Search
- Page Path
- HOME > Search
Original Articles
- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
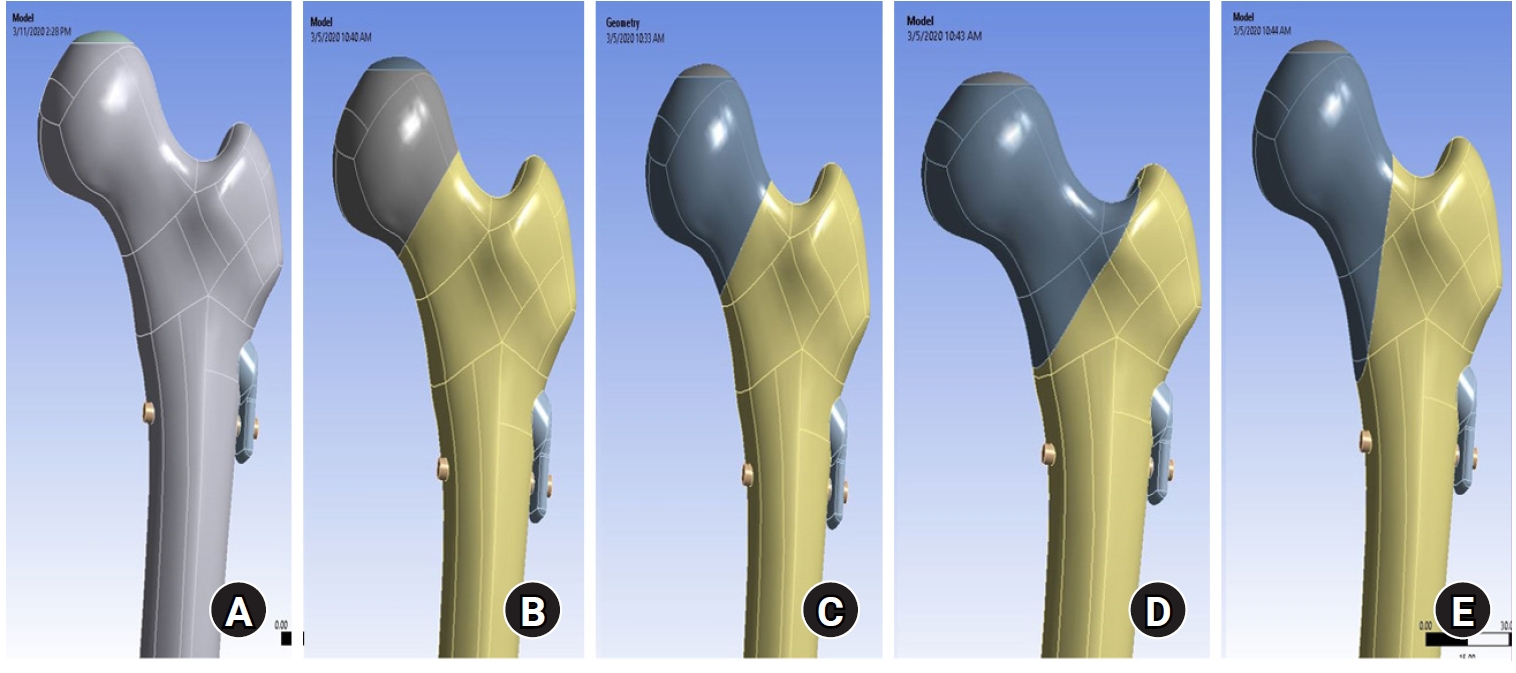
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV.
- 931 View
- 60 Download

- Intra-Articular Alterations after Suprapatellar Nailing in Tibial Shaft Fractures: An Arthroscopic Evaluation
- GwangChul Lee, Sung Hun Yang, Sung Min Jo, Jeong Min Kook
- J Korean Fract Soc 2022;35(4):129-134. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.129
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study attempted to study the intra-articular changes due to intramedullary nailing through the suprapatellar approach by evaluating the joint cartilage damage and presence of foreign bodies through a comparison of the pre- and post-operative status evaluated by knee arthroscopy.
Materials and Methods
This retrospective study analyzed fifteen patients who underwent intramedullary nailing through the suprapatellar approach for proximal tibial shaft fracture from January 2017 to March 2020. The condition of the joint cartilage and the presence of foreign substances in the patellofemoral joint were evaluated. The cartilage status of the patellofemoral joint was evaluated using the International Cartilage Repair Society (ICRS) grading system. Data from the ICRS grading and the visual analogue scale (VAS) scores of the femoral and patellar cartilage were compared to each independent variable surveyed.
Results
All the intra-articular structures before nailing were normal. In all cases after nailing, articular cartilage damage of the patellofemoral joint and intra-articular debris were observed. The average VAS score was 0.6 (0-1) before surgery and 2.27 (0-4) after surgery. There were no statistically significant differences except for the correlation in the diameter of the tibia nail and femoral ICRS grade (p=0.001) and the damage to the cartilage was greater in the femoral cartilage than that to the patella (p=0.001).
Conclusion
Intra-articular damage appears to be unavoidable in suprapatellar nailing. Further research is needed on the long-term effects of intra-articular damage and on methods to reduce this damage.
- 318 View
- 5 Download

Case Report
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture
- Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
- J Korean Fract Soc 2021;34(3):112-116. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.112
-
 Abstract
Abstract
 PDF
PDF - A helical blade type of hip screw is used widely for the operative management of femoral trochanteric fractures. A 73-year-old female patient was admitted for femoral trochanteric fracture AO/OTA type 31A2.2. A helical blade locking sleeve dissembled 18 weeks after surgery did not achieve accurate reduction. The patient underwent bipolar hip hemiarthroplasty because the fracture reduction was lost, and it was impossible to remove the remaining helical blade without bone loss. The authors report this case of a rare complication of helical blade.
- 367 View
- 2 Download

Review Article
- Pediatric around Elbow Fracture
- Taehun Kim, Jaeho Cho, Seungmin Chung
- J Korean Fract Soc 2021;34(1):44-49. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.44
-
 Abstract
Abstract
 PDF
PDF - This study assessed the current concepts of pediatric elbow fractures. PubMed and Embase databases were searched for publications in English on elbow fractures. Papers believed to yield significant findings to this area were included in this review. The supracondyle of humerus, lateral condyle of the humerus, proximal radius, and proximal ulna fractures were included. Sixteen papers and textbooks were selected. Pediatric elbow fractures should be evaluated for combined injuries. Treatment should be done accurately for each fracture for the further growth of children.
- 306 View
- 9 Download

Original Articles
- Comparison of the Clinical and Radiographic Results between 125° and 130° Caput-Collum-Diaphyseal Angle Proximal Femoral Nail Anti-Rotation II in Patients with Intertrochanteric Fracture
- Soo Jae Yim, Yong Bok Park, Hyun Kwon Kim, Sin Hyung Park
- J Korean Fract Soc 2020;33(4):210-216. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.210
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiographic results of two proximal femoral nail antirotation II (PFNA-II) angled by 125° and 130° in patients with intertrochanteric fractures.
Materials and Methods
From March in 2015 to September in 2016, 65 patients who underwent a closed reduction and internal fixation with PFNA-II for a femoral intertrochanteric fracture were evaluated retrospectively. The minimum follow-up period was two years. Of those, 30 and 35 patients underwent 125° angled PFNA-II and 130° angled PFNA-II, respectively. The clinical performance was evaluated using the Harris hip score, WOMAC (Western Ontario and McMaster Universities Osteoarthrtis Index), and UCLA (University of California Los Angeles) score. Radiographic analyses were performed using standardized anteroposterior and lateral radiographs to assess the implant position and quality of reduction. The blade length, distance between the blade tip and the tip of the greater trochanter, and distance between the blade tip and the most lateral protrusion point of the greater trochanter in the two groups were measured and compared.
Results
The clinical results, including the Harris hip score, WOMAC, and UCLA, were similar in the two groups at the last follow-up postoperatively. In the radiography evaluation, the implant position, quality of reduction, and the blade length were similar in the two groups. The distances between the blade tip and the tip of the greater trochanter were 52.60±3.53 mm and 58.07±5.54 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The distance between the blade tip and the most lateral protrusion point of greater trochanter were 16.48±2.54 mm and 21.19±4.43 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The differences were significant (p=0.031, p=0.012).
Conclusion
The operation with the 125° angled PFNA-II showed a more superior and lateral position of the blade than that with the 130° angled PFNA-II. Nevertheless, lateral thigh pain can occur when the blade is positioned superolaterally.
- 335 View
- 1 Download

- Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
- J Korean Fract Soc 2020;33(4):179-188. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 450 View
- 3 Download
- 1 Crossref

Case Report
- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
- Yongun Cho, Jai Hyung Park, Se Jin Park, Ingyu Lee, Eugene Kim
- J Korean Fract Soc 2019;32(4):222-226. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.222
-
 Abstract
Abstract
 PDF
PDF - This paper reports the use of a traction device for the treatment of neglected proximal interphalangeal fracture dislocations. A 44-year-old man with a fracture dislocation of a right ring finger proximal interphalangeal joint was admitted 17 days after the injury. Closed reduction and external fixation were performed using a dynamic traction device and C-arm under a brachial plexus block. Passive range of motion exercise was started after two weeks postoperatively and active range of motion exercise was started after three weeks. The traction device was removed after five weeks. No infection occurred during the traction period. No subluxation or displacement was observed on the X-ray taken two months postoperatively. The active range of motion of the proximal interphalangeal joint was 90°. The patient was satisfied with the functional result of the treatment with the traction device. The dynamic traction device is an effective treatment for neglected fracture dislocations of the proximal interphalangeal joint of a finger.
- 793 View
- 1 Download

Original Articles
- Use of a Distraction Dynamic External Fixator in the Treatment of Comminuted Middle Phalanx Base Fractures
- Sang Woo Kim, Chae Chil Lee, Sang Hun Ko, Il Yeong Hwang, Min Seok Kim, Woo Young Jin
- J Korean Fract Soc 2019;32(1):1-5. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This paper suggests the use of distraction dynamic external fixators (DDEF) for the treatment of proximal middle phalanx fractures.
MATERIALS AND METHODS
Seven patients, who were diagnosed with comminuted intra-articular fractures at the base of the middle phalanx from February 2014 to November 2016, were enrolled in this study (volar aspect 6 cases, dorsal aspect 1 case). They underwent a closed reduction under a C-arm image intensifier, and DDEF was applied with general anesthesia. Range of motion (ROM) exercise was encouraged after 3 to 5 days postoperatively, and DDEF was removed after 5 weeks. Subluxation, angulation and displacement were evaluated 6 weeks postoperatively.
RESULTS
The patients who were treated with DDEF showed a normal proximal interphalangeal joint ROM (100°), and there was no subluxation or displacement on the X-ray film 6 weeks postoperatively. In addition, there were no signs of infection, such as local heat, redness, and pus-like discharge.
CONCLUSION
DDEF helps maintain the reduction and reducing forces through the ligamentotaxis. The joint stiffness is reduced, which it makes early return to daily life easier. -
Citations
Citations to this article as recorded by- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
Yongun Cho, Jai Hyung Park, Se-Jin Park, Ingyu Lee, Eugene Kim
Journal of the Korean Fracture Society.2019; 32(4): 222. CrossRef
- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
- 627 View
- 0 Download
- 1 Crossref

- Computational Simulation of Multiple Cannulated Screw Fixation for Femoral Neck Fractures and the Anatomic Features for Clinical Applications
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2018;31(2):37-44. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.37
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To identify the anatomic features for clinical applications through a computational simulation of the fixation of three cannulated screws for a femoral neck fracture.
MATERIALS AND METHODS
Thirty cadaveric femurs underwent computed tomography and the images were transferred to the Mimics® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the 7.0 mm cannulated screw was performed to enable computerized virtual fixation of multiple cannulated screws for femoral neck fractures. After positioning the screws definitively for cortical support, the intraosseous position of the cannulated screws was evaluated in the anteroposterior image and axial image direction.
RESULTS
Three cannulated screws located at the each ideal site showed an array of tilted triangles with anterior screw attachment and the shortest spacing between posterior and central screws. The central screw located at the lower side was placed in the mid-height of the lesser trochanter and slightly posterior, and directed toward the junction of femoral head and neck to achieve medial cortical support. All the posterior screws were limited in height by the trochanteric fossa and were located below the vastus ridge, but the anterior screws were located higher than the vastus ridge in 10 cases. To obtain the maximum spacing of the anterior and posterior screws on the axial plane, they should be positioned parallel to the cervical region nearest the cortical bone at a height not exceeding the vastus ridge.
CONCLUSION
The position of cannulated screws for cortical support were irregular triangular arrangements with the anterosuperior apex. The position of the ideal central screw in the anteroposterior view was at the mid-height of the lesser trochanter toward the junction of the femoral head and neck, and the anterior and posterior screws were parallel to the neck with a maximal spread just inferior to the vastus ridge. -
Citations
Citations to this article as recorded by- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
Ju-Yeong Kim
Journal of the Korean Fracture Society.2023; 36(1): 1. CrossRef
- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- 443 View
- 0 Download
- 1 Crossref

Review Article
- Conservative Treatment of Proximal Humeral Fracture
- Hwansub Hyun, Jonghyun Ahn, Sang Jin Shin
- J Korean Fract Soc 2018;31(1):29-35. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.29
-
 Abstract
Abstract
 PDF
PDF - A proximal humeral fracture is an osteoporotic fracture that often occurs in elderly women. Approximately 80% of all proximal humeral fractures are non-displaced fractures, which can be treated with conservative treatment to achieve stable union. The treatment plan for fractures involving displaced and comminuted fractures is controversial. Malunion, avascular necrosis of the humeral head, and shoulder stiffness due to conservative treatment can occur but the functional deterioration is low and the patient satisfaction is high. The indications for the conservative management of proximal humeral fractures include a non-displaced fracture and a 2-part fracture, low-functional demanded 3-part fracture, and operative-limited 4-part fracture. Recently, the surgical indications have expanded as technological advances in surgical fixation methods and functional needs of elderly patients are increasing. Current treatment policy decisions tend to be determined by the personal preference and expert opinion rather than by evidence-based decision-making.
-
Citations
Citations to this article as recorded by- The Effect of Postoperative Korean Traditional Medicine for the of Proximal Humeral Fracture: A Case Report
Hyun Il Go, Hangyul Choi, Jieun Hong, Nam geun Cho
Journal of Acupuncture Research.2019; 36(1): 50. CrossRef
- The Effect of Postoperative Korean Traditional Medicine for the of Proximal Humeral Fracture: A Case Report
- 337 View
- 5 Download
- 1 Crossref

Original Article
- The Determination of Optimal Entry Point for Proximal Femoral Nail Antirotation-II by Fluoroscopic Simulation: A Cadaveric Study
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2017;30(4):173-179. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study seeks to determine the anatomically optimal entry point of proximal femoral nail antirotation-II (PFNA-II®) according to geographic features of Korean cadaveric femoral trochanters for successful reduction of osteoporotic proximal femoral fractures.
MATERIALS AND METHODS
Forty-three adult cadaveric femurs without previous fractures or surgeries were included. Anteroposterior (AP) and lateral images of all femurs and PFNA-II® were taken with an image intensifier. Using the image synthesis process via the image editing program (Adobe Photoshop CS6), the optimal entry point was verified and compared with the tip of the greater trochanter (GT) and the cervicotro-chanteric junction on AP images, as well as the width of the trochanter and the neck on lateral images.
RESULTS
The optimal entry point of PFNA-II® was an average distance of 9.1 mm (range, 7–15 mm) medially from the tip of GT on AP images. The center of the nail was located at an average of 30% (range, 21%–44%) area from the posterior margin of the middle neck, which is an average area of 38% (range, 26%–48%) from the posterior cortex of the trochanter on lateral images. Furthermore, the ideal entry point was at the extended line of the cervico-trochanteric junction.
CONCLUSION
The optimal entry point, which was found to be medial to the tip of the GT and posterior to the center of the middle femoral neck and the trochanter, was at on the extended line of the cervicotrochanteric junction. -
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef - Does the Entry Point of Proximal Femoral Nail Antirotation Affect the Malalignment of Intertrochanteric Fracture? A Cadaveric Study
Chittawee Jiamton, Nonpawit Nimmankiatkul, Pongsakorn Rungchamrassopa, Wichan Kanchanatawan, Pariyut Chiarapatanakom, Wirat Kongcharoensombat
Journal of Southeast Asian Orthopaedics.2022;[Epub] CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 1,061 View
- 27 Download
- 2 Crossref

Case Reports
- Medial Plating of Distal Femoral Fracture with Locking Compression Plate-Proximal Lateral Tibia: Cases' Report
- Se Ang Jang, Young Soo Byun, In Ho Han, Dongju Shin
- J Korean Fract Soc 2016;29(3):206-212. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.206
-
 Abstract
Abstract
 PDF
PDF - Generally, lateral plating is used for a comminuted fracture of the distal femur. However, in some cases, it has been shown that using a medial plate is necessary to achieve better outcome. Nevertheless, there are no available anatomical plates that fit either the distal medial femoral condyle or fracture fixation, except for the relatively short plate developed for distal femoral osteotomy. We found that locking compression plate-proximal lateral tibia (LCP-PLT) fits anatomically well for the contour of the ipsilateral medial femoral condyle. Moreover, LCP-PLT has less risk of breaking the thread holes since it rarely needs to be bent. We report a plastic bone model study and two cases of distal femoral fractures fixed with medial plating using LCP-PLT.
-
Citations
Citations to this article as recorded by- A novel anatomical locked medial femoral condyle plate: a biomechanical study
M. A. Ozer, S. Keser, D. Barıs, O. Yazoglu
European Journal of Orthopaedic Surgery & Traumatology.2024; 34(5): 2767. CrossRef - Medial plating of distal femur: which pre-contoured angular stable plate fits best?
Shaam Achudan, Rex Premchand Antony Xavier, Sze Ern Tan
European Journal of Orthopaedic Surgery & Traumatology.2024; 34(6): 3297. CrossRef - Medial augmentation of distal femur fractures using the contralateral distal femur locking plate: A technical note
Jaime Andrés Leal
OTA International.2024;[Epub] CrossRef - The missing piece of the trauma armoury-medial femoral condyle plate
Piyush Upadhyay, Farhan Syed, Darryl N Ramoutar, Jayne Ward
Injury.2022; 53(3): 1237. CrossRef - Surgical Tips and Tricks for Distal Femur Plating
Christopher Lee, Dane Brodke, Ajay Gurbani
Journal of the American Academy of Orthopaedic Surgeons.2021; 29(18): 770. CrossRef - Medial minimally invasive helical plate osteosynthesis of the distal femur – a new technique
G.M. Hohenberger, A.M. Schwarz, P. Grechenig, B. Clement, Mario Staresinic, Bore Bakota
Injury.2021; 52: S27. CrossRef - Feature-Based Design of Personalized Anatomical Plates for the Treatment of Femoral Fractures
Xiaozhong Chen, Zhijian Mao, Xi Jiang
IEEE Access.2021; 9: 43824. CrossRef
- A novel anatomical locked medial femoral condyle plate: a biomechanical study
- 826 View
- 44 Download
- 7 Crossref

- Medial and Lateral Dual Plate Fixation for Osteoporotic Proximal Humerus Comminuted Fracture: 2 Case Reports
- Sam Guk Park
- J Korean Fract Soc 2016;29(1):61-67. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.61
-
 Abstract
Abstract
 PDF
PDF - Some proximal humeral fractures in elderly patients are accompanied by medial metaphyseal comminution and quality of the bone is so poor that head preserving osteosynthesis seems to be amenable. In cases of medial metaphyseal comminution, lateral locking compression plate (LCP) fixation also has a tendency to become a matter of screw cut out or loss of fixation. The author reports on successful treatment of two osteoporotic proximal humeral fractures combined with medial meta-physeal comminution, with application of additional direct medial supporting plate fixation. Medial plate fixations were added when the fractures were still unstable after the conventional lateral LCP fixation and anterior circumflex humeral arteries had been ruptured before. The fixations were stable enough to start exercise immediately after surgery. The inclinations of the humeral neck were not changed until the last follow-up and clinical results were satisfactory without humeral head osteonecrosis which was a concern.
-
Citations
Citations to this article as recorded by- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
Hyun-Gyu Seok, Sam-Guk Park
Journal of Orthopaedic Trauma.2023; 37(10): e387. CrossRef - The plate fixation strategy of complex proximal humeral fractures
Qi Sun, Xiaoming Wu, Lei Wang, Ming Cai
International Orthopaedics.2020; 44(9): 1785. CrossRef - Biomechanical evaluation of a novel dualplate fixation method for proximal humeral fractures without medial support
Yu He, Yaoshen Zhang, Yan Wang, Dongsheng Zhou, Fu Wang
Journal of Orthopaedic Surgery and Research.2017;[Epub] CrossRef
- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
- 446 View
- 6 Download
- 3 Crossref

- Breakage of Cephalomedullary Nail Used in the Treatment of Proximal Femur Fractures: Case Report
- Seok Hyun Kweon, Chang Hyun Shin, Jin Sung Park, Byoung San Choi
- J Korean Fract Soc 2016;29(1):42-49. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.42
-
 Abstract
Abstract
 PDF
PDF - Internal fixation using a cephalomedullary nail as treatment for proximal femur fracture has recently been popular for early ambulation and rehabilitation. However metal breakage at the lag screw insertion site was reported due to non-union, delayed-union, and early weight bearing. In our orthopedic department, we experienced 2 cases of nail breakage at the lag screw insertion site, therefore we report on evaluation of the cause of metal failure and prevention of complications with literature review.
-
Citations
Citations to this article as recorded by- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
Asep Santoso, Ik-Sun Choi, Kyung-Soon Park, Taek-Rim Yoon
Hip & Pelvis.2017; 29(3): 199. CrossRef
- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
- 417 View
- 1 Download
- 1 Crossref

- Irreducible Open Dorsal Dislocation of the Proximal Interphalangeal Joint: A Case Report
- Youn Tae Roh, Il Jung Park, Hyoung Min Kim, Jae Young Lee, Sung Lim You, Youn Soo Kim
- J Korean Fract Soc 2015;28(1):65-70. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.65
-
 Abstract
Abstract
 PDF
PDF - Dorsal dislocation of the proximal interphalangeal joint is a common injury in the orthopedic department. In most cases, the joint is reduced simply by closed manipulation. However, in rare cases, the joint is not reducible by closed manipulation, therefore, surgery is required. We report on a case of irreducible open dorsal dislocation of the proximal interphalangeal joint which was surgically treated. Because the flexor tendon interposed between the head of the proximal phalanx and the base of the middle phalanx, we could reduce the joint only after repositioning of the flexor tendon.
- 312 View
- 2 Download

- Rupture of the Extensor Pollicis Longus Tendon at the Proximal Screw of Volar Plate Fixation for Distal Radius Fracture: A Case Report
- Dong Ju Shin, Seung Oh Nam, Hun Sik Cho
- J Korean Fract Soc 2013;26(4):338-342. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.338
-
 Abstract
Abstract
 PDF
PDF - As volar plate fixation of distal radius fracture becomes more common, reports of ruptured extensor pollicis longus tendon by a protruding distal screw tip are also increasing steadily. Authors have experienced a rare case of ruptured extensor pollicis longus tendon at the prominent proximal screw of fixed volar plate for distal radius fracture, and we report it herein with a review of the literature.
- 288 View
- 1 Download

Original Articles
- Comparative Study of Proximal Femoral Nail Antirotation and Zimmer Natural Nail for the Treatment of Stable Intertrochanteric Fractures
- Jee Hoon Kim, Oog Jin Shon
- J Korean Fract Soc 2013;26(4):305-313. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.305
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the results between Proximal femoral nail antirotation II (PFNA II) and Zimmer natural nail Asia type (ZNN) for the treatment of stable intertrochanteric fractures.
MATERIALS AND METHODS
Between September 2011 and September 2012, 40 consecutive patients with stable intertrochanteric femoral fractures were treated with PFNA II or ZNN. We reviewed 20 cases of PFNA II and 20 cases of ZNN prospectively. We evaluated the operation time, amount of bleeding, mean hospital day, and capability of mobility and function using 'mobility score of Parker and Palmer' and 'social score of Jensen'. We also evaluated the reduction state by the Fogagnolo, Cleveland index, change of tip and apex distance (TAD), sliding distance of cervical screw, change of neck shaft angle and bone union time.
RESULTS
There were no significant differences between the groups treated with PFNA and ZNN. Both groups showed good clinical results. PFNA showed less TAD change and ZNN showed a shorter sliding distance of cervical screw, but they were not statistically different. The bone union time was approximately 13 weeks in both groups.
CONCLUSION
PFNA and ZNN produced good clinical and radiologic results in the treatment of stable intertrochanteric fractures. There were no significant differences between the groups. Both implants provide good stability and union, so we can conclude that they are both suitable for the treatment of stable intertrochanteric fractures. -
Citations
Citations to this article as recorded by- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - Comparison of osteoporotic intertrochanteric fracture fixation using a proximal femoral nail with a helical blade and lag screw type proximal femoral nail
Woong Chae Na, Chae Won Lim, Sang Hong Lee
Medical Biological Science and Engineering.2018; 1(2): 45. CrossRef - BONE HEALING PATTERNS OF INTERLOCKED INTRAMEDULLARY NAIL-FIXATED FEMORAL SHAFT FRACTURES: AGE-MATCHED RADIOGRAPHIC PRESENTATION OF UNION PATTERN
Myung-Sang Moon, Dong-Hyeon Kim, Bong-Keun Park, Min-Geun Yoon
Journal of Musculoskeletal Research.2017; 20(02): 1750010. CrossRef - The Curative Effect Comparison Between Prolonged Third Generation of Gamma Nail and Prolonged Dynamic Hip Screw Internal Fixation in Treating Femoral Intertrochanteric Fracture and the Effect on Infection
Wenye He, Wei Zhang
Cell Biochemistry and Biophysics.2015; 71(2): 695. CrossRef
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- 1,423 View
- 1 Download
- 5 Crossref

- The Result of Conservative Treatment of Proximal Humerus Fracture in Elderly Patients
- Seung Gil Baek, Chang Wug Oh, Young Soo Byun, Jong Keon Oh, Joon Woo Kim, Jong Pil Yoon, Hyun Joo Lee, Hyung Sub Kim
- J Korean Fract Soc 2013;26(4):292-298. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
With the increase in the old age population, proximal humerus fractures have been increasing recently. However, complications after operative treatment, such as fixation failure, are common because of osteoporosis. We treated proximal humerus fractures in patients with osteoporosis conservatively, and evaluated the radiographic and functional results by analyzing the factors affecting the results.
MATERIALS AND METHODS
Nineteen out of 30 cases for whom the clinical follow-up was over 1 year were included in this retrospective study. There were 17 females and 2 males, and the mean age was 73.2 years. The causes were slip from a short height (18 cases) and a minor car accident (1 case). We evaluated the union period, nonunion, malunion and the Constant score and analyzed several factors affecting the functional result, such as age, fracture pattern, and malunion.
RESULTS
Seventeen cases (89.5%) obtained union within 12.8 weeks on average. Neck-shaft angle was 125.3degrees on average, with seven cases of malunion. The Constant score was 84.1 on average, and there were excellent scores in 11 cases, good scores in 4 cases, and fair scores in 2 cases. Fracture pattern, neck-shaft angle, or malunion did not affect the functional outcome, and elderly patients showed poorer shoulder function.
CONCLUSION
Proximal humeral fractures with osteoporosis may achieve a high rate of bony union when treated with conservative methods. Despite the common occurrence of malunion, a satisfactory functional outcome may be expected.
- 425 View
- 4 Download

- The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
- Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
- J Korean Fract Soc 2013;26(4):284-291. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.284
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to analyze the results of treating subtrochanteric femoral fractures with proximal femoral nail antirotation (PFNA).
MATERIALS AND METHODS
Twenty five consecutive patients diagnosed with subtrochanteric femoral fractures underwent intramedullary fixation using PFNA and followed-up for over 12 months. According to the Seinsheimer's classification, there were 2 type IIA, 9 type IIB, 2 type IIIA, 3 type IV and 9 type V. According to the AO classification, there were 10 type A, 9 type B and 6 type C. There were 16 cases of closed reduction group and 9 cases of limited open reduction group. Retrospectively, radiological outcomes were assessed at the union period, change of neck shaft angle, tip-apex distance, Cleveland index, sliding of lag screw and complication.
RESULTS
Union was achieved in 23 of 25 cases, over an average of 17 weeks. Limb length shortening below 2 cm occurred in 7 patients. The Cleveland index was shown in 80% of 5, 6, 8 and 9 zone; the tip apex distance was 19.6 mm; the mean sliding distance was 4.4 mm; and the mean change of femur neck and shaft angle was varus 3 degree at the final follow-up. Complications included 3 cases of delayed union and 2 cases of nonunion.
CONCLUSION
With its early bony union, ambulation, rehabilitation and low complication, PFNA is a useful and reliable choice for the treatment of subtrochanteric fractures of the femur. Limited open reduction and additional fixation such as cable grip are recommended if it is difficult to obtain anatomical reduction by closed reduction. -
Citations
Citations to this article as recorded by- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Gyu Min Kong
Journal of the Korean Fracture Society.2019; 32(2): 107. CrossRef
- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
- 529 View
- 2 Download
- 1 Crossref

Case Reports
- Insufficiency Fracture of Proximal Femur Shaft without Bisphosphonate Therapy: Report of Three Cases
- Suk Kyu Choo, Dae Yeon Jo, Hyoung Keun Oh
- J Korean Fract Soc 2013;26(3):217-220. Published online July 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.3.217
-
 Abstract
Abstract
 PDF
PDF - There is a growing interest in the factors related to insufficiency fractures. We are going to report three insufficiency fracture cases which are considered to be caused by osteoporosis, rheumatoid arthritis, steroid use and femoral shaft bowing among the patients not taking bisphosphonate. All cases are caused by low energy trauma and among these cases, one patient is being presented with a prodromal symptom and another patient complains of both prodromal symptoms and bilateral lesions.
- 226 View
- 0 Download

- Excessive Sliding of the Helical Blade and the Femoral Neck Fracture after Insertion of Proximal Femoral Nail Anti-Rotation for Type A2 Intertrochanteric Fractures - A Case Report -
- Bong Ju Park, Hong Man Cho, Ju Han Kim, Woo Jin Sin
- J Korean Fract Soc 2013;26(2):151-155. Published online April 30, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.2.151
-
 Abstract
Abstract
 PDF
PDF - Proximal femoral nail anti-rotation (PFNA) with a lag screw that is shaped like a spiral blade shape is an orthopedic implant to fix trochanteric fractures of the proximal femur. In addition the reason of the biomechanical advantages, PFNA widely been used recently. We report an 83-year-old man with excessive sliding of the helical blade and a femoral neck fracture after AO/OTA type A2 intertrochanteric fracture, which was fixed with a PFNA.
-
Citations
Citations to this article as recorded by- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture - A Case Report -
Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
Journal of the Korean Fracture Society.2021; 34(3): 112. CrossRef - Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
Journal of the Korean Fracture Society.2020; 33(4): 179. CrossRef - Failure of a Rotation Control Gamma 3 Lag Screw Used to Treat a Trochanteric Fracture
Kyungho Choi, Yongtae Kim, Shicheng Zhou, Jihyo Hwang
Hip & Pelvis.2018; 30(2): 129. CrossRef - Femoral neck fractures after internal fixation of trochanteric fractures with implants in situ in adults: A systematic review
Antonio Barquet, Peter V. Giannoudis, Andrés Gelink
Injury.2018; 49(12): 2121. CrossRef
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture - A Case Report -
- 484 View
- 2 Download
- 4 Crossref

Original Articles
- Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
- Jae Cheon Sim, Tae Ho Kim, Ki Do Hong, Sung Sik Ha, Jong Seong Lee
- J Korean Fract Soc 2013;26(1):37-43. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.37
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the result between the third generation gamma nail (gamma 3 nail) and proximal femoral nail anti-rotation (PFNA) in the treatment of unstable intertrochanteric fractures.
MATERIALS AND METHODS
Between March 2009 and June 2011, 47 consecutive patients with unstable intertrochanteric femoral fractures were treated with gamma 3 nail or PFNA. We reviewed 24 cases of gamma 3 nail and 23 cases of PFNA. Retrospectively, we evaluated the mean operation time, amount of bleeding, average union period, reduction status, change of neck shaft angle, Tip-apex distance, Cleveland index, sliding of lag screw and complication on set of telephone interview and outpatient. We also evaluated the postoperative capability of function and mobility, using 'Modified Koval index'.
RESULTS
There were no significant differences between the groups, which were treated with gamma 3 nail and PFNA. In addition, they did not show statistical difference. We experienced 2 cases of complication (gamma 3 nail 1 case, PFNA 1 case), which were cut-out of the femoral head.
CONCLUSION
The gamma 3 nail and PFNA were seen with good results in the treatment of unstable intertrochanteric fracture. -
Citations
Citations to this article as recorded by- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
Milan Mitkovic, Sasa Milenkovic, Ivan Micic, Predrag Stojiljkovic, Igor Kostic, Milorad Mitkovic
Vojnosanitetski pregled.2022; 79(2): 177. CrossRef - Does the Helical Blade Lead to Higher Rates of Fixation Failure as Compared to Lag Screw in the Cephalomedullary Nailing Treatment of Hip Fractures? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Han Soul Kim, Yong-Chan Kim, Dou Hyun Moon
Journal of Orthopaedic Trauma.2021; 35(8): 401. CrossRef - The Curative Effect Comparison Between Prolonged Third Generation of Gamma Nail and Prolonged Dynamic Hip Screw Internal Fixation in Treating Femoral Intertrochanteric Fracture and the Effect on Infection
Wenye He, Wei Zhang
Cell Biochemistry and Biophysics.2015; 71(2): 695. CrossRef - Accuracy of the Lesser Trochanter for Guiding Lag Screw Insertion in Hip Fracture Management
Jianlin Xiao, Zhongli Gao, Yanguo Qin, Xuezhou Li, Ao Wang, Lanyu Zhu, Jincheng Wang
Orthopedics.2014;[Epub] CrossRef
- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
- 947 View
- 3 Download
- 4 Crossref

- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- Youn Soo Hwang, Kwang Yeol Kim, Hyung Chun Kim, Su Han Ahn, Dong Eun Lee
- J Korean Fract Soc 2013;26(1):14-20. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.14
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the effectiveness of optimal treatment of proximal humeral fractures and humeral shaft fractures in elderly patients with osteoporosis using the Polarus nail.
MATERIALS AND METHODS
Twenty-three patients with proximal humeral and humeral shaft fractures in elderly osteoporosis patients were treated using the Polarus intramedullary nail. Nine patients had proximal humeral fracture, 10 had humeral shaft fracture and 4 had the proximal humeral frac-ture extended diaphyseally. Radiological outcomes included the bone-union and the degree of re-sidual deformity. The residual deformities of the proximal humerus were assessed by the neck-shaft angle and the shaft angulation. Clinical outcome was assessed with the American Shoulder and Elbow Surgeons (ASES) score.
RESULTS
All cases had bony union and the mean union period was 16.5 weeks. The average neck/shaft alignment at the time of bone union was 135degrees and varus deformities of neck-shaft angle was not seen in all patients. Varus shaft angulation was seen in 5 patients. The mean ASES score after surgery was 86.7 points.
CONCLUSION
The Polarus intramedullary nail is effective for the treatment of proximal humeral and humeral shaft fractures in elderly patients with osteoporosis because it not only enables early postoperative mobilization, but also obtains bone-union without avascular necrosis and nonunion. -
Citations
Citations to this article as recorded by- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
Shankar Ramaprasad Kurpad
Indian Journal of Orthopaedics.2025; 59(8): 1053. CrossRef
- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
- 402 View
- 0 Download
- 1 Crossref

- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
- J Korean Fract Soc 2012;25(4):305-309. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.305
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Our study aimed to investigate the clinical and radiological results of humerus proximal or distal shaft fractures treated with minimally invasive plate osteosynthesis (MIPO) using a 3.5/5.0 metaphyseal locking plate.
MATERIALS AND METHODS
We reviewed the clinical and radiographic records of 17 patients with humeral proximal or distal shaft fractures who had undergone 3.5/5.0 metaphyseal locking plate osteosynthesis with a minimally invasive technique. We evaluated the results with respect to the anatomical reduction and union of the humerus shaft fracture through radiologic studies. We also evaluated the clinical results using the motion of shoulder and elbow functional outcome, American Shoulder and Elbow Surgeons (ASES) score, Mayo elbow performance score (MEPS), and postoperative complications.
RESULTS
Complete union was achieved in all cases. The mean union time was 14.2 weeks. According to the functional outcome rated by the ASES score and MEPS, 15 cases were considered excellent and 2 cases were good. There were no cases of surgically-related complications like metal failure, loss of anatomical reduction, or postoperative nerve injuries.
CONCLUSION
Using a 5.0 metaphyseal locking plate for humerus shaft fracture has the limitation that difficulties can arise in achieving sufficient screw fixation for small bony fragments. The 3.5/5.0 metaphyseal locking plate used in MIPO for humerus 1/3 proximal or distal shaft fractures was concluded to give good clinical and radiologic results. -
Citations
Citations to this article as recorded by- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
Journal of the Korean Fracture Society.2013; 26(1): 14. CrossRef
- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- 465 View
- 1 Download
- 1 Crossref

- Clinical Outcome of Surgical Treatment for Fracture of the Femoral Shaft with Ipsilateral Fracture of the Proximal Femur
- Hee Gon Park, Jae Sung Yoo
- J Korean Fract Soc 2011;24(4):307-312. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.307
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze diagnostic process and clinical data in cases of fracture of the femoral shaft with fracture of the proximal femur.
MATERIALS AND METHODS
We reviewed 24 cases of patient who undergone surgery for fracture of the femoral shaft with ipsilateral fracture of the proximal femur and more than 1 year of examination of follow up was available. Age, sex.location and classification of the fracture, the time of diagnosis and operation, the method of operation, the associated injuries, the time of bony union and complication were investigated, postoperative function was evaluated on Friedman and Wyman criteria.
RESULTS
Bony union showed significant difference in the displacement and comminution of fracture, postoperative function revealed significant difference according to the associated injuries. The 6 cases (25%) out of 24 cases are failed early diagnosis, 4 cases out of 6 cases was detected during operation and 2cases was found after surgery. 21 cases out of 24 cases of femoral shaft fractures showed union, 23 cases out of 24 cases of femoral neck fractures showed union. There were eleven good, eleven fair, and two poor functional result according to Friedman and Wyman criteria.
CONCLUSION
Precious clinical and radiologic examination is needed not to miss the diagnosis of proximal femur fractures in ipsilateral femoral shaft fractures with proximal femur fractures. Anatomical reduction and rigid fixation of proximal femur are important to reduce avascular necrosis of femoral head and nonunion of proximal femoral fractures.
- 223 View
- 2 Download

- Intramedullary Nailing for Complex Fractures of the Proximal and Midshaft of the Humerus
- Chul Hyun Cho, Gu Hee Jung, Kyo Wook Kim
- J Korean Fract Soc 2011;24(3):237-242. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.237
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results of antegrade interlocking intramedullary nailing for complex fractures of the proximal and midshaft of the humerus.
MATERIALS AND METHODS
We retrospectively analyzed the clinical and radiologic results in 11 cases, which were treated by antegrade interlocking intramedullary nail. We assessed clinical outcomes according to ASES scoring system and radiological result.
RESULTS
All cases had bony union and the mean union period was 14.7 weeks. Postoperative complications were 1 loss of fixation, 2 proximal protrusion of nail and 2 temporary shoulder pain. A case with loss of fixation was treated open reduction and refixation and had union at 14 weeks postoperatively. The mean ASES score was 85.9 and the clinical outcomes were 4 excellent, 5 good, 1 fair and 1 poor.
CONCLUSION
Intramedullary nailing for complex fractures of the proximal and midshaft of the humerus can offer a reliable treatment option.
- 230 View
- 0 Download

- Treatment of the Intertrochanteric Femoral Fracture with Proximal Femoral Nail: Nailing Using the Provisional K-wire Fixation
- Gu Hee Jung
- J Korean Fract Soc 2011;24(3):223-229. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.223
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the efficiency of provisional K-wire fixation in intertrochanteric fractures treated with proximal femoral nail (PFN).
MATERIALS AND METHODS
Twenty seven patients (by AO/OTA classification, A1 8 cases, A2 19 cases) were treated with PFN with percutaneous reduction and provisional K-wire fixation, and followed a mean 24.5 months. The adequacy of fracture reduction was assessed by Fogagnolo's classification and reestablishment of bone-to-bone contact with the medial anatomy. Functional results were evaluated by postoperative complications, Jensen's method and Harris hip score (HHS).
RESULTS
In all cases, the bone-to-bone contact with the medial anatomy was reestablished by percutaneous reduction and examination of Fogagnolo's classification showed a good reduction. The technical complications and error of starting point were not occurred. The mean HHS was 76.5 and means Jensen's grade was 2.1 grades. Complications included excessive sliding in 1 case and early cutting-out of screw in 1 case.
CONCLUSION
The provisional K-wire fixation in trochanteric fracture treated with PFN had an advantage in preventing technical complications because it facilitates a nail insertion in ideal position. -
Citations
Citations to this article as recorded by- Analysis of Low-Energy Trochanter Fracture Using the Multiplanar Computed Tomography Image: Application for Intramedullary Nail Fixation
Gu-Hee Jung, Sung-Keun Heo, Hyun-Je Seo
Journal of the Korean Fracture Society.2015; 28(3): 155. CrossRef - Morbidity and Mortality of the Elderly after Early Operation for Trochanteric Fractures
Se-Ang Jang, Young-Ho Cho, Young-Soo Byun, Ki-Hong Park, Hyun-Seong Yoo, Chul Jung
Journal of the Korean Fracture Society.2013; 26(3): 199. CrossRef
- Analysis of Low-Energy Trochanter Fracture Using the Multiplanar Computed Tomography Image: Application for Intramedullary Nail Fixation
- 525 View
- 1 Download
- 2 Crossref

- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
- Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
- J Korean Fract Soc 2011;24(3):217-222. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.217
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the results of intertrochanteric fractures treatment with proximal femoral nail antirotation (PFNA) without using fracture tables and thereby prevent complications.
MATERIALS AND METHODS
Forty cases of intertrochanteric fracture of 39 patients that were treated with PFNA without using fracture tables between January 2008 to December 2009 were analyzed. There were 13 males and 27 females. The mean age was 76 years old. Using AO classification, 6 cases were A1, 25 cases were A2 and 9 cases were A3. The operation was done without using fracture tables at supine position. Operation time, intraoperative bleeding were checked. For the result, Cleveland index, tip apex distance, fracture site sliding rate, change of femur neck and shaft angle were evaluated. Bone union time and complications were also estimated from the follow up radiograph. Statistics were analyzed using Independent T-test.
RESULTS
The mean operation time was 40 minutes (25 to 70 minutes) and mean intraoperative bleeding was 113 cc (40 to 250 cc). The Cleveland index was shown 94% of 5, 6, 8 and 9 zone, the tip apex distance was 12.96 mm (6 to 22 mm), the fracture sliding distance was 1.9 mm (0 to 6 mm), the change of femur neck and shaft angle was 2.5 degree (0~10 degree) and the average bone union time was 15 weeks (8 to 24 weeks). The complication include 2 cases of delayed union and 2 cases of varus deformities.
CONCLUSION
We have shortened the operation time by closed reduction methods without using the fracture tables, and the complication were minimized with using simple tools like a reduction forcep or bone hook at PFNA blade insertion. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
Journal of the Korean Fracture Society.2013; 26(4): 284. CrossRef
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- 508 View
- 1 Download
- 2 Crossref

Case Report
- Periprosthetic Fracture after Proximal Humeral Intramedullary Nail, Treated by Functional Bracing: A Case Report
- Jae Hyuk Shin, Ho Guen Chang, Young Woo Kim, Nam Kyou Rhee, Yong Bok Park, Yong Kuk Kim
- J Korean Fract Soc 2011;24(2):185-190. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.185
-
 Abstract
Abstract
 PDF
PDF - Periprosthetic fracture following a proximal humeral intramedullary (IM) nailing is rarely reported neither for its occurrence nor for its treatment. Proximal humeral IM nail (Acumed, LLC, Hillsboro, OR, USA) has been increasingly reported of its successful treatment outcomes, yet there is paucity of data describing its complications. Here we report a 26 year-old female patient, who sustained a proximal humerus fracture which was initially successfully treated by proximal humeral IM nail, and was complicated by a periprosthetic fracture distal to the nail tip at postoperative 4 months. Serial application of U-shaped coaptation splint, hanging cast, and functional bracing resulted in satisfactory clinical outcome. Periprosthetic fracture after proximal humerus IM nail can occur by a low energy injury, which need to reminded in treating young and sports-active patients.
-
Citations
Citations to this article as recorded by- Locking compression plate fixation of periprosthetic distant humeral fracture after intramedullary nail for humeral shaft fracture: A case report
Mei-Ren Zhang, Kui Zhao, Jiang-Long Guo, Hai-Yun Chen
Trauma Case Reports.2022; 37: 100565. CrossRef - Distal Humeral Fixation of an Intramedullary Nail Periprosthetic Fracture
Hiren M. Divecha, Hans A. J. Marynissen
Case Reports in Orthopedics.2013; 2013: 1. CrossRef
- Locking compression plate fixation of periprosthetic distant humeral fracture after intramedullary nail for humeral shaft fracture: A case report
- 476 View
- 3 Download
- 2 Crossref

Original Article
- Comparison of Results between Internal Plate Fixation and Hemiarthroplasty in Comminuted Proximal Humerus Fracture
- Doo Sup Kim, Dong Kyu Lee, Chang Ho Yi, Jang Hee Park, Jung Ho Rah
- J Korean Fract Soc 2011;24(2):144-150. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.144
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Authors compare clinical and radiological results of internal fixation group and hemiarthroplasty group for comminuted proximal humerus fracture to find out which the treatment method have to be chose for comminuted proximal humerus fractures.
MATERIALS AND METHODS
Patients who were treated from March 2005 to March 2007 and available for 2 years follow-up were targets of this study. The internal fixation group had 38 cases, and hemiarthroplasty group included 26 cases. The results were analyzed both clinically and radiologically.
RESULTS
On average, Bone union took 15.6 weeks in the internal fixation group. Constant score between the internal fixation and hemiarthroplasty groups were on average 75+/-6.5 points and 70+/-7.4 points (p=0.034). In 3-part fracture, Constant score between both groups were 78+/-5.4 points from the former and 71+/-2 points, respectively (p=0.028). In 4-part fracture group, Constant score were 72+/-8 points for the internal fixation group and 69+/-9.2 points for the hemiarthroplasty group (p=0.041).
CONCLUSION
Internal plate fixation can gain better outcome than hemiarthroplasty in 4-part fracture as well as 3-part fracture of proximal humerus by careful dissection for preservation of blood supply for humeral head and optimal reduction. -
Citations
Citations to this article as recorded by- Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis
Erik Hohmann, Natalie Keough, Vaida Glatt, Kevin Tetsworth
European Journal of Orthopaedic Surgery & Traumatology.2022; 33(6): 2215. CrossRef - Effectiveness and Safety of Interventions for Treating Adults with Displaced Proximal Humeral Fracture: A Network Meta-Analysis and Systematic Review
Long Chen, Fei Xing, Zhou Xiang, Ara Nazarian
PLOS ONE.2016; 11(11): e0166801. CrossRef - Meta-analysis comparing locking plate fixation with hemiarthroplasty for complex proximal humeral fractures
Jiezhi Dai, Yimin Chai, Chunyang Wang, Gen Wen
European Journal of Orthopaedic Surgery & Traumatology.2014; 24(3): 305. CrossRef
- Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis
- 628 View
- 2 Download
- 3 Crossref


 E-submission
E-submission KOTA
KOTA

 First
First Prev
Prev