Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(2); 2020 > Article
- Review Article Periprosthetic Fracture after Total Shoulder Arthroplasty
- Nam Su Cho, Myung Seo Kim, Jae Woo Yang, Jeung Hwan Seo, Dong Won Seo
-
Journal of Musculoskeletal Trauma 2020;33(2):118-123.
DOI: https://doi.org/10.12671/jkfs.2020.33.2.118
Published online: April 30, 2020
2Department of Orthopaedic Surgery, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
- 815 Views
- 16 Download
- 0 Crossref
- 0 Scopus
Abstract
Periprosthetic humeral fractures in patients with total shoulder arthroplasty are rare and difficult to treat. With the significant increase in the number of older patients who have undergone total shoulder arthroplasty in recent years, an increase in the number of periprosthetic shoulder fractures can be estimated. The decisions of treatment have to be taken individually, depending on the stability of the prosthesis, fracture location, and bone quality. On the other hand, there are limited data for treatment guidance and outcomes. This paper reviews the risk factors, classification, treatment, and outcomes of periprosthetic humeral fractures.
Published online Apr 28, 2020.
https://doi.org/10.12671/jkfs.2020.33.2.118
Periprosthetic Fracture after Total Shoulder Arthroplasty
 , M.D., Ph.D.,
Myung Seo Kim
, M.D., Ph.D.,
Myung Seo Kim , M.D.,*
Jae Woo Yang
, M.D.,*
Jae Woo Yang , M.D.,*
Jeung Hwan Seo
, M.D.,*
Jeung Hwan Seo , M.D.,*
and Dong Won Seo
, M.D.,*
and Dong Won Seo , M.D.*
, M.D.*
Abstract
Periprosthetic humeral fractures in patients with total shoulder arthroplasty are rare and difficult to treat. With the significant increase in the number of older patients who have undergone total shoulder arthroplasty in recent years, an increase in the number of periprosthetic shoulder fractures can be estimated. The decisions of treatment have to be taken individually, depending on the stability of the prosthesis, fracture location, and bone quality. On the other hand, there are limited data for treatment guidance and outcomes. This paper reviews the risk factors, classification, treatment, and outcomes of periprosthetic humeral fractures.
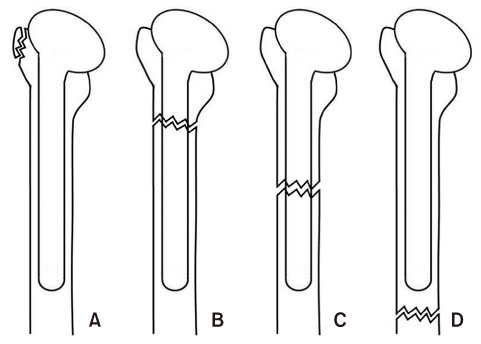
Fig. 1
Diagram showing the Wright and Cofield classification of a periprosthetic fracture of the humerus. Type A fractures are centered near the tip and extend proximally. Type B fractures are centered at the tip with variable extension distally. Type C fractures are located distal to the tip of the stem.
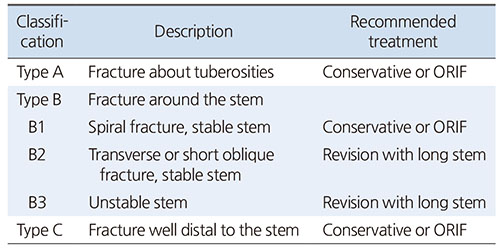
Fig. 2
Fracture location categories. (A) Region 1, tuberosity fracture. (B) Region 2, metaphyseal portion of the proximal humerus. (C) Region 3, proximal humeral diaphysis. (D) Region 4, mid- and distal humeral diaphysis.
Table 1
Periprosthetic Humeral Fracture
Financial support:None.
Conflict of interests:None.
References
-
Casp AJ, Montgomery SR Jr, Cancienne JM, Brockmeier SF, Werner BC. Osteoporosis and implant-related complications after anatomic and reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2019 [doi: 10.5435/JAAOS-D-18-00537][epub].
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

