Search
- Page Path
- HOME > Search
Original Articles
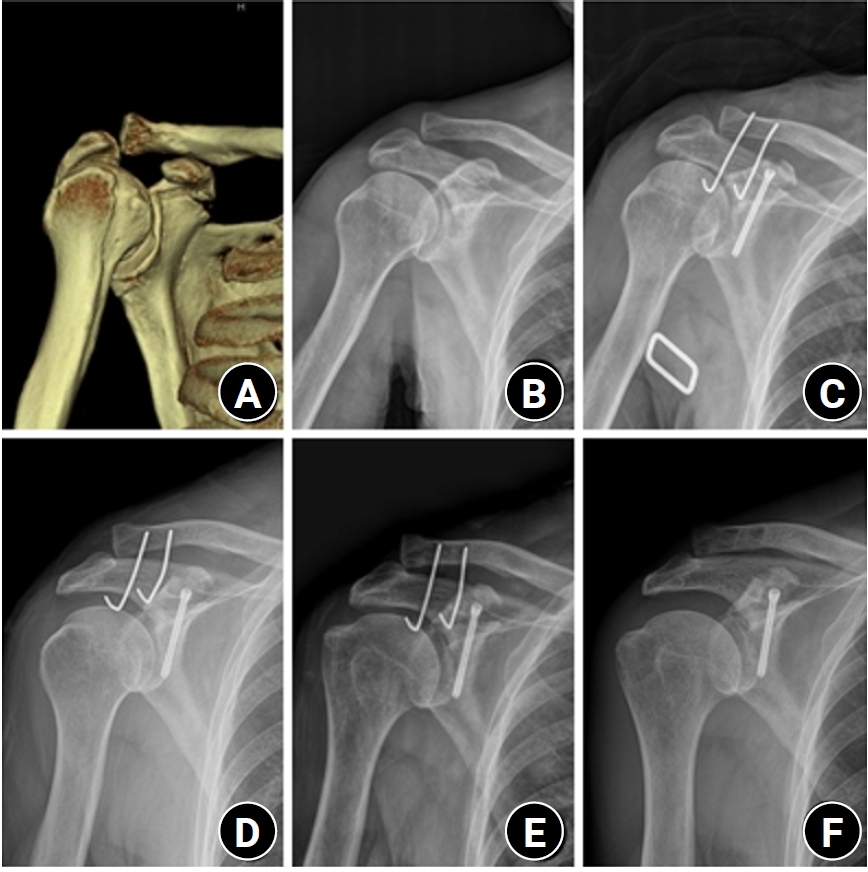
- Surgical outcomes of the coracoid process fracture associated with the acromioclavicular joint injury in Korea: a case series
- Dongju Shin, Sung Choi, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2026;39(1):54-61. Published online January 14, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00346
-
 Abstract
Abstract
 PDF
PDF - Background
Excluding technical reports and isolated case reports, there are no published studies evaluating coracoid process fixation with or without an acromioclavicular joint (ACJ) stabilization procedure for coracoid process fractures associated with ACJ injury. The purpose of this study was to assess the surgical outcomes of coracoid process fractures associated with ACJ injuries and to determine the usefulness of coracoid process fixation with or without an ACJ stabilization procedure.
Methods
From February 2006 to December 2015, patients with coracoid process fractures associated with ACJ injuries were enrolled. Radiological and clinical outcomes were analyzed in 12 patients who underwent coracoid process fixation with or without an ACJ stabilization procedure. A 3.5-mm cannulated screw with a washer or a 3.0-mm headless compression screw was used for coracoid process fixation, and either a clavicle hook plate or Kirschner (K)-wires were used for ACJ injuries when additional fixation was necessary.
Results
Bone union was achieved in 11 patients (91.7%), while one case was determined to be a nonunion at 6 months. Radiological union occurred at an average of 3 months (range, 1.5–4 months) in all patients except the nonunion case. At the final follow-up, the average clinical scores were a visual analogue scale (VAS) pain score of 1.5 (range, 0–4) and a UCLA score of 30.9 (range, 28–35). Clinical outcomes were satisfactory in all patients, including the patient with nonunion.
Conclusion
The clinical and radiological outcomes of treating coracoid process fractures associated with ACJ injuries using coracoid process fixation with or without ACJ stabilization were favorable. A cannulated screw with a washer and clavicle hook plate fixation may provide sufficient stability for both the coracoid process fracture and the ACJ injury when feasible. Level of evidence: IV.
- 182 View
- 6 Download

- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005
-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 2,047 View
- 59 Download

Case Report
- Axillary Artery Rupture after Shoulder Dislocation That Was Treated with a Self-Expanding Stent - A Case Report -
- HaengJin OHE, Daehyun Hwang, Inkeun Park, Minki Lee, Jun-Ku Lee
- J Korean Fract Soc 2020;33(4):217-221. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.217
-
 Abstract
Abstract
 PDF
PDF - raumatic shoulder dislocations are one of the most common major dislocations in the general population. Injury to major vessels is rarely reported as a complication of shoulder dislocations. This case report presents the traumatic dissection of the axillary artery after a simple shoulder dislocation that was managed successfully with the placement of a self-expanding stent. With the clinical manifestations of a brachial plexus injury and progressive vascular compromise in the affected arm, a major vascular injury was detected on an angiogram, and a self-expanding stent was deployed. Through immediate diagnosis and prompt intervention, serious complications, such as hypovolemic shock and even death, were averted, ultimately achieving a favorable patient outcome.
- 1,246 View
- 7 Download

Review Article
- Periprosthetic Fracture after Total Shoulder Arthroplasty
- Nam Su Cho, Myung Seo Kim, Jae Woo Yang, Jeung Hwan Seo, Dong Won Seo
- J Korean Fract Soc 2020;33(2):118-123. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.118
-
 Abstract
Abstract
 PDF
PDF - Periprosthetic humeral fractures in patients with total shoulder arthroplasty are rare and difficult to treat. With the significant increase in the number of older patients who have undergone total shoulder arthroplasty in recent years, an increase in the number of periprosthetic shoulder fractures can be estimated. The decisions of treatment have to be taken individually, depending on the stability of the prosthesis, fracture location, and bone quality. On the other hand, there are limited data for treatment guidance and outcomes. This paper reviews the risk factors, classification, treatment, and outcomes of periprosthetic humeral fractures.
- 815 View
- 16 Download

Case Report
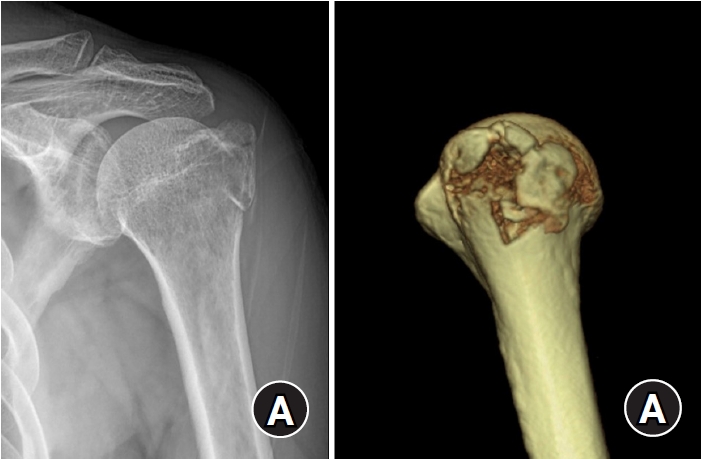
- Shoulder Quadruple Dislocation Fracture: Fracture of Glenoid Rim, Coracoid Process, Greater Tuberosity, Surgical Neck of Humerus Associated with Anterior Shoulder Dislocation: A Case Report
- Jae sung Yoo, Seong jun Kim, Seung gwan Park, Joong Bae Seo
- J Korean Fract Soc 2019;32(1):47-51. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.47
-
 Abstract
Abstract
 PDF
PDF - Shoulder joint dislocation has the most common incidence rate compare compared to other joints. It is reported that shoulder Shoulder dislocation couldmay be associated with glenoid rim, greater tuberosity of humerus and coracoid process fracture. There were have only been 2 cases of anterior shoulder dislocation simultaneously combined with simultaneous glenoid rim, coracoid process, and humerus greater tuberosity fracture worldwide and no report reports in Korea. We present a case of quadruple fracture (glenoid rim, coracoid process, greater tuberosity, surgical neck of humerus) associated with anterior shoulder dislocation and treated successfully by open reduction. In addition, with we provide the injury mechanism, diagnosis, treatment procedure and discussion.
- 677 View
- 2 Download

Original Article
- Clinical Features and Characteristics of Greater Tuberosity Fractures with or without Shoulder Dislocation
- Dong Wan Kim, Young Jae Lim, Ki Cheor Bae, Beom Soo Kim, Yong Ho Lee, Chul Hyun Cho
- J Korean Fract Soc 2018;31(4):139-144. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.139
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to compare the characteristics and clinical features of greater tuberosity fractures with or without a shoulder dislocation.
MATERIALS AND METHODS
A total of 108 cases of greater tuberosity fractures (56 cases with shoulder dislocation, 52 cases without shoulder dislocation) were reviewed retrospectively. Age, sex, side, injury mechanism, fracture displacement, fracture morphology, number of fracture fragments, main fragment size, treatment, and combined injuries were investigated.
RESULTS
The age, sex, side, injury mechanism, treatment, and combined injuries were similar in both groups (p>0.05). A statistically significant difference in fracture displacement, fracture morphology, number of fracture fragment, and main fragment size was observed between the two groups (p < 0.05).
CONCLUSION
In greater tuberosity fractures with a shoulder dislocation, the prevalence of fracture displacement was high and the depression type of fractures occurred frequently. In addition, the number and size of the fracture fragment increased. Therefore, an understanding of these fracture patterns will be helpful for deciding treatment and prognosis.
- 314 View
- 1 Download

Review Article
- Conservative Treatment of Mid-Clavicle Fractures
- Woong Kyo Jeong
- J Korean Fract Soc 2018;31(1):22-28. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.22
-
 Abstract
Abstract
 PDF
PDF - Clavicle fractures are very common injuries in adults and children and the majority of these fractures occur in the midshaft. Traditionally, mid-clavicle fractures have been treated with conservative methods and the clinical outcomes of this method are believed to be excellent. On the other hand, recent studies have shown that the clinical results of severe comminuted or markedly displaced fractures after conservative management were not as favorable as previously described. Despite these concerns, the conservative treatment of mid-clavicle fractures is still an efficient method, which can be applied to all patients as a primary care. This review focuses on the proper indication, technique, and limitations of conservative treatment of mid-clavicle fractures.
-
Citations
Citations to this article as recorded by- Two Patients Who Were Hospitalized for Clavicle Fracture Caused by a Traffic Accident and Improved with Korean Medicine Complex Treatment
Deok Kang, ByungSoo Kang, Hwe-Joon Jeong, Dong-Hoon Shin, Kyung-Moon Shin, Ji-Hoon O, Jae-Woo Yang
Journal of Korean Medicine Rehabilitation.2022; 32(3): 179. CrossRef
- Two Patients Who Were Hospitalized for Clavicle Fracture Caused by a Traffic Accident and Improved with Korean Medicine Complex Treatment
- 500 View
- 2 Download
- 1 Crossref

Case Reports
- Functional Recovery of the Shoulder after Correcting Malrotation of the Distal Humerus: A Case Report
- Hyunseong Yoo, Jaehui Han, Youngsoo Byun, Daegeun Jeong, Dongju Shin
- J Korean Fract Soc 2016;29(1):73-78. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.73
-
 Abstract
Abstract
 PDF
PDF - Although studies on malrotation of the humerus possibly leading to dysfunction of the shoulder have been reported, studies on its causes are inadequate. The authors encountered a patient complaining of malrotation accompanied by dysfunction of the shoulder which occurred during treatment of a distal humeral fracture. The patient recovered the shoulder function by only correcting malrotation of the humerus without direct treatment on the shoulder, and we report it herein with a review of the literature.
- 429 View
- 2 Download

- Iatrogenic Humeral Fracture during Reduction of Shoulder Dislocation: Two Cases Report
- Hyung Lae Cho, Hyoung Min Kim, Ki Bong Park, Tae Hyun Wang, Dong Hyun Lee
- J Korean Fract Soc 2016;29(1):50-54. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.50
-
 Abstract
Abstract
 PDF
PDF - Shoulder dislocation is the most common dislocation presenting to the emergency department. In old age, the attempt of closed reduction is made with caution in order to prevent iatrogenic fracture around the shoulder. We report two cases of iatrogenic fractures of humeral shaft and anatomical neck in female patients older than 70 years old, which occurred during the manual closed reduction. One patient was proved as first-time and the other was recurrent. In addition, the second case had a massive irreparable rotator cuff tear. Those patients were treated successfully with humeral nailing and reverse total shoulder arthroplasty, respectively.
- 412 View
- 4 Download

Original Articles
- The Result of Conservative Treatment of Proximal Humerus Fracture in Elderly Patients
- Seung Gil Baek, Chang Wug Oh, Young Soo Byun, Jong Keon Oh, Joon Woo Kim, Jong Pil Yoon, Hyun Joo Lee, Hyung Sub Kim
- J Korean Fract Soc 2013;26(4):292-298. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
With the increase in the old age population, proximal humerus fractures have been increasing recently. However, complications after operative treatment, such as fixation failure, are common because of osteoporosis. We treated proximal humerus fractures in patients with osteoporosis conservatively, and evaluated the radiographic and functional results by analyzing the factors affecting the results.
MATERIALS AND METHODS
Nineteen out of 30 cases for whom the clinical follow-up was over 1 year were included in this retrospective study. There were 17 females and 2 males, and the mean age was 73.2 years. The causes were slip from a short height (18 cases) and a minor car accident (1 case). We evaluated the union period, nonunion, malunion and the Constant score and analyzed several factors affecting the functional result, such as age, fracture pattern, and malunion.
RESULTS
Seventeen cases (89.5%) obtained union within 12.8 weeks on average. Neck-shaft angle was 125.3degrees on average, with seven cases of malunion. The Constant score was 84.1 on average, and there were excellent scores in 11 cases, good scores in 4 cases, and fair scores in 2 cases. Fracture pattern, neck-shaft angle, or malunion did not affect the functional outcome, and elderly patients showed poorer shoulder function.
CONCLUSION
Proximal humeral fractures with osteoporosis may achieve a high rate of bony union when treated with conservative methods. Despite the common occurrence of malunion, a satisfactory functional outcome may be expected.
- 774 View
- 6 Download

- Coracoclavicular Screw Fixation and Tension Band Wiring in Treatment of Distal Clavicle Fracture
- Dae Gyu Kwon, Tong Joo Lee, Kyung Ho Moon, Byoung Ki Shin, Min Su Woo
- J Korean Fract Soc 2013;26(1):1-7. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to analyze the effectiveness of coracoclavicular screw fixation with tension band wiring in the treatment of displaced distal clavicle fractures.
MATERIALS AND METHODS
From October 2006 to December 2010, 18 patients with Neer type 2 displaced distal clavicle fracture were surgically treated. Fixation was performed, using coracoclavicular screw with tension band wiring. Radiographic and clinical evaluation was performed and the University of California at Los Angeles (UCLA) shoulder rating scale was employed for the assessment of shoulder joint function.
RESULTS
Osseous union was achieved approximately 9.5 weeks (8-11 weeks) in all patients. After the union, the screw and wire were removed under local anesthesia. All patients returned to the normal shoulder range of motion. Loosening of the screw was seen in two patients and breakage was seen in one patient. However, we could not observe the delayed union and complications, such as infection and refracture. All but one patient showed excellent results according to the UCLA shoulder score at one year after the operation.
CONCLUSION
Coracoclavicular screw fixation with tension band wiring in the treatment of displaced distal clavicle fractures is a clinically useful technique with good result and less complication.
- 578 View
- 4 Download

Case Report
- Dislocation of the Shoulder with Ipsilateral Humeral Shaft Fracture: A Case Report
- Chul Hyun Cho, Kwang Yeung Jeong
- J Korean Fract Soc 2010;23(4):382-385. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.382
-
 Abstract
Abstract
 PDF
PDF - Dislocation of the shoulder with ipsilateral humeral shaft fracture is very rare, but serious injury that requires emergent care. There have been approximately 20 cases reported in the English literature, but it has never been reported in Korea. We report a case of dislocation of right shoulder with ipsilateral humeral shaft fracture which was successfully treated by closed reduction of the shoulder under general anesthesia and internal fixation with antegrade interlocking intramedullary nailing for the humeral shaft fracture.
-
Citations
Citations to this article as recorded by- Anterior Shoulder Dislocation With an Ipsilateral Humeral Shaft Fracture: A Case Report
Abdulmalik B Albaker , Ahmad Abdullah A Alsaleh, Mishari Malik Alshammari, Hatim Abdullah Akkasi, Hazzaa Abdullah Hazza Alharbi, Norah Ibrahim S Alqurmulah
Cureus.2023;[Epub] CrossRef
- Anterior Shoulder Dislocation With an Ipsilateral Humeral Shaft Fracture: A Case Report
- 699 View
- 1 Download
- 1 Crossref

Original Articles
- Result of Interlocking Intramedullary Nailing for Humeral Shaft Fracture Evaluation of Post-operative Shoulder Function
- Seung Rim Park, Tong Joo Lee, Ryuh Sub Kim, Kyoung Ho Moon, Dong Seok You
- J Korean Fract Soc 2007;20(2):166-171. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.166
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the post-operative functional reduction of the shoulder joint and the impacting factors to post-operative shoulder joint function in interlocking IM nailing treatment of humeral shaft fracture.
MATERIALS AND METHODS
From April 1999 to August 2004, 35 patients (35 cases) whom admitted to hospital for humeral shaft fracture and treated using interlocking intramedullary nail were followed up for more than 1 year. 1 year post-operative shoulder joint function were evaluated using American Shoulder Elbow Surgery Scale (ASES). Pre-operative shoulder joint pain, radiologically degenerative change and extent of nail protrusion were evaluated, and each factor was correlated with function of the shoulder joint.
RESULTS
33 cases out of 35 cases showed union and average union period was 12 weeks. Complications consisted of 2 cases of nonunion, 1 case of infection, 1 case of loosening of distal fixing screw, 1 case of radial nerve palsy and 1 case of axillary nerve palsy. Shoulder joint function 3 months after operation : mean ASES score 78.2, 12 months after operation : mean ASES score 89.6. Pre-operative shoulder joint pain and nail protrusion showed to be statistically related to shoulder joint function.
CONCLUSION
If the operation leaves no protrusion of intramedullary nail, it can be concluded to be relatively safe and effective. -
Citations
Citations to this article as recorded by- Comparison of the Result of the Intramedullary Nail Fixation and Plate Fixation in Humeral Shaft Fracture with Butterfly Fragments
Duk-Hwan Kho, Hyeung-June Kim, Byoung-Min Kim, Hyun-Ryong Hwang
The Korean Journal of Sports Medicine.2016; 34(2): 120. CrossRef - Plain Radiograph Analysis of the Distal Humerus Posterior Bowing That May Affect Interlocking Intramedullary Nailing for Humerus Shaft Fracture
Jaekwang Yum, Kyunghwan Boo, Minkyu Sung, Jiseok Jang
Journal of the Korean Orthopaedic Association.2015; 50(1): 31. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef - Surgical Treatment of Pathologic Humeral Fracture
Ho Jung Kang, Byoung Yoon Hwang, Jae Jeong Lee, Kyu Ho Shin, Soo Bong Hahn, Sung Jae Kim
Journal of the Korean Fracture Society.2010; 23(2): 187. CrossRef
- Comparison of the Result of the Intramedullary Nail Fixation and Plate Fixation in Humeral Shaft Fracture with Butterfly Fragments
- 699 View
- 0 Download
- 4 Crossref

- Result of Early Active Range of Motion Exercise after Bankart Repair of Traumatic Anterior Instability
- Haeng Kee Noh, Jong Woong Park, Jung Il Lee, Jung Ho Park
- J Korean Fract Soc 2007;20(1):53-57. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.53
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate prospectively the results of early active exercise after open Bankart repair of traumatic anterior shoulder instability.
MATERIALS AND METHODS
From January, 2001 to June, 2003, 26 patients who were followed up at least 1 year after open Bankart repair for traumatic anterior shoulder instability were evaluated. Average age was 23.9 years old (range, 19~43) with 24 males and 2 females. We evaluated them using the functional shoulder scores (modified Rowe score, ASES score), range of motion, VAS pain scale, patient's subjective satisfaction and return to unlimited daily living activity.
RESULTS
The shoulder functional scores increased significantly. At last follow up, the final range of motion were flexion in average 5° deficit in comparison to normal side, external rotation in average 10o deficit, and internal rotation in T9. The patient's subjective satisfaction was good in 2l patients (81%). Return to unlimited daily activity was possible in 23 patients (88.5%), and 19 patients (73%) rejoined to sports activity before injury. There were complications including anterior recurrent subluxation in 1 case, weakness of subscapularis muscle in 1 case.
CONCLUSION
In traumatic anterior shoulder instability, early active range of motion exercise after open Bankart repair does not decrease shoulder stability. Early exercise can be useful for returning to previous level of sports activity in young active patients.
- 565 View
- 3 Download

- Clinical and Functional Result after Internal Fixation of Severely Displaced Floating Shoulder
- Sang Hun Ko, Chang Hyuk Choe, Sung Do Cho, Jae Sung Seo, Jong Oh Kim, Jaedu Yu, Sang Jin Shin, In Ho Jeon, Kwang Hwan Jung, Jong Keun Woo, Ji Young Jeong, Gwon Jae No
- J Korean Fract Soc 2006;19(1):46-50. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.46
-
 Abstract
Abstract
- PURPOSE
To evaluate the follow-up result of 11 cases that were operated with internal fixation of scapular neck and internal fixation of clavicle or acromioclavicular dislocation for severely displaced floating shoulder which was high energy injury and unstable.
MATERIALS AND METHODS
We examined the scapular neck fracture with clavicle fracture or acromioclavicular joint dislocation by multidisciplinary research from August 1997 to July 2004. The scapular neck fractures were operated in the case of translational displacement of more than 25 mm and angular displacement of more than 45 degrees with 3.5 mm reconstruction plate fixation and internal fixation for clavicle fracture or acromioclavicular joint perpormed simultaneously. And we evaluated 11 cases that can be followed up for more than 9 months.
RESULTS
We achieved bony union in all cases. In ASES functional score, we got average 89.2 (75~95) points. In Rowe functional score, we got average 89.1 (75~100) points. In complication, there was external rotation weakness in 1 case.
CONCLUSION
In severely displaced floating shoulder due to high energy injury, we got good clinical and functional result after internal fixation for scapular neck and clavicle or acromioclavicular joint.
- 351 View
- 0 Download

- Operative Treatment of Floating Shoulder
- Ho Jung Kang, Gun Bo Park, Dong Joon Shim, Soo Bong Hahn, Eung Shick Kang
- J Korean Fract Soc 2004;17(1):38-42. Published online January 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.1.38
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Conservative treatment of displaced ipsilateral compound fractures of clavicle and scapula neck or gleonoid cavity, causing a floating shoulder, cannot expect satisfactory results in all of them. We reviewed 9 operative cases of floating shoulders and analyzed the results with review of literature.
MATERIALS AND METHODS
Nine patients with floating shoulders were operated from July 1996 to August 2000 were reviewed. Patient's age was in average 38.3 years old. Associated injuries were 4 cases of rib fractures and 1 case of humerus shaft fracture. Other injuries included 3 hemothorax, 2 pneumothorax, 1 brachial plexus injury, and 1 ulnar nerve injury. Operation for both clavicle and scapula fracture was done in 6 cases, and surgery was done for only clavicle in 3 cases. Internal fixation for clavicle was done with 3.5 mm AO reconstruction plate in 4 cases and Dynamic Compression Plate in 5 cases.
RESULTS
Clinical results by Hardegger method showed 7 cases of excellent, 1 case of good, and 1 case of poor. Complications include 2 cases of limitation of motion of shoulder joint and one case of residual pain.
CONCLUSION
Floating Shoulder is caused by high-energy trauma, therefore initial assessment of associated injuries should be done carefully. In evaluating the articular surface of the glenoid and positions of the fracture fragment, CT evaluation is very useful in planning the surgical treatment. Clinical results after surgery can give satisfactory results.
- 610 View
- 8 Download

- The Result of Modified Bankart Operation with Suture Anchor in Traumatic Recurrent Anterior Dislocation of Shoulder Joint
- Kwang Suk Lee, Jung Dae Seo, Kwang Jun Oh, Seung Joon Lee, Seung Yong Wang
- J Korean Soc Fract 2001;14(3):484-490. Published online July 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.3.484
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the clinical result of modified Bankart operation repairing the Bankart lesion with capsular shifting using suture anchor in traumatic recurrent anterior dislocation of shoulder joint MATERIALS AND METHODS: All of the cases were treated with modified Bankart operation. The inferior and superior capsular flaps were advanced to the anterior aspect of glenoid neck and fixed with three suture anchors in 30 degrees abduction and external rotation of shoulder joint. Especially the inferior 1/3 capsular flap was sutured over the superior 2/3 capsular flap. We used the grading system of Rowe and Zarins as measuring function, pain, stability, range of motion of shoulder joint.
RESULT
The clinical results were excellent in 80%, good in 20%. The mean loss of motion at follow up study was 2% of flexion and 7% of external rotation.
CONCLUSION
This operative technique is useful in repairing the Bankart lesion and gaining adequate capsular tension. And the using of suture anchor could save the operation time. -
Citations
Citations to this article as recorded by- Result of Early Active Range of Motion Exercise after Bankart Repair of Traumatic Anterior Instability
Haeng Kee Noh, Jong Woong Park, Jung Il Lee, Jung Ho Park
Journal of the Korean Fracture Society.2007; 20(1): 53. CrossRef
- Result of Early Active Range of Motion Exercise after Bankart Repair of Traumatic Anterior Instability
- 629 View
- 4 Download
- 1 Crossref

- Modified Phemister Operation for Acromioclavicular Dislocation
- Jin Yung Park, Gun Nam Kim, Byung Sam Min, Moon Jib Yoo
- J Korean Soc Fract 2001;14(3):456-462. Published online July 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.3.456
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical results after modified Phemister operation for complete dislocation of acromioclavicular joint.
MATERIALS AND METHODS
Thirty-seven cases of Fifty-three cases complete dislocation of acromioclavicular joint which were treated modified Phemister operation, follow up for at least one year, were evaluated. After operation, applied Kenny-Howard brace for six weeks and removed the inserted pins at ten to twelve weeks postoperatively. The ROM exercise was started at postoperative six weeks and meticulous ROM exercise was begun at pin removal. The clinical results were evaluated with range of movement, comparision of the coracoclavicular distance after surgery with that of follow up, and complications.
RESULTS
The range of motion were forward elevation 150 degree, external rotation 71 degree, external rotation at 90 degree abduction 77 degree, and internal rotation T8. The comparision of coracoclavicular distance after surgery(0,6mm) with that of follow up(1.0mm) showed no significant ligament laxity. The complication were subluxation in 2 cases, heterotrophic calcification in 3cases, broken K-wire in 2cases, pin site infection in 7cases and distal clavicle osteolysis in 3cases, which were healed at follow up radiographically.
CONCLUSION
To prevent of redislocation of acromioclavicular joint, we tried to insert the pin during relatively long period for sufficient healing of ruptured coracoclavicular ligament. Although immobilization period was relatively long period, clinical results were good.
- 454 View
- 1 Download

Case Report
- The combined qudriple lesion : fracture of acromion, distal end of clavicle, distal coracoid and glenoid rim associated with anterior shoulder dislocation: A Case Report
- Ryup Sub Kim, Suk Myun Ko, Kyu jung Cho, Hyeok Chae Jeong, Dong Hun Choi
- J Korean Soc Fract 2000;13(3):550-554. Published online July 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.3.550
-
 Abstract
Abstract
 PDF
PDF - A distal clavicle fracture, as a single fracture, has been reported frequently in the literature. However, combined anterior shoulder dislocations with fracture of the coracoid or acromion is very rare. Fracture of the coracoid or the acromion are even uncommon, represent 3-5% and 9-12% of scapular fractures respectively, which account for 1 perecnt of all fractures. Combined anterior shoulder dislocations with distal end clavicle or glenoid rim fractures are also rare. We observed the concurrent quadruple lesion: fracture of acromion, distal end of clavicle, distal coracoid and glenoid rim associated with anterior shoulder dislocation. To our knowledge, this combined injury has not been reported previously in the literature. Therefore, We presented the proposed mechanism of injury, course of treatment, and its clinical outcome with brief review of literature.
- 434 View
- 5 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


