-
Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
-
Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
-
J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00157
-
-
 Abstract Abstract
 PDF PDF
- Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
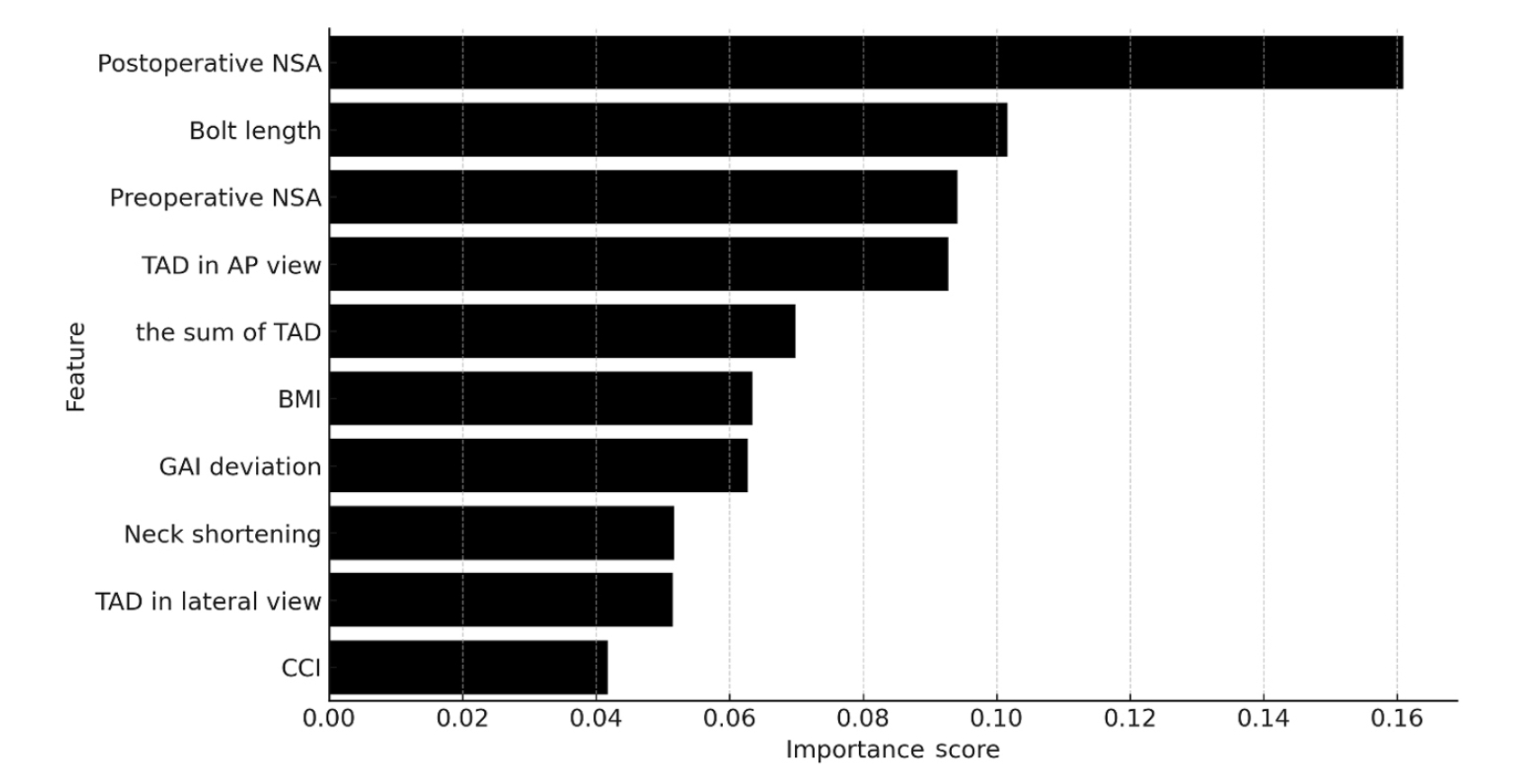
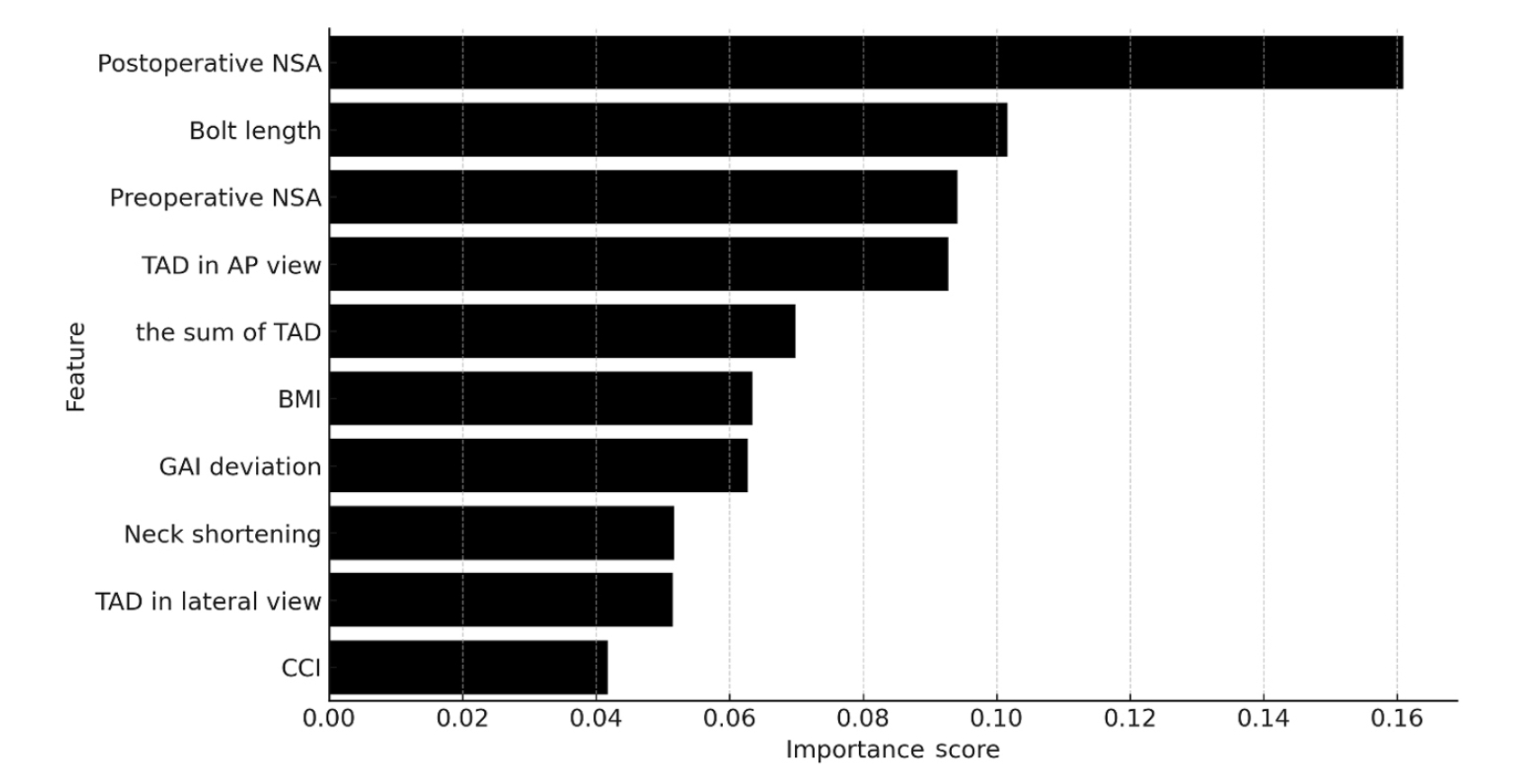
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery.
Level of Evidence: III.
-
Computed Tomography Image Analysis of the Fusion Site of Subtalar Arthrodesis for Traumatic Arthritis after a Displaced Intraarticular Calcaneal Fracture
-
Hong Gi Park, Jae Ang Sim, Han Soul Kim, Byung Hoon Lee
-
J Korean Fract Soc 2019;32(3):121-127. Published online July 31, 2019
-
DOI: https://doi.org/10.12671/jkfs.2019.32.3.121
-
-
 Abstract Abstract
 PDF PDF
- PURPOSE
The study examined the fusion site and characteristics of the subtalar arthrodesis after intraarticular calcaneal fractures using computed tomography.
MATERIALS AND METHODS
The clinical results and computed tomographic analysis of the fusion site were reviewed in 18 patients who were followed-up for a minimum of six months after undergoing subtalar arthrodesis due to traumatic arthritis caused by an intra-articular calcaneal fracture from December 2012 to April 2017.
RESULTS
An evaluation of clinical results after subtalar arthrodesis revealed statistically significant improvements. In all cases, arthritis was found in the injured articular surface, which was displaced superolaterally from the initial primary fracture line of the calcaneus. Six months after arthrodesis, the subtalar fusion rate was 80.0% (16/20). Of these, 14 cases had a cannulated screw inserted in the uninjured site that is medial to the primary fracture line. Joint fusion was observed on the uninjured articular surface in 17 cases (85.0%).
CONCLUSION
Joint fusion was initially achieved at the uninjured posterior facet after subtalar arthrodesis due to traumatic arthritis caused by a displaced intra-articular calcaneal fracture. This suggests that meticulous surgical techniques and cannulated screw positioning at the uninjured site will promote joint fusion.
|