Search
- Page Path
- HOME > Search
Original Article
- Hook plate fixation for volar plate avulsion fractures of the middle phalanges in Korea: a case series
- Kang-San Lee, Sang-Woo Son, Hee-June Kim, Hyun-Joo Lee, Dong Hee Kim
- J Musculoskelet Trauma 2026;39(1):48-53. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00339

-
 Abstract
Abstract
 PDF
PDF - Background
Volar plate avulsion fractures in phalanges are relatively common injuries. While surgical treatment can help reduce limitations in motion after injury, the small size of the fracture fragment can make the procedure challenging. In this study, we used hook plate fixation as a surgical technique for treating volar avulsion fractures in phalanges and evaluated its radiological and clinical outcomes.
Methods
The medical records of eight patients (nine digits) with volar plate avulsion fractures of the middle phalanx were retrospectively reviewed. All fractures were treated with a 1.5-mm hook plate after open reduction. Radiologic evaluations were performed using simple radiographs, and clinical outcomes were assessed through range of motion, instability, and pain.
Results
The mean follow-up period was 4.89 months (range, 1–9 months). All nine digits achieved bone union at the final follow-up. The mean union time was 2.2 months (range, 1–4 months). In all patients, the range of motion in the proximal interphalangeal joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. All patients demonstrated no joint instability and no residual pain.
Conclusion
Using a hook plate for volar plate avulsion fractures presents a promising alternative to existing fixation methods. Its biomechanical advantages and ease of fabrication make it a valuable tool in hand surgery. Level of evidence: IV.
- 191 View
- 8 Download

Review Articles
- Current concepts in the management of phalangeal fractures in the hand
- Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):109-123. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00136
-
 Abstract
Abstract
 PDF
PDF - This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra- articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
- 17,306 View
- 378 Download

- Avulsion Fractures of around the Hand
- Dong Whan Kim, Jung Il Lee
- J Korean Fract Soc 2024;37(3):158-168. Published online July 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.3.158
-
 Abstract
Abstract
 PDF
PDF - An avulsion fracture occurs when soft tissues, including the tendons and ligaments, are forcibly detached from the main bone by an external force. The hand contains numerous anatomical structures, such as ligaments, tendons, and volar plates, which are essential for maintaining multidirectional motion and joint stability. Excessive force applied in a specific direction can damage these structures, leading to avulsion fractures around the joint. These fractures can result in severe complications if left untreated or improperly managed, including joint deformity, contracture, nonunion or malunion of the fracture, secondary osteoarthritis, and limited range of motion. Therefore, an accurate examination, diagnosis, and appropriate treatment are crucial for preventing these adverse outcomes. An avulsion fracture can be managed conservatively when the avulsed fragment does not compromise joint stability or motion. Nevertheless, surgical intervention is required to stabilize the fragment if it affects joint stability or motion. The use of internal fixation has become more prevalent because of recent advances in small implants for fixation.
- 1,077 View
- 18 Download

- Hand Fractures
- Seokwon Yang, Jong Pil Kim
- J Korean Fract Soc 2018;31(2):61-70. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.61
-
 Abstract
Abstract
 PDF
PDF - Hand fractures are the second most common fracture in the upper extremities after the distal radius, and patients with these injuries may be experienced in hand surgery clinics. On the other hand, during the treatment of hand fractures, complications can occur due to complex functions of the hand and small-sized injuries to the bone and soft tissues. This review focused on the principles of management of these fractures, including injury mechanism, evaluations and recent treatment options. Minimally invasive surgery in various types of hand fractures, including the phalanx and metacarpal bone, is preferred because early mobilization after surgery has been emphasized to reduce complications, such as stiffness.
-
Citations
Citations to this article as recorded by- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
Dae-Geun Kim, Hyo Jun Park
Archives of Hand and Microsurgery.2023; 28(4): 239. CrossRef
- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
- 601 View
- 2 Download
- 1 Crossref

- Current Concepts of Fractures and Dislocation of the Hand
- Yong Cheol Yoon, Jong Ryoon Baek
- J Korean Fract Soc 2016;29(2):143-159. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.143
-
 Abstract
Abstract
 PDF
PDF - Fractures and dislocation of the hand is a body injury involving complex structures and multiple functions, which frequently occur as they represent 10%-30% of all fractures. Such fractures and dislocation of the hand should be treated in the context of stability and flexibility; and tailored treatment is required in order to achieve the most optimal functional performance in each patient since deformation may occur if not treated, stiffness may occur with unnecessarily excessive treatment, and both deformation and stiffness may occur coincidently with inappropriate treatment. Stable injuries can be fixed with splintage whereas surgery is actively considered for unstable injuries. In addition, surgeons should keep in mind that as the surgical intervention is done aggressively, aggressive rehabilitation must be followed in correspondence with the surgical intervention. Successful outcome requires effort to prevent any potential complication including nerve hypersensitivity and infection. Finally, it is also important that the patient to know that swelling, stiffness, and pain may last for a long period of time until the recovery of fractures and dislocation of the hand.
-
Citations
Citations to this article as recorded by- Current concepts in the management of phalangeal fractures in the hand
Hyun Tak Kang, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(3): 109. CrossRef - Current Concepts in Management of Phalangeal Fractures
Yohan Lee, Sunghun Park, Jun-Ku Lee
Journal of the Korean Fracture Society.2022; 35(4): 169. CrossRef
- Current concepts in the management of phalangeal fractures in the hand
- 1,190 View
- 20 Download
- 2 Crossref

Case Report
- Salvage Therapy from Traumatic Ischemic Finger Necrosis via Prostaglandin E1 Assisted Conservative Treatment: A Case Report
- Jae Hyuk Shin, Ho Guen Chang, Cheol Jung Yang, Jungtae Ahn
- J Korean Fract Soc 2015;28(4):245-249. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.245
-
 Abstract
Abstract
 PDF
PDF - Prostaglandin E1 (PGE-1) is a potent vasodilator, which also inhibits platelet aggregation, affects the blood flow viscosity, and fibrinolysis. The compound also excerts anti-inflammatory effects by inhibiting the monocyte and neutrophil function. PGE-1 has been widely administered following microvascular flap surgery, along with perioperative antithrombotic agents such as low molecular weight heparin or aspirin, showing excellent results. We report a case showing successful salvage recovery from post-traumatic ischemic necrosis of the finger via PGE-1 assisted conservative treatment.
- 681 View
- 2 Download

Original Article
- Percutaneous Retrograde Intramedullary Pin Fixation for Isolated Metacarpal Shaft Fracture of the Little Finger
- Soo Hong Han, Hyung Ku Yoon, Dong Eun Shin, Seung Chul Han, Young Woong Kim
- J Korean Fract Soc 2010;23(4):367-372. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.367
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the anatomic and functional outcome of retrograde intramedullary single wire fixation for metacarpal shaft fractures of the little finger.
MATERIALS AND METHODS
hirty one consecutive patients with closed metacarpal shaft fractures of the little finger who have been treated with retrograde intramedullary single wire fixation were evaluated. Fracture union and angulation were analyzed radiologically, and clinical evaluations were performed including range of motion, DASH score and complications.
RESULTS
Fracture union was achieved in all cases and callus formation was obvious at postoperative 41 days. Average angulation of fracture site was 3degrees in the coronal plane and 1.2degrees in the sagittal plane at the last follow up and no measurable metacarpal shortening was observed. Mean TAM was 253degrees and DASH score was 2.6. There were two cases of pin migration as intermediate complications.
CONCLUSION
Closed reduction with subsequent percutaneous retrograde K-wire fixation produced good radiological and functional results. We recommend this minimally invasive technique which provides adequate fixation of displaced little finger metacarpal shaft fractures with good functional results and low morbidity. -
Citations
Citations to this article as recorded by- The Treatment Outcomes of the Metacarpal Shaft and Neck Comminuted Fractures Using Modified Percutaneous Retrograde Intramedullary Kirschner Wire Fixation
Seok Woo Hong, Young Ho Lee, Min Bom Kim, Goo Hyun Baek
Archives of Hand and Microsurgery.2018; 23(3): 175. CrossRef
- The Treatment Outcomes of the Metacarpal Shaft and Neck Comminuted Fractures Using Modified Percutaneous Retrograde Intramedullary Kirschner Wire Fixation
- 917 View
- 4 Download
- 1 Crossref

Case Reports
- Osteochondral Autograft Using Head of Proximal Phalanx of Toe for Partial Osteochondral Defect of Proximal Interphalangeal Joint: A Case Report
- Tong Joo Lee, Kyung Ho Moon, Yoon Sang Jeon, Do Seung Kwon
- J Korean Fract Soc 2010;23(3):321-325. Published online July 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.3.321
-
 Abstract
Abstract
 PDF
PDF - Osteochondral injury due to the trauma of the hand is relatively common. If the size of the osteochondral fracture fragment is large, open reduction and internal fixation are often feasible in treating these problems. However, arthroplasty using osteochondral graft is more preferred when the particle is small and articular surface is comminuted or fully defected. There are many reports of osteochondral graft using the costal osteochondral graft but the osteochondral graft using the interphalangeal joint of the toe is rarely reported. Thoroughly reviewed with relevant articles, this report presents a case of a 33 year old male who was successfully treated with osteochondral autograft using the proximal interphalangeal joint of the toe due to the traumatic osteochondral defect in the head of the second proximal phalanx.
- 393 View
- 3 Download

- Simultaneous Dorsal Dislocation of Interphalangeal Joints in the Same Finger: Two Case Report
- Hyun Seok Song, Suk Ku Han, Sung Jin Park, Won Sik Nam, Hyuk Jae Yang, Nam Yong Choi
- J Korean Fract Soc 2006;19(3):388-391. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.388
-
 Abstract
Abstract
- We treated 2 cases of simultaneous dorsal dislocation of interphalangeal joints in the 5th finger. One case was injured by herperextension during basketball, and treated by open reduction and K-wire fixation. Another case was injured by industrial accident, and treated by splint for 1 week.
-
Citations
Citations to this article as recorded by- Double Dislocation of Interphalangeal Joints in a Single Digit - A Case Report -
Jai Hyung Park, Jeong Hyun Yoo, Joo Hak Kim, In Hyeok Lee
Journal of the Korean Society for Surgery of the Hand.2012; 17(4): 196. CrossRef
- Double Dislocation of Interphalangeal Joints in a Single Digit - A Case Report -
- 564 View
- 0 Download
- 1 Crossref

Original Articles
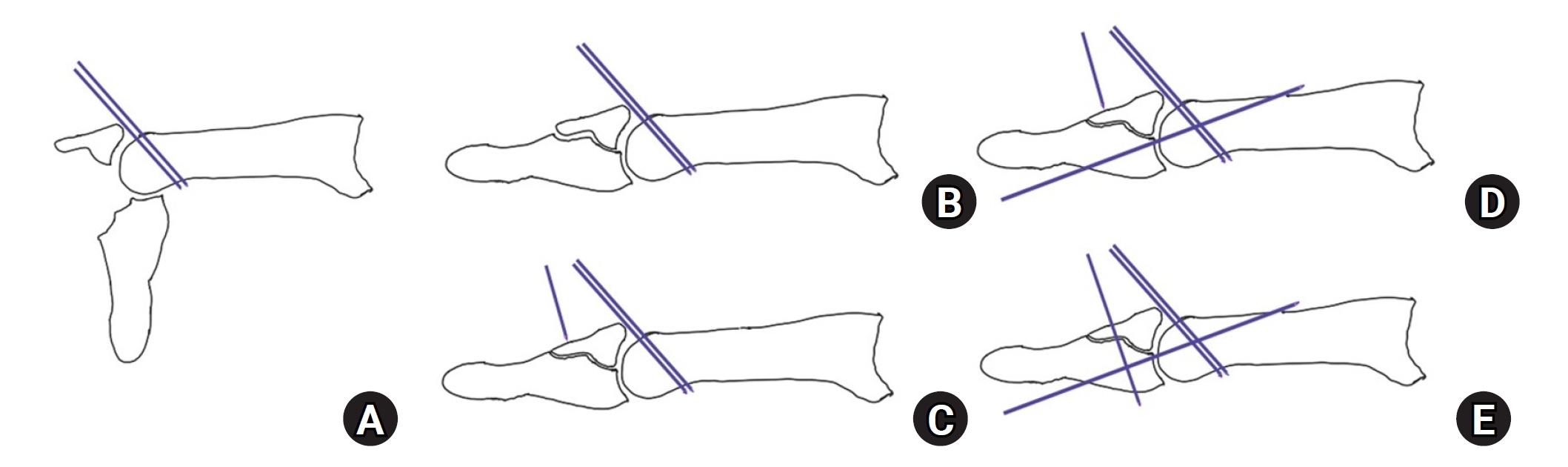
- The Result of the Modified Extension Block Technique in Bony Mallet Finger
- Seung Rim Yi, Sung Ho Hahn, Bo Kyu Yang, Yang Joon Ahn, Jae Hoo Yoo, Yong Beom Yeo, Sung Woo Bin
- J Korean Fract Soc 2006;19(2):236-240. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.236
-
 Abstract
Abstract
- PURPOSE
To evaluate the treatment outcomes of the modified extension block technique for bony mallet finger.
MATERIALS AND METHODS
This study included 16 patients who had been treated with the modified extension block technique for bony mallet finger from December 2002 to January 2004. The average duration of follow up was 13 (12~17) months. The indication of operation was the presence of a large bony fragment invading more than 1/3 of the articular surface or the palmar subluxation in the distal interphalangeal joint.
RESULTS
The average extension lag was 2.3 degrees, and the range of motion of the distal interphalangeal joint was 68.8 degrees. Radiograph showed bony union state in all cases. By the Crawford's evaluation criteria, 12 cases (75%) was excellent or good. Postoperative complications occurred in 3 cases, which were reduction loss within postoperative 2 weeks in 2 cases and mild pain with motion in 1 case.
CONCLUSION
The modified extension block technique is a easy and simple method. It shows a good result without complications from skin incision. So, it seems a useful method for bony mallet finger. -
Citations
Citations to this article as recorded by- Percutaneous Kirschner Wire Fixation of Acute Mallet Fractures Percutaneousely Reduced by Towel Clip
Chung Soo Han, Duke Whan Chung, Bi O Jeong, Hyun Chul Park, Jin Young Kim, Cheol Hee Park, Jin Sung Park
Journal of the Korean Fracture Society.2009; 22(4): 283. CrossRef
- Percutaneous Kirschner Wire Fixation of Acute Mallet Fractures Percutaneousely Reduced by Towel Clip
- 615 View
- 0 Download
- 1 Crossref

- Treatment of Bony Mallet Finger: Closed Reduction Using Extension Block K-wire
- Jae Yeol Choi, Hwa Jae Jung, Ho Jin Lee, Kyung Mo Son, Young Hun Kim
- J Korean Fract Soc 2004;17(4):362-367. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.362
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To review the result of bony mallet finger treated with a closed reduction using extension block K-wire MATERIALS AND METHODS: Between January 2001 and November 2002, among the patients with bony mallet finger underwent closed reduction using extension block K-wire, we retrospectively reviewed 14 patients with 14 fractures who had a minimum follow-up of 12 months.
RESULTS
There were 10 men and 4 women, with an average follow-up for all cases 15.7 months (range, 12 months~18 months). According to Crawford's evaluation criteria, we obtained 7 excellent, 5 good, 2 fair. We obtained bony union in all patients, with no remained pain. The average ROM was 67 degrees at postoperative 12 months. Postoperative complications occurred in two cases, which were nail deformity and mild osteoarthritis at the distal interphalangeal joint. There was no pin site infection.
CONCLUSION
This technique is not only easier but also less invasive than other techniques for reduction of mallet finger. Also, it shows excellent result with lower complication rate. So, it seems a reliable treatment for bony mallet finger. -
Citations
Citations to this article as recorded by- Osteoarthritis after Extension Block Technique for the Bony Mallet Finger
Sung Hoon Koh, Jung Hyun Park, Jin Soo Kim, Si Young Roh, Kyung Jin Lee, Dong Chul Lee
Archives of Hand and Microsurgery.2021; 26(4): 238. CrossRef - Comparison of Surgical Outcomes of Percutaneous K-Wire Fixation in Bony Mallet Fingers with Use of Towel Clip versus 18-Gauge Needle
Ho-Seung Jeon, Chan-Sam Moon, Seo-Goo Kang, Kyeong-Seop Song, Uk-Hyun Choi
Journal of the Korean Society for Surgery of the Hand.2013; 18(1): 1. CrossRef - Percutaneous Kirschner Wire Fixation of Acute Mallet Fractures Percutaneousely Reduced by Towel Clip
Chung Soo Han, Duke Whan Chung, Bi O Jeong, Hyun Chul Park, Jin Young Kim, Cheol Hee Park, Jin Sung Park
Journal of the Korean Fracture Society.2009; 22(4): 283. CrossRef
- Osteoarthritis after Extension Block Technique for the Bony Mallet Finger
- 628 View
- 2 Download
- 3 Crossref

- A Comparision of conservative and Operative Treatmene in the Bony Mallet Finger
- Ik Su Choi, Su In Roh, Hong Ju Ha, Jin Goo Kang, Dae Yeon Kim
- J Korean Soc Fract 1999;12(4):1021-1026. Published online October 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.4.1021
-
 Abstract
Abstract
 PDF
PDF - Mallet finger is a commom deformity caused by disruption of the extensor mechnism at the dorsal base of the distal phalanx. Patients can by managed by either conservative or operative treatment depending on some factors, such as the fracture type and interval from injury to medical treatment. However, whether to perform conservative or operative treatment is in debate. We conducted this study to compare the results of conservative and operative treatment of mallet finger caused by intra-articular fracture of the distal phalanx, with not mere than one third of the articular surface of the distal phalanx involved. From March 1994 to April 1999, we experienced 26 cases of bony mallet fingers. Following are the results. 1. The result by Kanies scale was satisfactory in 9 cases of 12 in conservative treatment(75%), and 10 cases of 14 in operative treatment(71%)(P>0.05). 2. The result was satisfactory in 8 cases of 10 in patients who were treated within 2 weeks(80%), and 4 cases of 7 in those treated after 4 weeks(57%)(P<0.05). 3. Conservative treatment was more cost effective, easier to perform compared to operative treatment. Thus, we suggest conservative treatment as the better treatment method for bony mallet finger with ont more than one third of the articular surface of the distal phalanx involved.
-
Citations
Citations to this article as recorded by- Extension pin block technique versus extension orthosis for acute bony mallet finger; a retrospective comparison
Gurkan Gumussuyu, Mehmet Melih Asoglu, Olcay Guler, Hasan May, Adil Turan, Ozkan Kose
Orthopaedics & Traumatology: Surgery & Research.2021; 107(5): 102764. CrossRef
- Extension pin block technique versus extension orthosis for acute bony mallet finger; a retrospective comparison
- 566 View
- 1 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


