-
Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
-
Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
-
J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00157
-
-
 Abstract Abstract
 PDF PDF
- Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
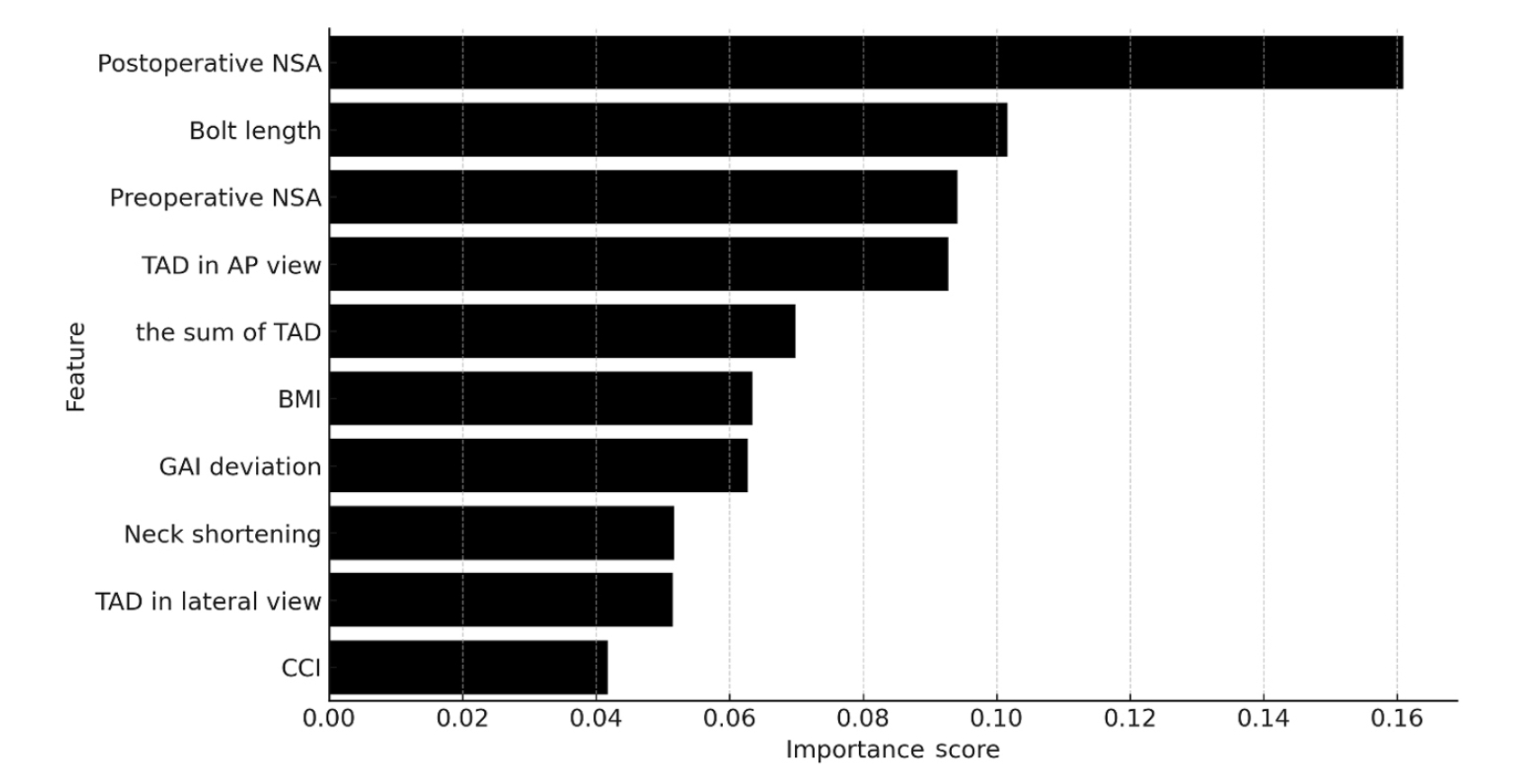
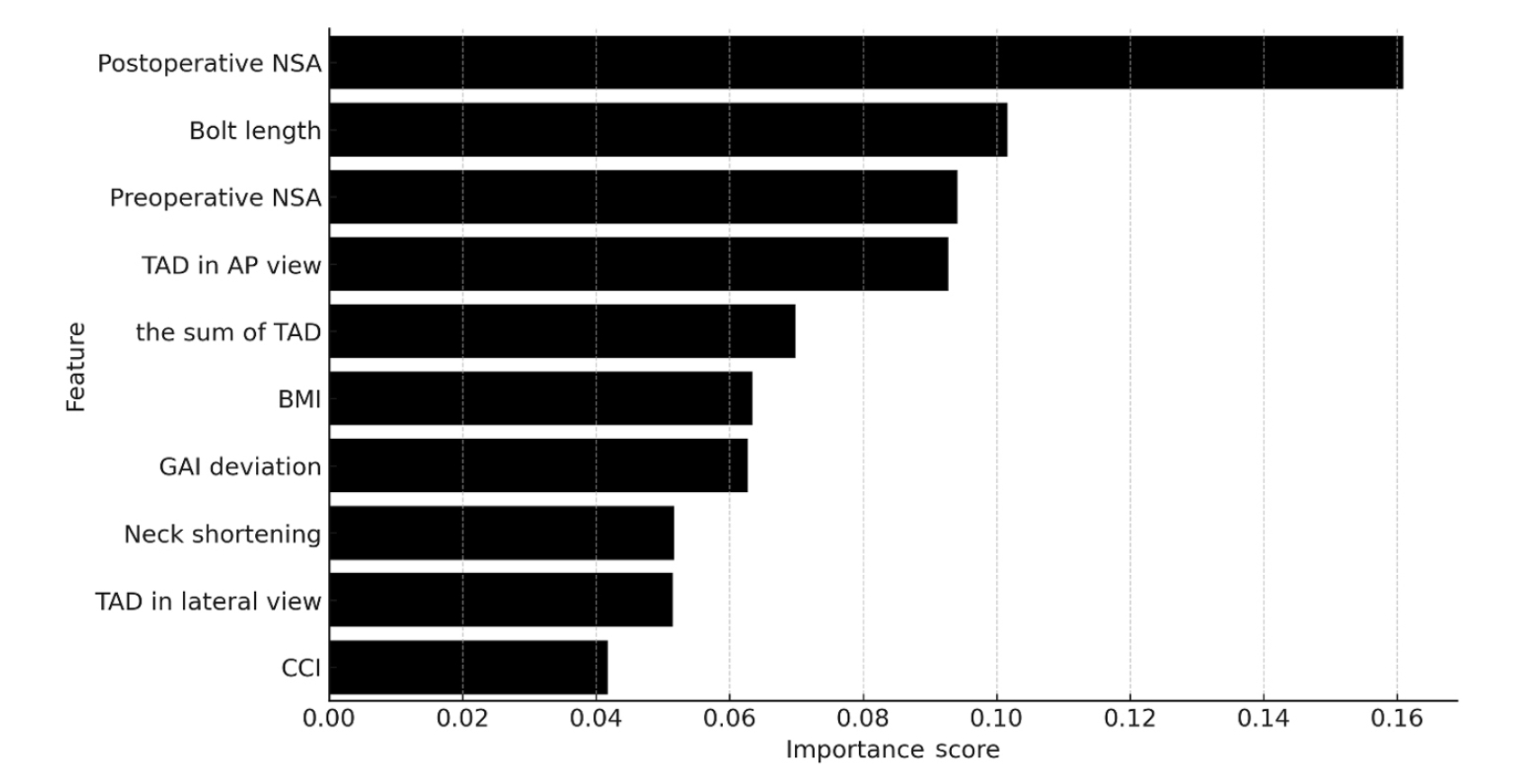
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery.
Level of Evidence: III.
-
Femoral Head Fracture with Hip Dislocation Treated by Autologous Osteochondral Transfer (Mosaicplasty) - A Case Report -
-
Eui-Sung Choi, Hyun-Chul Shon, Ho-Seung Jeong, Jae-Young Yang, Seok-Hyun Hong, Byung-Hyun Ahn
-
J Korean Fract Soc 2020;33(2):96-100. Published online April 30, 2020
-
DOI: https://doi.org/10.12671/jkfs.2020.33.2.96
-
-
 Abstract Abstract
 PDF PDF
- Femoral head fractures combined with hip dislocation are very rare injuries. In most cases, they result from high-energy trauma to the hip or lower extremity during traffic accidents. Various therapy options have been suggested to treat these injuries. Especially, different joint-preserving surgical options have been described for the treatment of traumatic osteochondral injury of the femoral head in young, active patients. In this report, we present a case that a traumatic osteochondral lesion to the femoral head after hip dislocation was treated with osteochondral autografts (OATS) from the non-weight-bearing area of the ipsilateral inferior femoral head through a surgical hip dislocation. After 1 year, the clinical and radiological outcome was satisfactory with no evidence of posttraumatic osteoarthritis and no pain of patients.
-
Citations
Citations to this article as recorded by  - Femoral head fracture with large crushed defect in weight-bearing area treated with autologous osteochondral transplantation (repositionplasty): A case report
Hyun-Chul Shon, Eic-Ju Lim, Jae-Young Yang, Seung-Jun Jeon
Medicine.2022; 101(52): e32569. CrossRef
-
313
View
-
0
Download
-
1
Crossref
|