant, the notable discrepancy in the proportion of Garden type 4 fractures (17% vs. 50%) indicates a potential clinical impact, warranting further investigation.
A TAD value of <25 mm was considered in previous studies [
17]. Thus, the clinical impact for the TAD value (control vs. complication, 16.7 vs. 12.1 mm) was difficult to interpret in the present study, despite the significant difference observed between the two groups. Nevertheless, the findings of previous studies indicate that the complication and control groups underwent surgery with excellent TAD values. Notably, the TAD in the complication group was lower than that in the control group. Severe fracture types were presumed to contribute to TAD in that surgeons may insist on performing firm fixation to achieve optimal outcomes; however, this approach results in the insertion of the FNS bolt close to the subchondral bone of the femoral head. Zhou et al. [
23] reported that a short screw-apex distance may be associated with ONFH. FNS has anti-rotation screws directed to the apex of the femoral head; thus, the short TAD may have influenced the incidence of complications.
Adverse events such as cortical comminution of the severed end, fracture fractionation, and improper reduction may lead to neck shortening after fixation [
6]. This observation indicates that neck shortening is associated with the incidence of complications. However, neck shortening cannot be detected immediately after surgery; it becomes apparent over a period of weeks to months. Thus, care should be taken to minimize the risk of neck shortening during FNS surgery.
Univariate analysis revealed no significant differences between the groups in terms of the postoperative NSA. However, risk factor analysis conducted using the random forest model identified postoperative NSA as the most important feature (0.161), suggesting a strong relationship between this anatomical measurement and the incidence of complications. In situ fixation is sometimes performed during osteosynthesis in cases with stable fractures such as Garden type I or II. However, the quality of reduction plays a crucial role in improving the poor prognosis associated with unstable FNFs [
24]. Unstable FNFs are inherently associated with a higher risk of complications than stable FNFs; thus, postoperative NSA is one of the few modifiable factors in the osteosynthesis process for unstable FNFs [
25]. Subtle variations in the alignment influence the biomechanical stability and stress distribution [
26]. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery.
This study has certain limitations. First, the relatively small sample size may have led to the low model performance score of the random forest model. In particular, there was a discrepancy between the results of the univariate analysis and the random forest model. While this can be attributed to the fundamental differences between the two analytical approaches, we acknowledge that the small sample size in our study may have limited the reliability of the random forest analysis. Further studies with larger sample sizes must be conducted to address this limitation. Second, variables with relatively lower importance were also considered owing to the retrospective study design. This may have affected the modeling process. Although this is a strength of the random forest model, the results must be interpreted with caution in conjunction with sample size considerations. Third, the follow-up period was short and inconsistent. This may have limited the detection of long-term complications and introduced variability in outcome assessment. Thus, cases with sufficient and consistent follow-up must be selected in future studies. Fourth, malunions such as varus deformity and femoral neck shortening were not specifically classified as complications, despite their potential to cause clinical problems. Although the degree of reduction was evaluated using the GAI deviation (9.5° in the complication group vs. 4.3° in the control group), a more detailed analysis focusing on malunion-related outcomes may provide additional clinical insights in future studies. In addition, not all patients were screened with MRI for ONFH among the complications as routinely, which may also have led to underestimation. According to previous studies, the incidence of asymptomatic ONFH that cannot be identified on plain radiographs after FNFs has been reported to be as high as 34.2% [
27]. Further research is warranted to investigate this issue.
Conclusions
Risk factor analysis conducted using the random forest model identified postoperative NSA as the most important feature for postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery.
Article Information
-
Author contribution
Conceptualization: CHK, JWK. Data curation: HCS, JWK. Formal analysis: HSK, JWK, EJL. Supervision: JWK. Writing – original draft: EJL, HSK, HCS. Writing – review & editing: CHK, JWK. All authors read and approved the final manuscript.
-
Conflicts of interest
Ji Wan Kim is the Deputy Editor of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
Fig. 1.Top 10 feature importance ranked by the random forest model in predicting complications. NSA, neck-shaft angle; TAD, tip-apex distance; AP, anteroposterior; BMI, body mass index; GAI, Garden alignment index; CCI, Charlson comorbidity index.
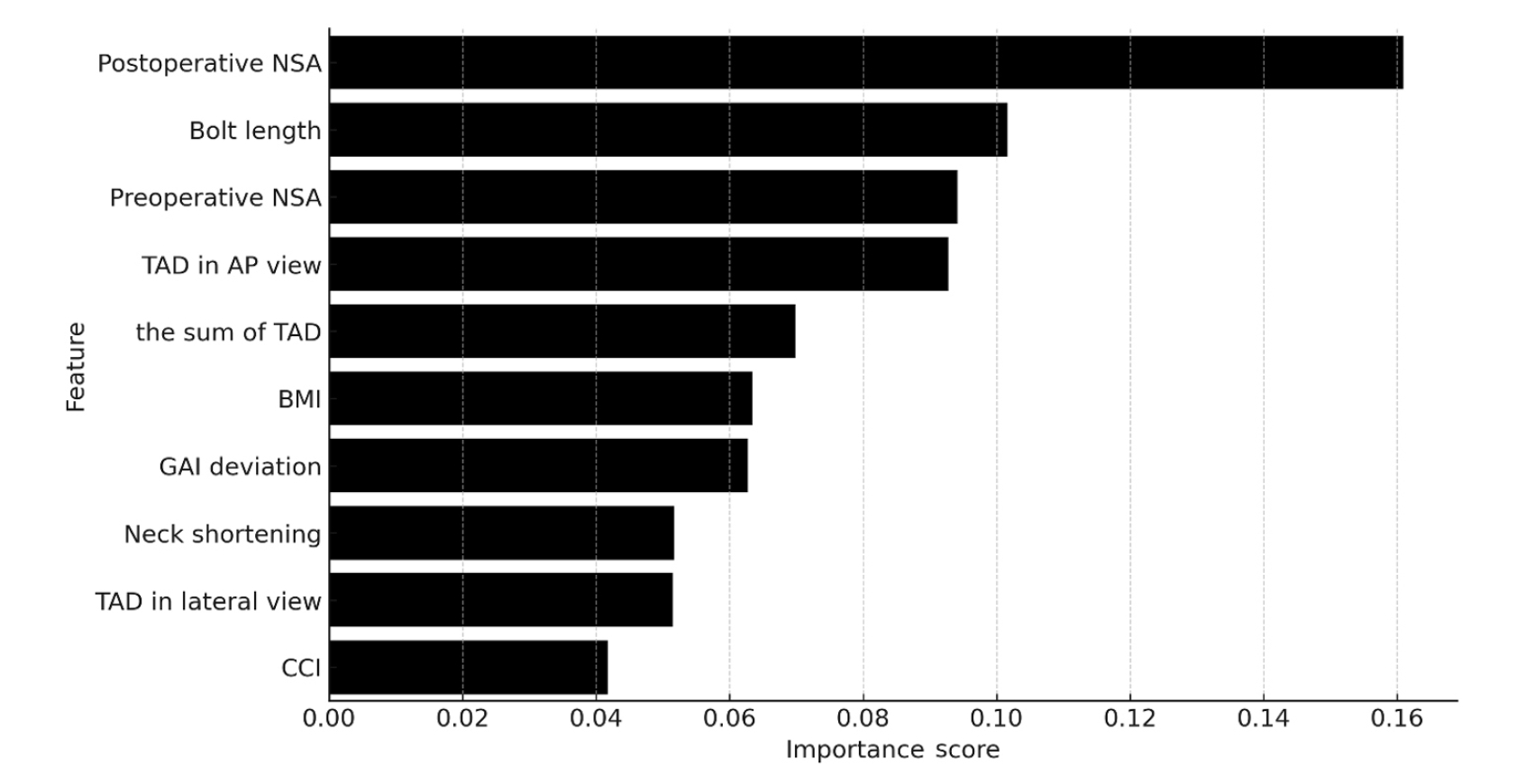
Table 1.Demographic data and fracture characteristics
|
Characteristic |
Control group (n=47) |
Complication group (n=10) |
P-value |
|
Age (yr) |
58.0±14.0 |
55.1±11.2 |
0.542 |
|
Female sex |
29 (62) |
5 (50) |
0.504 |
|
Left side |
21 (45) |
6 (60) |
0.492 |
|
Mechanism of injury |
|
|
0.447 |
|
Simple fall |
30 (64) |
9 (90) |
|
|
Fall from height |
12 (25) |
1 (10) |
|
|
Motor vehicle crash |
5 (11) |
0 (0) |
|
|
BMI (kg/m2) |
21.8±3.1 |
22.5±3.2 |
0.481 |
|
Smoker |
7 (15) |
2 (20) |
0.650 |
|
CCI |
|
|
0.539 |
|
0–3 |
30 (64) |
6 (60) |
|
|
4–6 |
13 (28) |
2 (20) |
|
|
7–9 |
4 (8) |
2 (20) |
|
|
ASA |
|
|
0.744 |
|
I |
16 (34) |
2 (20) |
|
|
II |
21 (45) |
6 (60) |
|
|
III |
10 (21) |
2 (20) |
|
|
Koval scorea)
|
|
|
0.482 |
|
1 |
26 (55) |
6 (60) |
|
|
2 |
4 (9) |
0 (0) |
|
|
3 |
2 (4) |
0 (0) |
|
|
4 |
0 (0) |
1 (10) |
|
|
5 |
14 (30) |
3 (30) |
|
|
6 |
1 (2) |
0 (0) |
|
|
Garden type |
|
|
0.115 |
|
1 |
18 (38) |
3 (30) |
|
|
2 |
10 (21) |
0 (0) |
|
|
3 |
11 (24) |
2 (20) |
|
|
4 |
8 (17) |
5 (50) |
|
|
Pauwels type |
|
|
0.556 |
|
1 |
7 (15) |
0 (0) |
|
|
2 |
18 (38) |
4 (40) |
|
|
3 |
22 (47) |
6 (60) |
|
|
AO classification |
|
|
0.882 |
|
31B1 |
27 (57) |
6 (60) |
|
|
31B2 |
20 (43) |
4 (40) |
|
|
Follow-up length (mo) |
16.4±11.6 |
20.9±10.0 |
0.256 |
Table 2.Perioperative profiles and outcomes
|
Variable |
Control group (n=47) |
Complication group |
P-value |
|
Time to surgery (day) |
0.91±1.0 |
0.60±0.8 |
0.366 |
|
Length of stay (day) |
7.5±9.8 |
5.6±2.8 |
0.561 |
|
Implant profile |
|
|
|
|
Number of holes |
|
|
0.709 |
|
1 |
33 (70) |
6 (60) |
|
|
2 |
14 (30) |
4 (40) |
|
|
Length of bolts |
86.0±7.1 |
91.5±12.0 |
0.189 |
|
Bolt position in AP view |
|
|
0.193 |
|
Superior |
1 (2) |
1 (10) |
|
|
Center |
33 (70) |
5 (50) |
|
|
Inferior |
13 (28) |
4 (40) |
|
|
Bolt position in lateral view |
|
|
0.530 |
|
Anterior |
4 (9) |
0 (0) |
|
|
Center |
41 (87) |
9 (90) |
|
|
Posterior |
2 (4) |
1 (10) |
|
|
Neck-shaft alignment (°) |
|
|
|
|
Preoperative NSA |
137.6±6.2 |
134.9±12.0 |
0.514 |
|
Postoperative NSA |
135.8±5.6 |
132.8±16.7 |
0.595 |
|
Garden index deviation |
4.3±4.4 |
9.5±11.1 |
0.177 |
|
TAD (mm) |
|
|
|
|
TAD in AP view |
8.4±2.6 |
5.9±2.3 |
0.008 |
|
TAD in lateral view |
8.3±3.1 |
6.2±3.4 |
0.054 |
|
Sum of TAD |
16.7±5.3 |
12.1±4.0 |
0.012 |
|
Neck shortening (mm) |
2.3±3.0 |
4.9±2.3 |
0.011 |
Table 3.
|
Complication type |
No. of cases (n=10) |
|
Osteonecrosis of femoral head |
6 |
|
Cut-out or through |
3 |
|
Peri-implant fracture |
1 |
References
- 1. Sundkvist J, Brüggeman A, Sayed-Noor A, Möller M, Wolf O, Mukka S. Epidemiology, classification, treatment, and mortality of adult femoral neck and basicervical fractures: an observational study of 40,049 fractures from the Swedish Fracture Register. J Orthop Surg Res 2021;16:561.ArticlePubMedPMCPDF
- 2. Xu Z, Sun J, Li J, et al. Comparative analysis of the femoral neck system (FNS) vs. cannulated cancellous screws (CCS) in the treatment of middle-aged and elderly patients with femoral neck fractures: clinical outcomes and biomechanical insights. BMC Musculoskelet Disord 2024;25:735.ArticlePubMedPMCPDF
- 3. Jiang X, Liang K, Du G, Chen Y, Tang Y, Geng K. Biomechanical evaluation of different internal fixation methods based on finite element analysis for Pauwels type III femoral neck fracture. Injury 2022;53:3115-23.ArticlePubMed
- 4. Moon JK, Lee JI, Hwang KT, Yang JH, Park YS, Park KC. Biomechanical comparison of the femoral neck system and the dynamic hip screw in basicervical femoral neck fractures. Sci Rep 2022;12:7915.ArticlePubMedPMCPDF
- 5. Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 2017;31:131-7.ArticlePubMed
- 6. Wang K, Lin D, Chen P, et al. Incidence and factors influencing neck shortening after screw fixation of femoral neck fractures with the femoral neck system. J Orthop Surg Res 2023;18:317.ArticlePubMedPMCPDF
- 7. Zheng S, Lin D, Chen P, et al. Comparison of femoral neck shortening after femoral neck system and cannulated cancellous screw fixation for displaced femoral neck fractures in young adults. Injury 2024;55:111564.ArticlePubMed
- 8. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51.ArticlePubMed
- 9. Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth 2011;55:111-5.ArticlePubMedPMC
- 10. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture: a prospective study in geriatric patients. Clin Orthop Relat Res 1995;(310):150-9.
- 11. Van Embden D, Rhemrev SJ, Genelin F, Meylaerts SA, Roukema GR. The reliability of a simplified Garden classification for intracapsular hip fractures. Orthop Traumatol Surg Res 2012;98:405-8.ArticlePubMed
- 12. Bartonícek J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma 2001;15:358-60.ArticlePubMed
- 13. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium: 2018. J Orthop Trauma 2018;32 Suppl 1:S1-170.Article
- 14. Bojan AJ, Beimel C, Taglang G, Collin D, Ekholm C, Jönsson A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord 2013;14:1.ArticlePubMedPMCPDF
- 15. Boese CK, Dargel J, Oppermann J, et al. The femoral neck-shaft angle on plain radiographs: a systematic review. Skeletal Radiol 2016;45:19-28.ArticlePubMedPDF
- 16. Yamakawa Y, Yamamoto N, Tomita Y, et al. Reliability of the garden alignment index and valgus tilt measurement for nondisplaced femoral neck fractures. J Pers Med 2022;13:53.ArticlePubMedPMC
- 17. Geller JA, Saifi C, Morrison TA, Macaulay W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop 2010;34:719-22.ArticlePubMedPDF
- 18. Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br 1985;67:3-9.ArticlePubMedPDF
- 19. Breiman L. Random forests. Mach Learn 2001;45:5-32.ArticlePDF
- 20. Kuhn M, Johnson K. Applied predictive modeling. Springer, 2013.
- 21. Hastie T, Tibshirani R, Friedman J. The elements of statistical learning. Springer, 2009.
- 22. Lim EJ, Shon HC, Cho JW, Oh JK, Kim J, Kim CH. Dynamic hip screw versus cannulated cancellous screw in Pauwels type II or type III femoral neck fracture: a systematic review and meta-analysis. J Pers Med 2021;11:1017.ArticlePubMedPMC
- 23. Zhou X, Guo S, Pan W, Zhang L, Ji H, Yang Y. The small screw-apex distance is potentially associated with femoral head osteonecrosis in adults with femoral neck fractures treated by closed reduction and percutaneous 3 parallel cannulated screws. BMC Musculoskelet Disord 2024;25:286.ArticlePubMedPMCPDF
- 24. Han S, Zhang ZY, Zhou K, et al. Positive buttress reduction in femoral neck fractures: a literature review. J Orthop Surg Res 2024;19:262.ArticlePubMedPMCPDF
- 25. Qiu L, Huang Y, Li G, Wu H, Zhang Y, Zhang Z. Essential role of reliable reduction quality in internal fixation of femoral neck fractures in the non-elderly patients: a propensity score matching analysis. BMC Musculoskelet Disord 2022;23:346.ArticlePubMedPMCPDF
- 26. Wang Y, Ma JX, Yin T, et al. Correlation between reduction quality of femoral neck fracture and femoral head necrosis based on biomechanics. Orthop Surg 2019;11:318-24.ArticlePubMedPMCPDF
- 27. Kim CH, Shin M, Lee D, Choi SJ, Moon DH. Hidden osteonecrosis of the femoral head after healed femoral neck fractures: magnetic resonance imaging study of 58 consecutive patients. Arch Orthop Trauma Surg 2022;142:1443-50.ArticlePubMedPDF
 , Hyun-Chul Shon, MD2
, Hyun-Chul Shon, MD2 , Han Soul Kim, MD3
, Han Soul Kim, MD3 , Ji Wan Kim, MD1
, Ji Wan Kim, MD1 , Eic Ju Lim, MD2
, Eic Ju Lim, MD2


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

