Search
- Page Path
- HOME > Search
Original Articles
- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
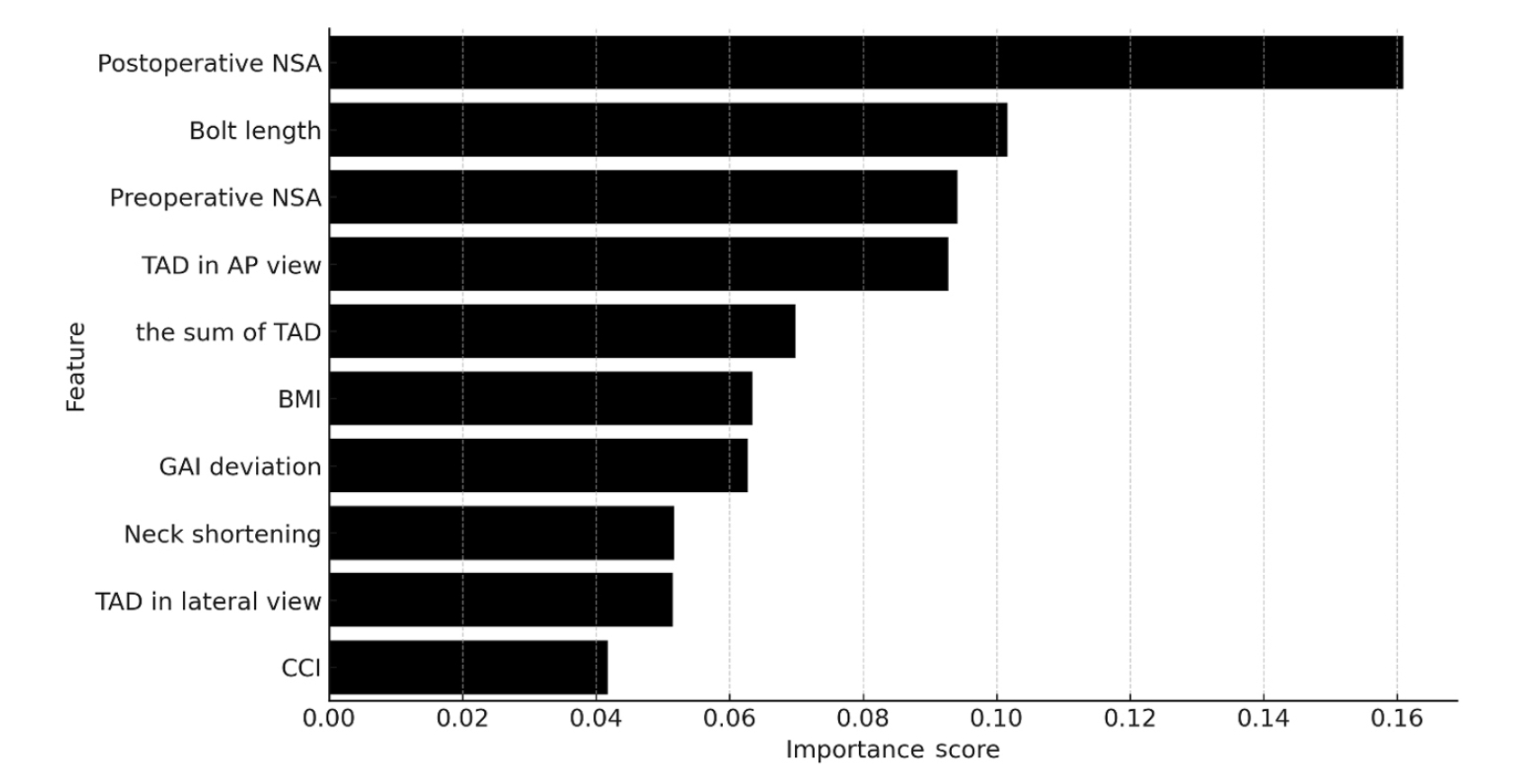
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III. -
Citations
Citations to this article as recorded by- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
Seonghyun Kang, Wonseok Choi, Jeong Seok Choi, Eic Ju Lim, SungJin Ahn, Jong-Keon Oh, William T. Kent, Whee Sung Son, Jae-Woo Cho
Journal of Orthopaedic Surgery.2026;[Epub] CrossRef
- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
- 1,229 View
- 43 Download
- 1 Crossref

- The Role of Beta-Tricalcium Phosphate Graft in the Dynamic Hip Screw Fixation of Unstable Intertrochanter Fracture
- Chul Ho Kim, Ji Wan Kim, Eic Ju Lim, Jae Suk Chang
- J Korean Fract Soc 2016;29(4):250-257. Published online October 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.4.250
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to introduce our method of stabilizing unstable intertrochanteric fractures by using the dynamic hip screw (DHS) with a beta-tricalcium phosphate (β-TCP) graft and to compare the outcomes of this procedure with those of the conventional DHS without β-TCP.
MATERIALS AND METHODS
Patients who underwent surgery by using DHS between March 2002 and January 2016 were retrospectively reviewed for analysis of the outcomes. The inclusion criteria were: 1) age of 60 years and older; 2) low-energy fracture resulting from a fall from no greater than the standing height; 3) multifragmentary pertrochanteric fracture (AO classification 31-A2.2, 2.3); and 4) follow-up of over 3 months. We compared 29 patients (29 hips) who underwent surgery, using DHS without β-TCP, with 29 age-sex matched patients (29 hips) who underwent surgery using DHS with grafted β-TCP granules to empty the trochanter area after reaming. We investigated the fracture union rate, union time, and length of lag screw sliding.
RESULTS
Bone union was achieved in all cases. The mean union time was 7.0 weeks in the β-TCP group and 8 .8 weeks in the non-β-TCP group. The length of lag screw sliding was 3.6 mm in the β-TCP group and 5 .5 mm in the non-β-TCP group. There were no implant failure cases in both groups.
CONCLUSION
The β-TCP graft for reinforcement DHS acquired satisfactory clinical outcomes for treating unstable intertrochanteric fractures.
- 437 View
- 3 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev