Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 32(2); 2019 > Article
- Review Article Locked Plating in Elderly Patients with Distal Femur Fracture: How to Avoid Complications?
- Chul Young Jang, Je Hyun Yoo
-
Journal of Musculoskeletal Trauma 2019;32(2):112-119.
DOI: https://doi.org/10.12671/jkfs.2019.32.2.112
Published online: April 30, 2019
- 961 Views
- 15 Download
- 0 Crossref
- 0 Scopus
Abstract
Distal femur fractures in elderly patients with osteoporosis are complicated because poor bone quality makes screw purchase and fixation less secure, presenting many clinical challenges to the orthopedic surgeon. Minimally invasive locked plating using an angularly stable locking compression plate has become an integral tool for achieving secure fixation in osteoporotic distal femur fractures with improved biomechanical performance. On the other hand, complications, such as implant failure and periplate fracture, have still occurred. This paper describes the principles of internal fixation in minimally invasive lateral locked plating in elderly patients with osteoporotic distal femur fractures as well as how to avoid complications.
Published online Apr 16, 2019.
https://doi.org/10.12671/jkfs.2019.32.2.112
Locked Plating in Elderly Patients with Distal Femur Fracture: How to Avoid Complications?
 , M.D.
and Je-Hyun Yoo
, M.D.
and Je-Hyun Yoo , M.D., Ph.D.
, M.D., Ph.D.
Abstract
Distal femur fractures in elderly patients with osteoporosis are complicated because poor bone quality makes screw purchase and fixation less secure, presenting many clinical challenges to the orthopedic surgeon. Minimally invasive locked plating using an angularly stable locking compression plate has become an integral tool for achieving secure fixation in osteoporotic distal femur fractures with improved biomechanical performance. On the other hand, complications, such as implant failure and periplate fracture, have still occurred. This paper describes the principles of internal fixation in minimally invasive lateral locked plating in elderly patients with osteoporotic distal femur fractures as well as how to avoid complications.
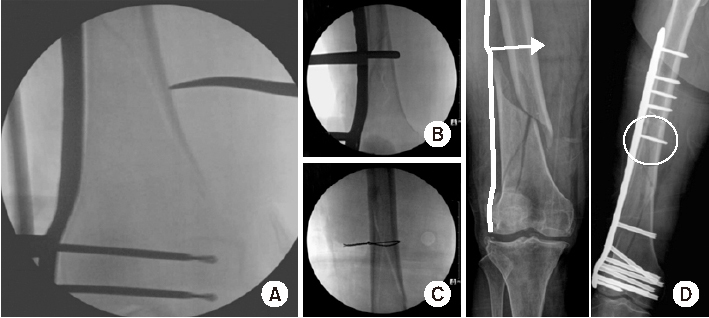
Fig. 1
Indirect reduction in the sagittal plane in a distal femur fracture. (A) Posterior angulation by deforming forces of the surrounding muscles. Reduction methods using a bump beneath the distal thigh (B) or a Schanz screw (C).
Fig. 2
Direct reduction methods in the coronal plane in distal femur fractures using a long hemostatic tonsil (A), Collinear reduction clamp (B), percutaneous wiring (C), or conventional cortical screw (D).
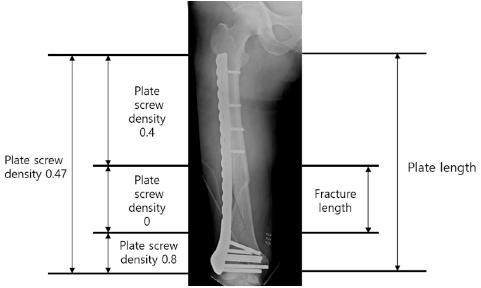
Fig. 3
Appropriate plate length and plate-screw density after minimally invasive plate osteosynthesis using a locking plate in osteoporotic distal femur fractures.
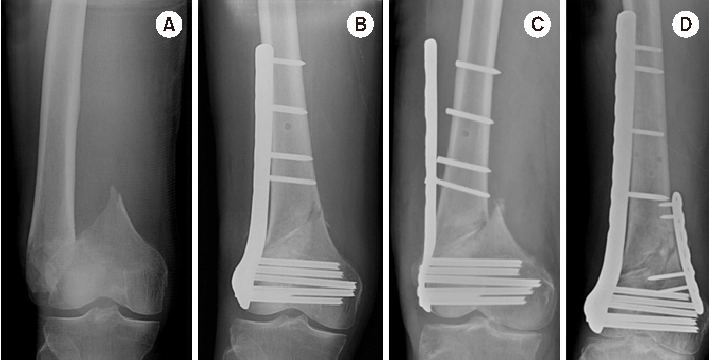
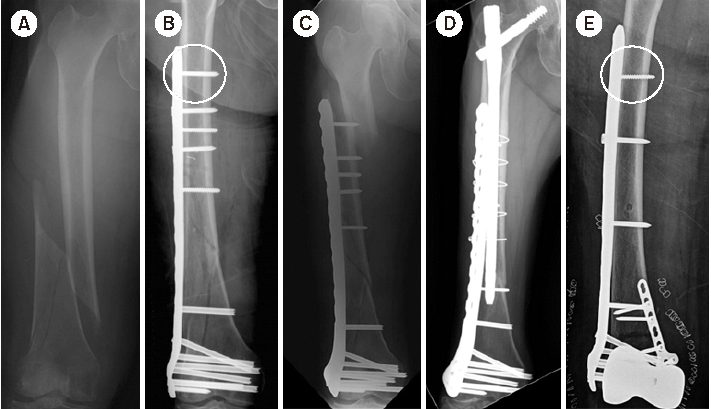
Fig. 4
(A) Distal femur fracture in a 70-year-old male. (B) Postoperative anteroposterior radiograph after minimally invasive locked plating. (C) Fixation failure along with broken locking screws two months after surgery. (D) Anteroposterior radiograph seven months after double plating showing bony union.
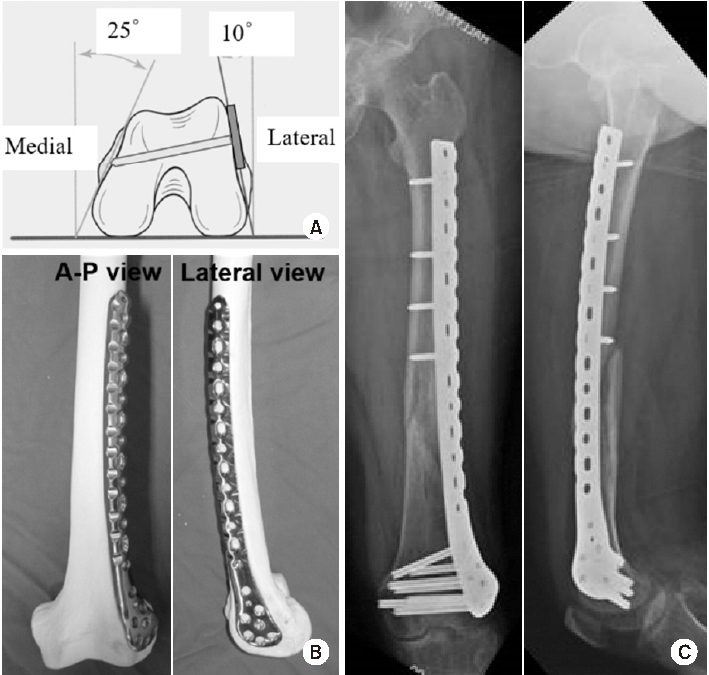
Fig. 5
(A) Schematic diagram showing the axial shape of the distal femur and the appropriate length of distal locking screw. (B) Anteroposterior (A–P) and lateral photos showing the appropriate position of the lateral anatomical locking plate in the distal femur model. (C) A–P and lateral radiographs showing the appropriate position of the locking plate fixed in a distal femur fracture of a 72-year-old female patient.
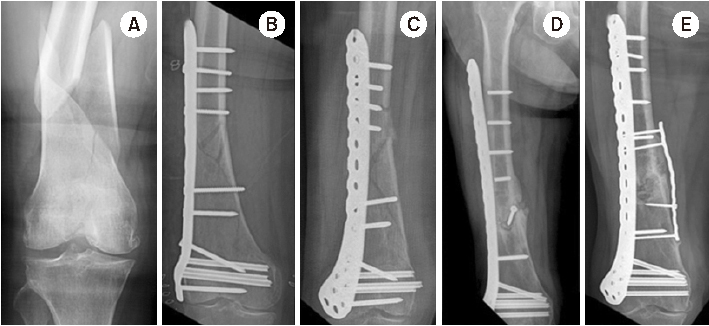
Fig. 6
(A) Radiograph of a distal femur fracture of a 74-year-old female after a ground-level fall. (B) Postoperative radiograph after a closed reduction and minimally invasive locked plating. (C) Six-week postoperative radiograph showing a stress riser fracture around the outermost locking screw after slip-down injury. (D) Radiograph showing bony union two years after overlapping intramedullary nailing. (E) Postoperative radiograph showing locked plating using a conventional cortical screw instead of a locking screw as a proximal outermost screw to minimize the stress riser.
Fig. 7
(A) Radiograph of a distal femur fracture of a 74-year-old female after a ground-level fall. (B) Postoperative radiograph after a closed reduction and minimally invasive locked plating. (C) Six-week postoperative radiograph showing a stress riser fracture around the outermost locking screw after slip-down injury. (D) Radiograph showing bony union two years after overlapping intramedullary nailing. (E) Postoperative radiograph showing locked plating using a conventional cortical screw instead of a locking screw as a proximal outermost screw to minimize the stress riser.
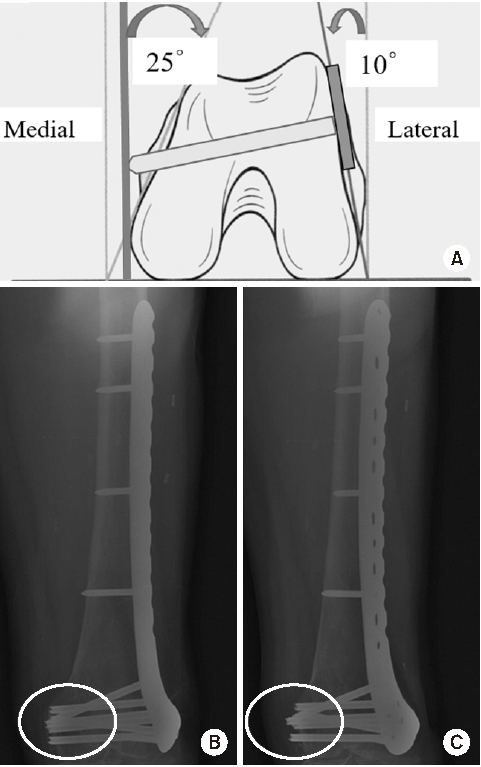
Fig. 8
(A) Schematic diagram showing the axial shape of the distal femur and the protrusion of distal locking screw. (B) True anteroposterior radiograph showing that the lengths of the distal locking screws appear to be appropriate. (C) Radiograph taken after rotating a thigh approximately 25° internally, showing the protrusion of multiple screws across the medial cortex.
Financial support:None.
Conflict of interests:None.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 PubReader
PubReader Cite
Cite

