Abstract
-
Background
Posterior malleolar fractures frequently accompany rotational ankle fractures. However, the morphological relationship between lateral and posterior malleolar fractures in supination-external rotation (SER) ankle fractures remains unclear. This study aimed to classify lateral malleolar fracture patterns in SER type 3 and 4 ankle fractures and investigated their associations with posterior malleolar fracture morphology.
-
Methods
We retrospectively reviewed 132 patients with SER type 3 or 4 ankle fractures and concurrent posterior malleolar fractures between January 2016 and December 2021. Lateral malleolar fractures were categorized as fibular fractures extending <4.5 cm proximal to the ankle joint (102 ankles) or fibular fractures extending ≥4.5 cm proximal to the ankle joint (30 ankles) based on posterior cortex height measured using three-dimensional computed tomography (3D-CT). Posterior malleolar fracture morphology was assessed using the Haraguchi and Bartonicek classifications. Quantitative parameters—including fracture height, angle, and articular involvement—were analyzed using 3D-CT imaging.
-
Results
Fibular fractures extending ≥4.5 cm proximal to the ankle joint were associated with a significantly higher frequency of Haraguchi type II and Bartonicek types 3 and 4 posterior malleolar fractures. This group also exhibited greater articular involvement (19.2% vs. 12.0%) and posterior cortical height (55.4 mm vs. 24.8 mm) compared to the <4.5 cm group (all P<0.001).
-
Conclusions
In SER type 3 and 4 ankle fractures, a fibular fracture extending ≥4.5 cm proximal to the ankle joint may be associated with posterior malleolar fractures exhibiting greater articular involvement and medial extension. Preoperative evaluation of the lateral malleolar fracture pattern may provide useful insights into posterior malleolar morphology and assist in surgical planning. However, these findings should be interpreted with caution due to inherent study limitations.
-
Level of evidence
IV.
-
Keywords: Ankle fractures, Ankle joint, Retrospective studies, Supination, X-Ray computed tomography
Introduction
Background
Posterior malleolar fractures account for approximately 40% of all rotational ankle fractures [
1,
2]. The posterior malleolus forms the weight-bearing portion of the tibial plafond, playing a critical role in tibiotalar load transmission and rotational ankle stability [
3,
4]. Inadequate diagnosis or management of posterior malleolar fractures can lead to persistent instability and subsequent degenerative changes in the ankle joint [
5,
6].
Accurate preoperative assessment of posterior malleolar fracture size and pattern is essential for optimal evaluation and surgical planning [
7]. Historically, fixation was recommended when the fracture fragment involved 25%–30% or more of the articular surface [
8-
10]. Recent studies, however, emphasize the importance of considering fracture morphology in addition to fragment size when determining surgical indications [
11,
12]. Factors influencing posterior malleolar fracture morphology include injury mechanism and the anatomical configuration of the fibular incisura [
10,
13,
14]. Despite this, no prior studies have analyzed posterior malleolar fracture morphology in relation to lateral malleolar fracture patterns in supination-external rotation (SER)-type ankle fractures, which are the most frequent cause of such injuries [
15].
The Weber classification, based on the location of the anterior cortex of the fibular fracture, designates all SER-type fractures as type B. Previous research has further characterized Weber B-type lateral malleolar fractures. Boden et al. [
16] found that fibular fractures extending more than 4.5 cm proximal to the ankle joint are often associated with excessive syndesmotic widening in cadaveric models. Yamaguchi et al. [
17] validated this biomechanical threshold in a prospective clinical study. Park et al. [
18] also reported that lateral malleolar fractures extending more than 4.5 cm above the joint line have a threefold higher incidence of syndesmotic instability compared to shorter fractures.
We hypothesized that fibular fractures extending more than 4.5 cm proximal to the ankle joint would be associated with larger posterior malleolar fragments. This association may provide clinically relevant information for preoperative assessment and surgical planning, particularly in anticipating the need for internal fixation of the posterior malleolus. Therefore, this study classified lateral malleolar fracture patterns in SER type 3 and 4 ankle fractures using three-dimensional computed tomography (3D-CT) and analyzed their association with posterior malleolar fracture morphology.
Methods
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Chonnam National University Hospital (IRB no., CNUH-2025-151).
Study design
This was a retrospective observational study evaluating the relationship between lateral malleolar fracture patterns and posterior malleolar fracture morphology in supination-external rotation (SER) type 3 and 4 ankle fractures. It was described according to the STROBE statement (
https://www.strobe-statement.org/).
We retrospectively analyzed ankle fracture patients treated at our institution between January 2016 and December 2021 at Chonnam National University Hospital, Gwangju, Korea.
All patients underwent preoperative anteroposterior, lateral, and mortise radiographs, as well as 3D-CT scans and at least 1 year of follow-up. CT data were acquired using either a 128-channel (SOMATOM Definition Flash, Siemens) or a 64-channel (Discovery 750 HD, GE Healthcare) CT scanner.
Given the absence of a standard subclassification for lateral malleolar fractures associated with posterior malleolar fractures, we used the 4.5 cm posterior cortex height threshold from previous studies to divide cases into two groups [
16-
18]. Lateral malleolar fractures were categorized as fibular fracture extending <4.5 cm proximal to the ankle joint (<4.5 cm group) or fibular fracture extending ≥4.5 cm proximal to the ankle joint (≥4.5 cm group) based on posterior cortex height measured using 3D-CT. The injury mechanism was retrospectively classified based on clinical records. Ground-level falls were defined as slips, trips, or missteps on flat surfaces or low steps (e.g., 1–2 stairs), without vertical descent from a significant height. Falls from height were defined as vertical descent injuries from more than 1 m. Motor vehicle collisions and high-impact sports injuries (e.g., soccer, basketball) were also recorded separately based on clinical documentation.
All enrolled patients underwent plate fixation for lateral malleolar fracture through a posterolateral approach. Posterior malleolar fixation was performed selectively based on intraoperative assessment. If satisfactory reduction was achieved via ligamentotaxis, screw fixation was performed in an anteroposterior direction. When reduction was insufficient, direct reduction and fixation of the posterior fragment were performed through a posterolateral window using screws or a plate.
Participants
A total of 150 patients (150 ankles) who underwent open reduction and internal fixation for SER type 3 and 4 ankle fractures were initially enrolled. Patients with open fractures, skeletal immaturity, osteoporotic fractures, diabetes-related fractures, polytrauma, or rotational deformities were excluded. Ultimately, 132 patients (132 ankles) met the inclusion criteria and were categorized as <4.5 cm group (102 ankles) or ≥4.5 cm group (30 ankles).
Variables
Primary outcome variable was a Posterior malleolar fracture morphology. Lateral malleolar fracture pattern, defined by posterior cortex height measured on 3D-CT was an exposure variable. Age, sex, body mass index (BMI), and injury mechanism were covariates.
Data sources/measurement
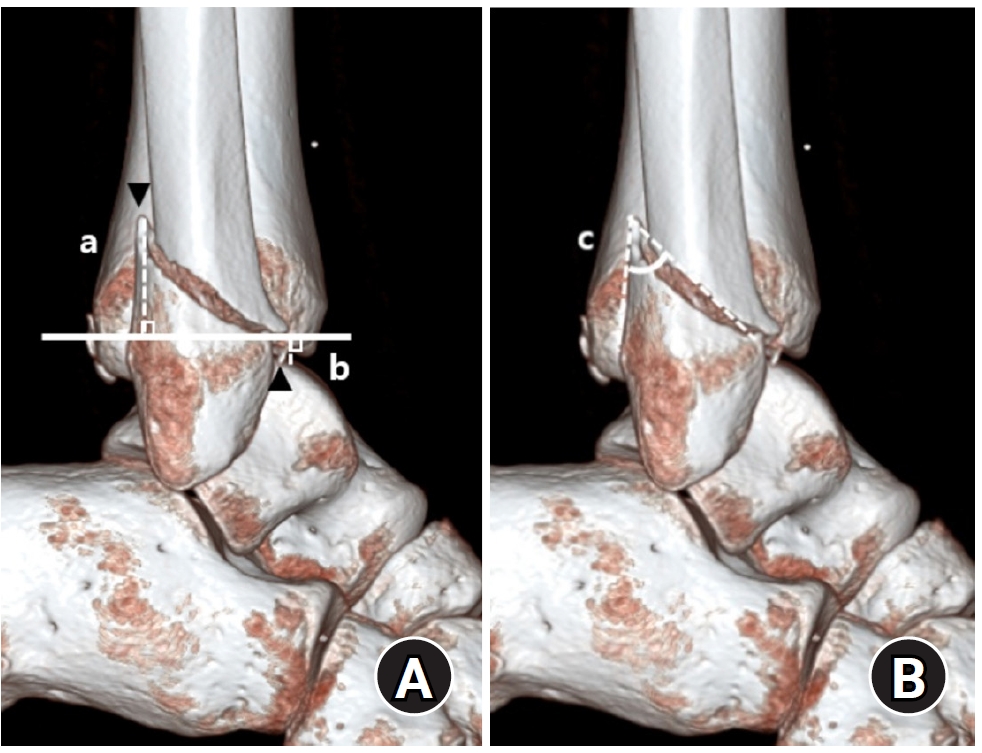
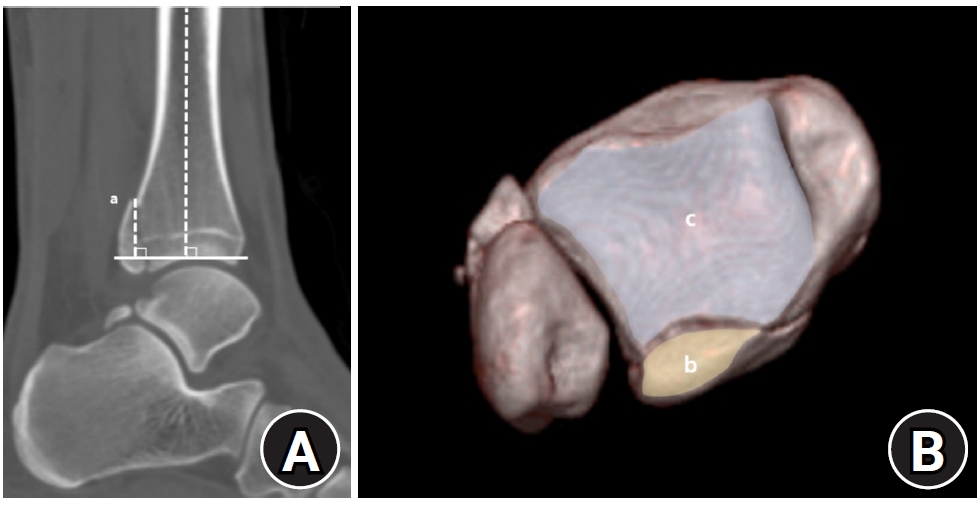
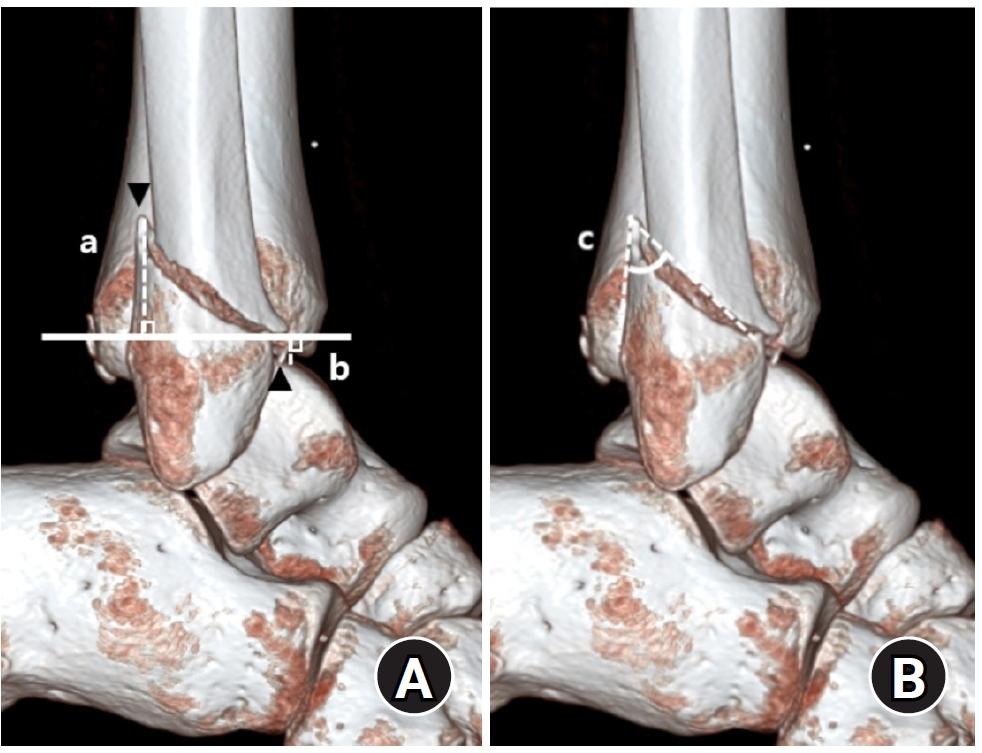
Demographic and clinical data were obtained from electronic medical records. Radiographic data were derived from 3D-CT scans. Radiographic analysis was performed using 3D-CT to assess the characteristics of both lateral and posterior malleolar fractures. Lateral malleolar fracture patterns were determined by measuring the vertical distance between the highest posterior cortex or lowest anterior cortex of the fracture and a line perpendicular to the tibial axis at the distal tibial articular surface. The angle between the posterior cortex of the lateral malleolus and the line connecting the anterior and posterior cortical points was defined as the fracture angle (
Fig. 1).
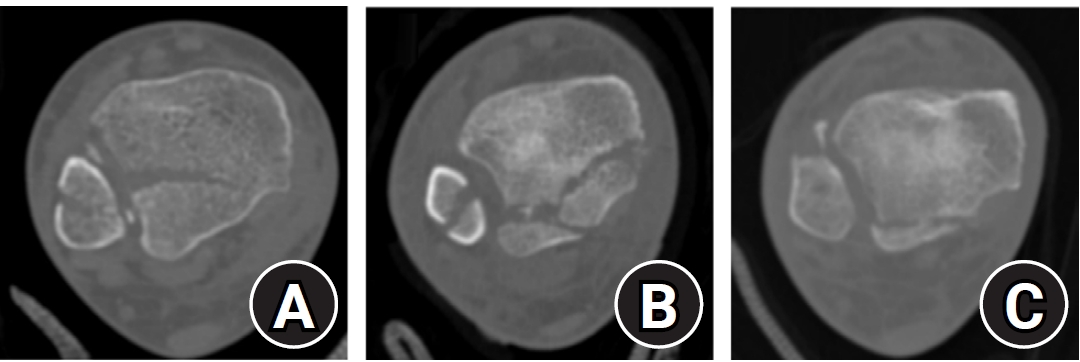
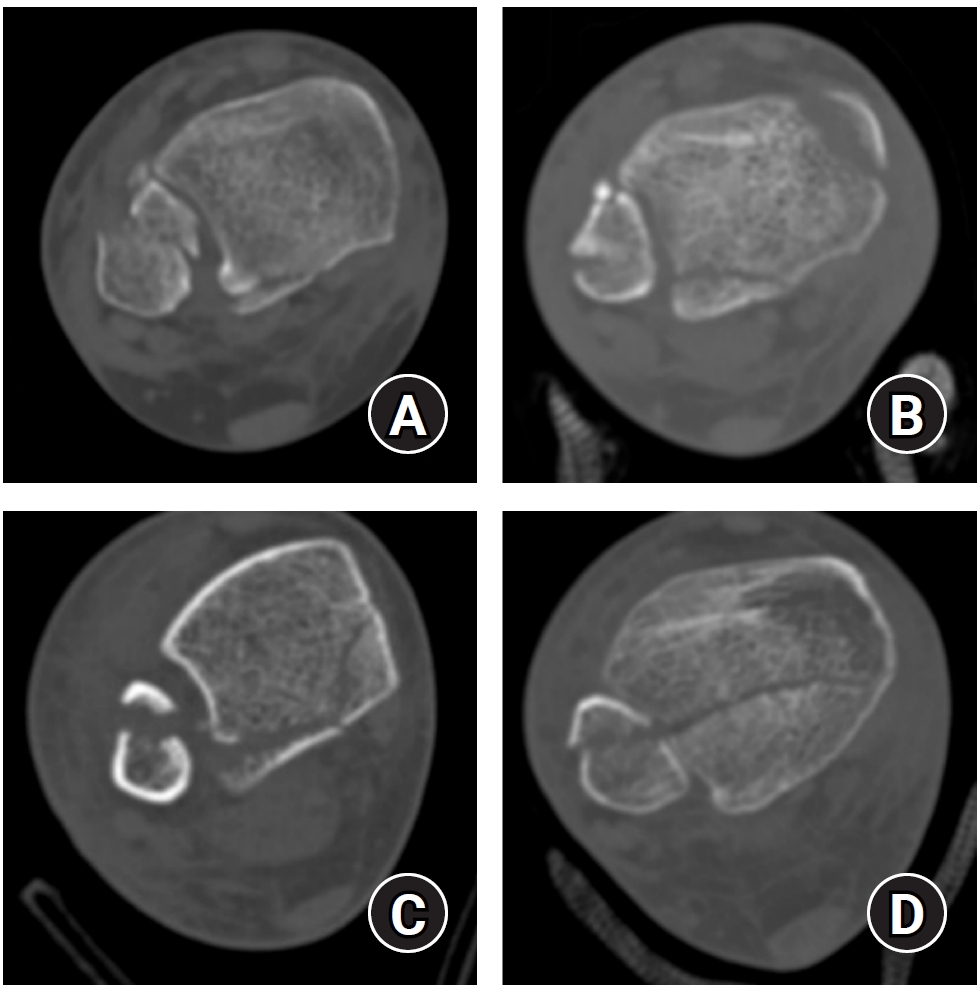
Posterior malleolar fracture morphology was classified according to the Haraguchi and Bartonicek systems (
Figs. 2,
3) [
19,
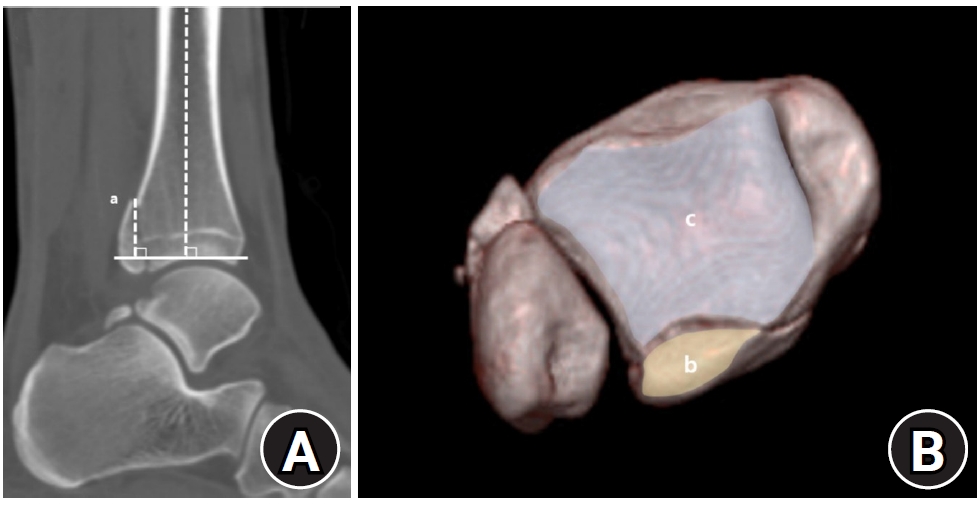
20]. The peak height of the posterior malleolar fracture was measured as the vertical distance from the highest point of the distal tibial articular surface to the fracture apex in the sagittal plane (
Fig. 4A). The articular surface area of the posterior malleolar fragment was calculated using the region of interest tool in a picture archiving and communication system (Maroview 5.4; INFINITT Healthcare) (
Fig. 4B). All quantitative radiographic measurements were performed by two orthopedic surgeons; mean values were used. For categorical variables, disagreements were resolved by consensus.
To reduce confounding bias, multivariate regression analysis was done by adjusting for age, BMI, and injury mechanism.
Study size
Study size estimation was not done due to the retrospective design. All eligible cases were included in the study period.
Statistical methods
Statistical analysis was conducted using IBM SPSS ver. 29.0 (IBM Corp.). The normality of continuous variables was assessed using the Kolmogorov-Smirnov test, followed by independent t-tests for group comparisons. Categorical variables were analyzed with the chi-square test or Fisher exact test. For radiographic outcomes, multivariable regression analysis was performed to adjust for baseline characteristics, including age, BMI, and injury mechanism, as potential confounders. Interrater reliability was assessed for continuous radiographic parameters using the intraclass correlation coefficient (ICC) with a 95% confidence interval, based on a 2-way random effects model with absolute agreement. ICC values were interpreted as follows: poor (<0.20), fair (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and excellent (0.81–1.00).
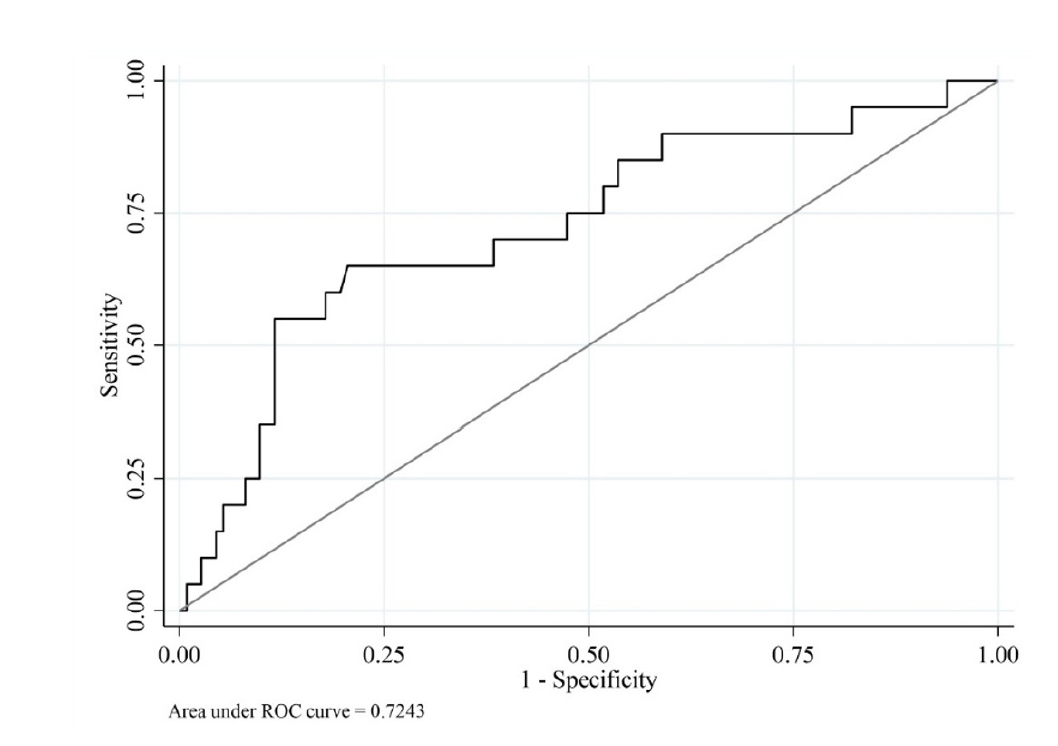
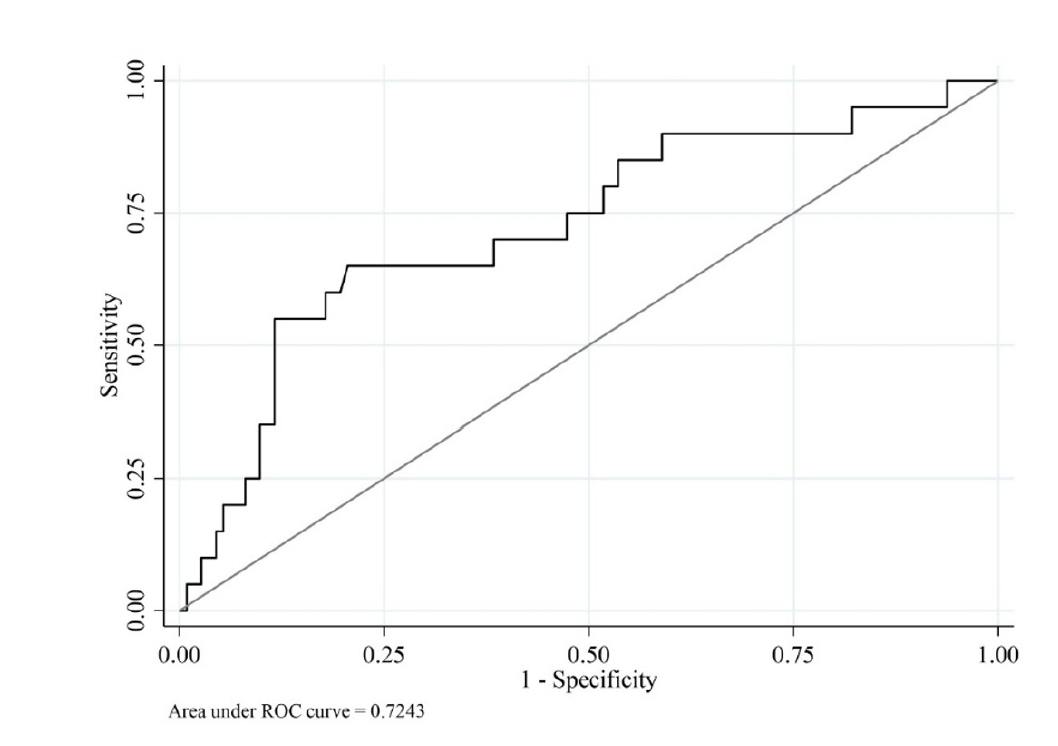
We performed a receiver operating characteristic (ROC) curve analysis to validate the 4.5 cm threshold for posterior cortex height used to classify lateral malleolar fracture patterns. A posterior malleolar articular surface involvement of ≥25%, which is commonly accepted as a surgical indication, was used as the reference standard [
21]. The optimal cut-off value for posterior cortex height was determined using Youden’s index. All analyses were reviewed by a statistician. Statistical significance was set at P<0.05.
Results
Participants
Classification by lateral malleolar fracture pattern identified 102 cases (77.3%) of fibular fracture extending <4.5 cm proximal to the ankle joint and 30 cases (22.7%) of fibular fracture extending ≥4.5 cm proximal to the ankle joint (
Table 1). The mean age was 54.2 years in the <4.5 cm group and 43.2 years in the ≥4.5 cm group, representing a statistically significant difference (P=0.004). Regarding the injury mechanism, ground-level falls accounted for 85.3% of cases in the <4.5 cm group and 66.7% in the ≥4.5 cm group. In contrast, the ≥4.5 cm group showed higher proportions of high-impact sports injuries (20.0% vs. 5.9%) and motor vehicle collisions (13.3% vs. 5.9%) compared to the <4.5 cm group.
The <4.5 cm group had a mean anterior cortical height of −1.1 mm, while the ≥4.5 cm group averaged 3.7 mm (
Table 2). These data indicate that fibular fracture extending <4.5 cm proximal to the ankle joint typically originated below the distal tibial articular plafond, whereas fibular fracture extending ≥4.5 cm proximal to the ankle joint generally began above it. The ≥4.5 cm group demonstrated greater posterior cortical height (55.4 mm vs. 24.8 mm) and a smaller fracture angle (20.5° vs. 38.1°). Differences in anterior and posterior cortical heights and fracture angle were statistically significant (all P<0.001).
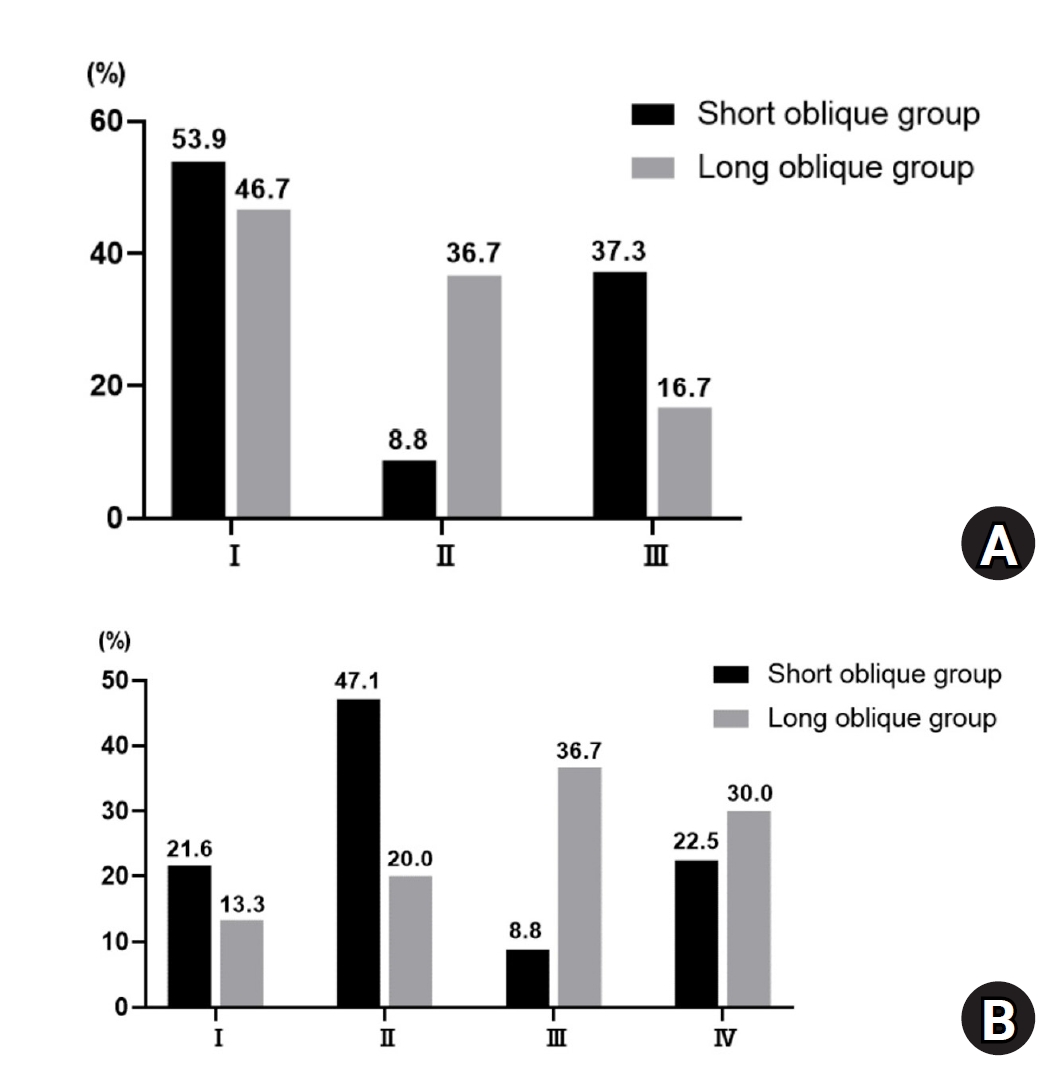
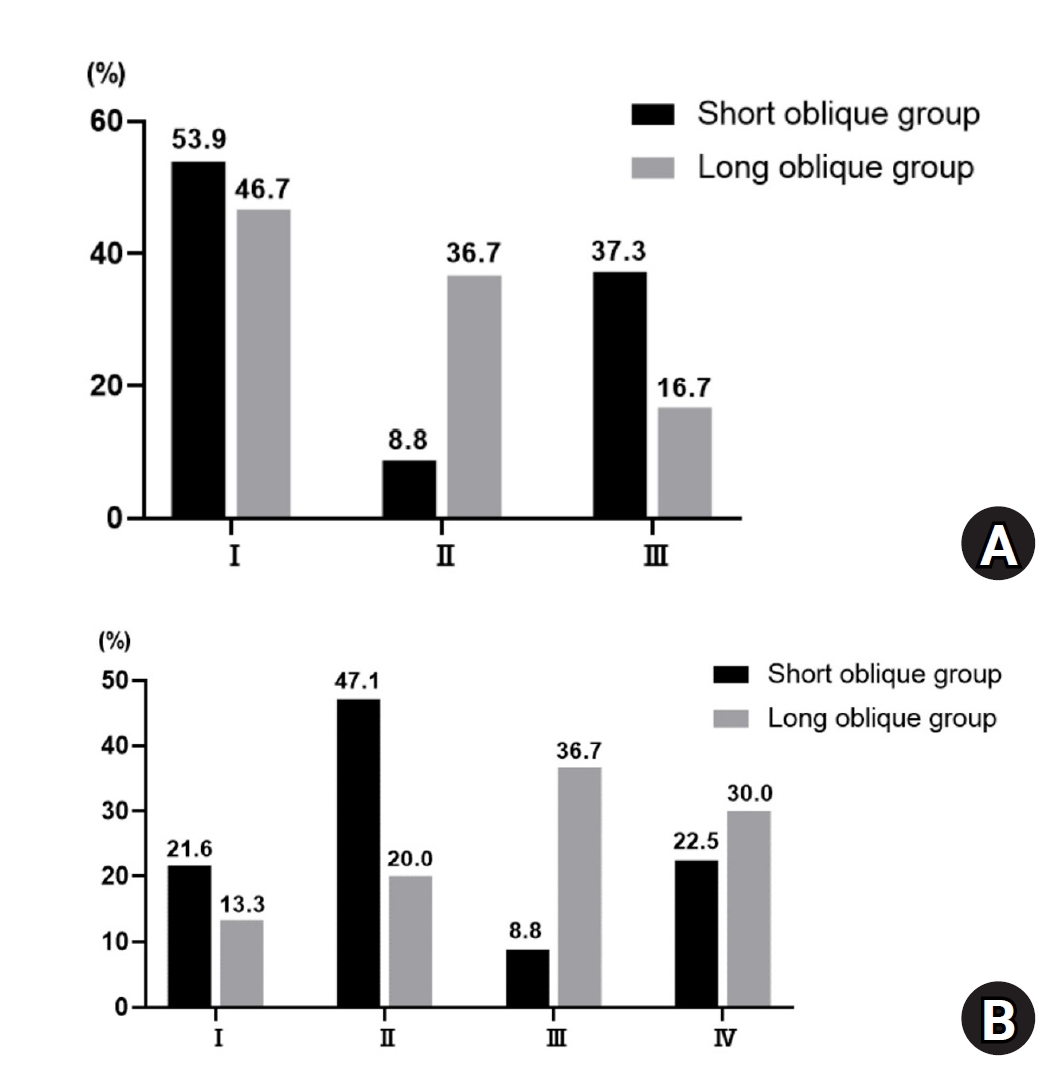
Regarding posterior malleolar fracture morphology, Haraguchi type III (small shell fragment) was more common in the <4.5 cm group, while type II (medial extension) predominated in the ≥4.5 cm group (P<0.001) (
Table 2,
Fig. 5). Similarly, the Bartonicek classification showed that type 1 (extra-incisural fragment with intact fibular notch) and type 2 (small posterolateral fragment extending into the fibular notch) were more frequent in the <4.5 cm group, whereas type 3 (posteromedial two-part fragment involving the medial malleolus) and type 4 (large posterolateral triangular fragment involving more than one-third of the notch) were predominant in the ≥4.5 cm group (P<0.001).
The mean vertical peak height of the posterior malleolar fracture was greater in the ≥4.5 cm group (21.0 mm) than in the <4.5 cm group (15.2 mm; P=0.002). The articular surface area of the posterior malleolar fragment at the distal tibial articular surface was also significantly larger in the ≥4.5 cm group (242.2 mm2 vs. 140.7 mm2; P<0.001). The fragment involved 19.2% of the tibial plafond in the ≥4.5 cm group compared to 12.0% in the <4.5 cm group, indicating significantly greater absolute size and articular involvement in fibular fracture extending ≥4.5 cm proximal to the ankle joint (P<0.001). These results suggest that posterior malleolar fragments are larger in the ≥4.5 cm group.
Interrater reliability
All radiographic parameters in both groups, measured independently by two orthopedic surgeons, demonstrated excellent interrater reliability (
Table 3). The highest ICC was observed for the anterior height of the lateral malleolar fracture (0.984, P<0.001), while the lowest was for the articular involvement of the posterior malleolar fracture (0.846, P<0.001).
ROC curve analysis demonstrated an area under the curve of 0.72, indicating acceptable discrimination. The optimal cut-off value for posterior cortex height was 39.3 mm, yielding a sensitivity of 0.65, specificity of 0.80, and a Youden’s index of 0.45 (
Fig. 6).
Discussion
Key results
This study is the first to assess the association between lateral malleolar fracture patterns and posterior malleolar fracture morphology in SER type 3 and 4 ankle fractures. The principal finding is that fibular fracture extending ≥4.5 cm proximal to the ankle joint are linked to larger posterior malleolar fragments, greater articular involvement, more frequent medial extension, and higher peak fracture height. These features are commonly considered when determining the need for posterior malleolar fixation. Therefore, identifying a fibular fracture extending ≥4.5 cm proximal to the ankle joint pattern on initial radiographs may provide useful insight into the underlying posterior malleolar morphology and assist in preoperative planning, even before 3D-CT assessment.
Interpretation/comparison with previous findings
We found that the fibular fracture extending ≥4.5 cm proximal to the ankle joint pattern was more prevalent among younger patients. This may reflect the morphological similarity between fibular fracture extending ≥4.5 cm proximal to the ankle joint—which extend more proximally on the posterior cortex—and Weber C-type fibular fractures, typically observed in pronation-external rotation (PER) ankle injuries. As PER fractures generally result from higher-energy trauma and are more common in young males, it is reasonable to infer that fibular fracture extending ≥4.5 cm proximal to the ankle joint share similar demographic characteristics [
22]. This observation is consistent with previous research on posterior malleolar fracture morphology. Yi et al. [
13] reported that larger fragments and medial extension types were more frequent in PER than SER injuries. In our study, the ≥4.5 cm group similarly showed more Haraguchi type II and Bartonicek types 3 and 4 fractures, indicating a tendency toward larger, medially extending posterior malleolar fragments. In addition, the proportion of injuries other than ground-level falls was higher in the ≥4.5 cm group (33.3%) than in the <4.5 cm group (14.7%), suggesting that this fracture pattern may be associated with relatively higher-energy trauma.
Posterior malleolar fractures are common, accounting for about 40% of rotational ankle fractures [
1,
2]. The posterior malleolus forms the weight-bearing portion of the tibial plafond and contributes to the syndesmosis, playing a key role in tibiotalar load transfer and rotational stability [
3,
4]. Inadequate management can result in complications such as instability and posttraumatic arthritis, leading to poor functional outcomes [
23-
25]. Solan et al. [
26] propose that fixation is often beneficial, as it restores the articular surface and fibular length, enhances syndesmotic stability, and facilitates earlier rehabilitation. Blom et al. [
11] further highlighted the importance of fixation, particularly in fractures with medial extension, as these are frequently associated with deep deltoid ligament injuries and a higher risk of persistent instability.
The indications for fixation and optimal surgical approach for posterior malleolar fractures remain debated [
19,
27]. Traditionally, fixation was advised when more than 25%–30% of the articular surface was involved, based on lateral radiographs [
8-
10]. However, recent studies have shown that plain radiographs often overestimate fragment size and may be unreliable for assessing articular involvement [
28,
29]. Lee et al. [
7] demonstrated that articular involvement measured on radiographs is frequently overestimated and varies with fracture morphology, underscoring the need for 3D-CT for accurate evaluation. In our study, although the ≥4.5 cm group had significantly greater articular involvement than the <4.5 cm group, mean involvement in both groups was less than 20%. While 3D-CT enables direct measurement of articular involvement, clear surgical guidelines based on fragment size are lacking and require further research.
First, its retrospective design and relatively small sample size—particularly the imbalance in group sizes between the two groups—may have limited the strength of the analysis. This imbalance also increases the risk of overinterpretation, especially for findings derived from the smaller group. Second, although two orthopedic surgeons performed the radiographic measurements, only interrater reliability was assessed, and intrarater reliability was not evaluated. Third, although the primary aim of this study was to analyze radiographic morphology rather than clinical results, the absence of clinical outcomes remains a key limitation. This limited the ability to evaluate the association between lateral malleolar fracture pattern and functional outcomes. Fourth, although we used a 4.5 cm posterior cortex height threshold for group classification based on previous literature, our ROC analysis identified an optimal cut-off of 39.3 mm. As this result was derived solely from articular involvement, which is not the only factor guiding fixation decisions for posterior malleolar fractures, and given the limited sample size of our study, further research is warranted to validate and refine these criteria. Finally, although we adjusted for age, BMI, and injury mechanism in the analysis of radiographic outcomes, other unmeasured confounding factors such as bone density may have influenced fracture morphology and were not included in the analysis.
Conclusions
SER type 3 and 4 ankle fractures with a fibular fracture extending ≥4.5 cm proximal to the ankle joint pattern may be associated with posterior malleolar fragments exhibiting greater articular involvement and more frequent medial extension. Thorough preoperative assessment of the lateral malleolar fracture pattern may suggest underlying posterior malleolar morphology and help inform surgical planning. However, given the small sample size and imbalance between groups, the findings should be interpreted with caution.
Article Information
-
Author contribution
Conceptualization: JEK, CJP, JYL, KBL, GWL. Data curation: JEK, CJP, GWL. Formal analysis: JEK, CJP, KBL, GWL. Methodology: JEK, CJP. Project administration: JYL, KBL, GWL. Investigation: JEK, CJP. Resources: JEK, CJP. Software: GWL. Supervision: KBL, GWL. Writing-original draft: JEK, GWL.
Writing-review & editing: JEK, JYL, KBL, GWL. All authors read and approved the final manuscript.
-
Conflict of interests
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
We are grateful to Cho Hee Hwang for her expert assistance with the statistical analysis.
-
Supplementary materials
None.
Fig. 1.Radiographic assessment of fracture characteristics. (A) Posterior height (a) and anterior height (b) represent the vertical distances from the highest point of the posterior cortex (▼) and the lowest point of the anterior cortex (▲) of the distal lateral fibula, respectively, to the line perpendicular to the tibial axis that intersects the distal tibial articular plafond. (B) The fracture angle (c) of the lateral malleolar fragment is defined as the angle between the posterior cortex of the lateral malleolus and the line connecting the anterior and posterior cortical points of the fracture.
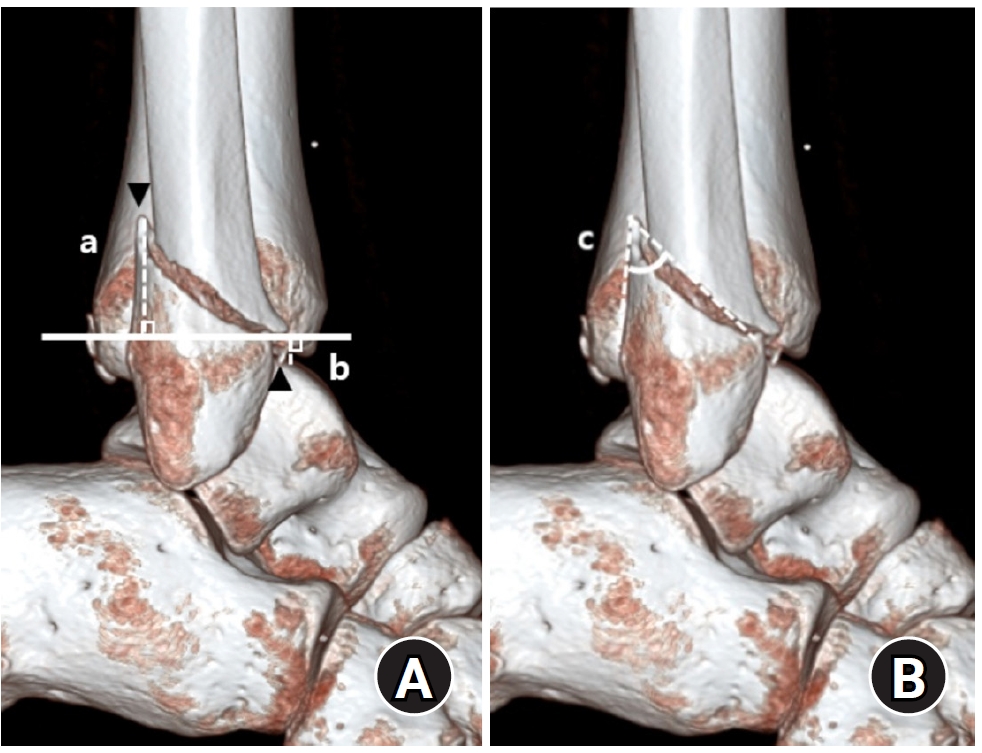
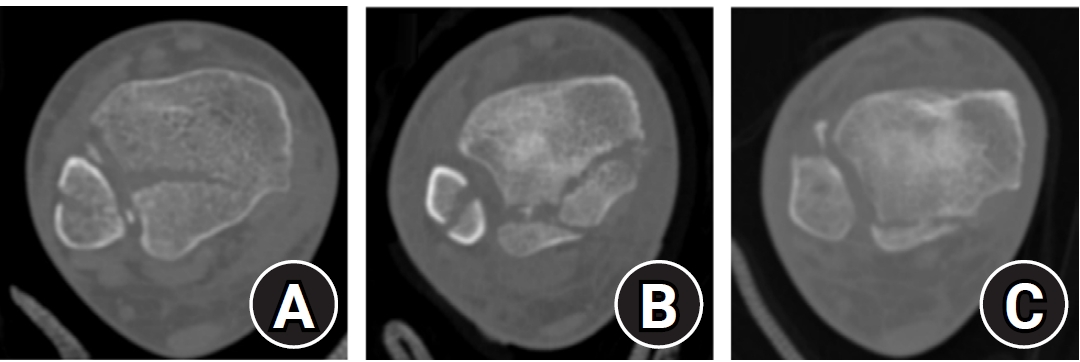
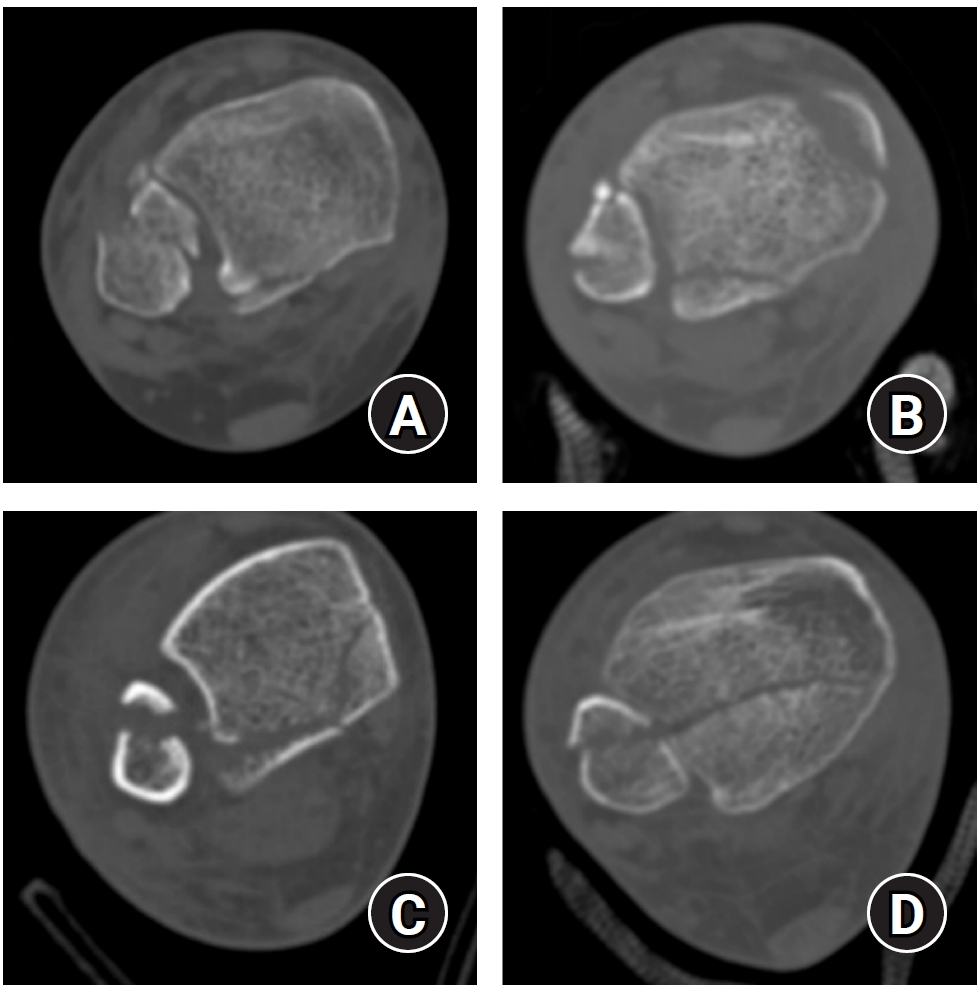
Fig. 2.Haraguchi classification of posterior malleolar fractures. (A) Type I: posterolateral-oblique type. (B) Type II: medial-extension type. (C) Type III: small-shell type.
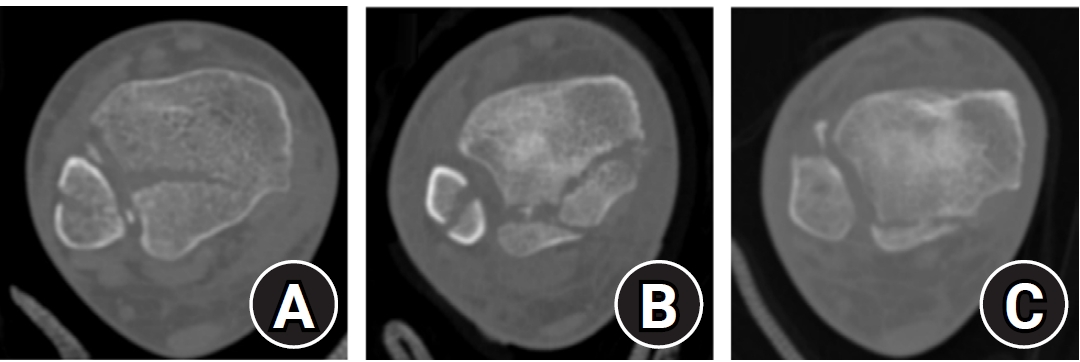
Fig. 3.Bartonicek classification of posterior malleolar fractures. (A) Type 1: extraincisural fragment with an intact fibular notch. (B) Type 2: posterolateral fragment extending into the fibular notch. (C) Type 3: posteromedial two-part fragment involving the medial malleolus. (D) Type 4: large posterolateral triangular fragment.
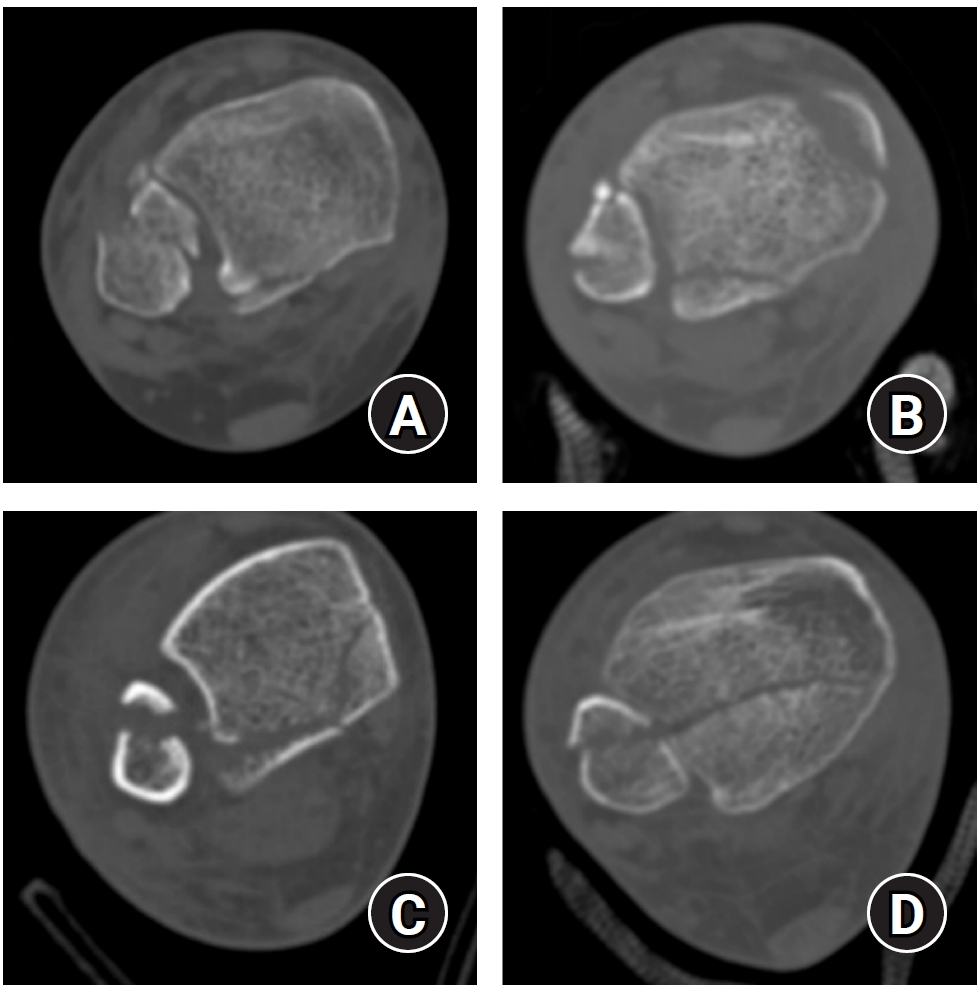
Fig. 4.(A) Peak height (a) of the posterior malleolar fracture is defined as the vertical distance from the highest point of the distal tibial articular plafond to the apex of the posterior malleolar fragment on the sagittal plane. (B) The articular surface area (mm2) of the posterior malleolar fracture fragment (b) was measured using the region of interest tool in a picture archiving and communication system. Articular involvement (%) was calculated as the ratio of the fractured area (b) to the total tibial plafond articular surface area (b+c).
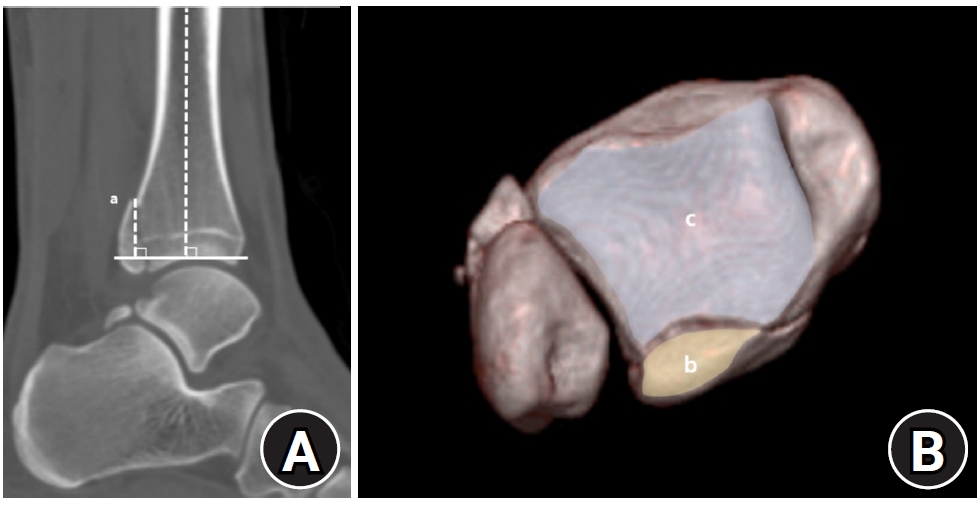
Fig. 5.(A) Distribution of Haraguchi classification types in the <4.5 cm and ≥4.5 cm groups. (B) Distribution of Bartonicek classification types in the <4.5 cm and ≥4.5 cm groups.
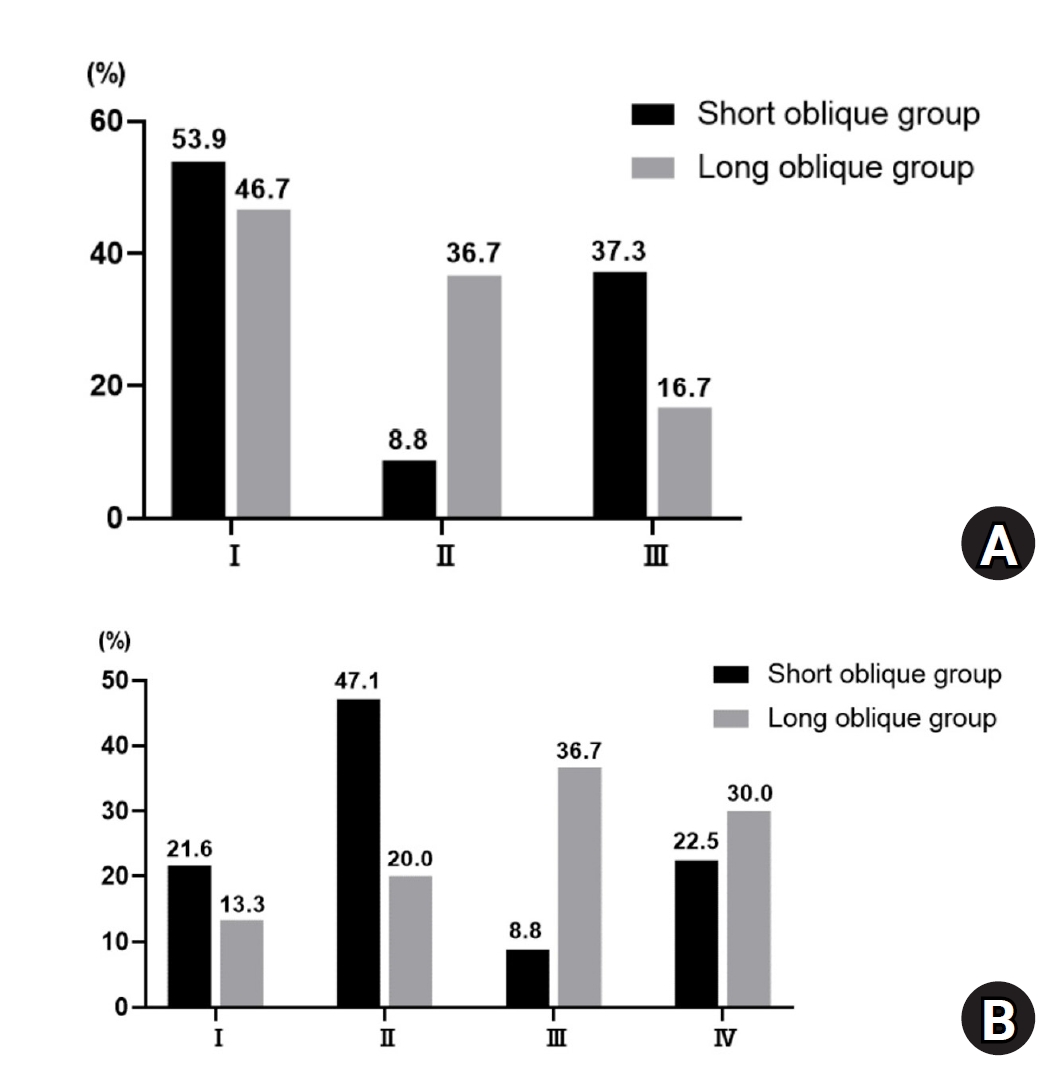
Fig. 6.Receiver operating characteristic curve of posterior cortex height for predicting ≥25% articular involvement of the posterior malleolar fragment. The area under the curve was 0.72, and the optimal cut-off value was 39.3 mm (sensitivity, 0.65; specificity, 0.80; Youden’s index, 0.45).
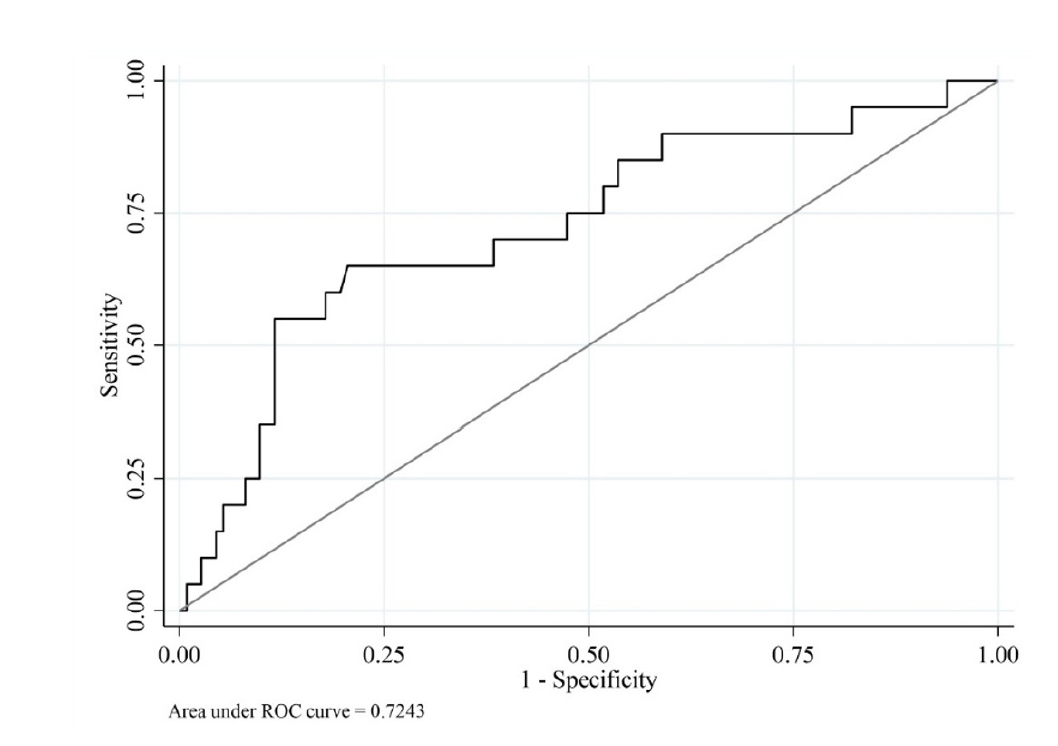
Table 1.Patient demographics and posterior malleolar fracture classification
|
Variable |
<4.5 cm group (n=102) |
≥4.5 cm group (n=30) |
P-valuea)
|
|
Age (yr) |
54.2±17.7 (18.0–86.0) |
43.2±19.5 (18.0–79.6) |
0.004 |
|
Sex |
|
|
0.058 |
|
Male |
37 (36.3) |
17 (56.7) |
|
|
Female |
65 (63.7) |
13 (43.3) |
|
|
Laterality, right:left |
53 (52.0):49 (48.0) |
14 (46.7):16 (53.3) |
0.680 |
|
BMI (kg/m2) |
24.7±3.1 (18.8–32.1) |
25.8±6.0 (21.6–34.1) |
0.083 |
|
Injury mechanism |
|
|
0.040 |
|
Ground level fall |
87 (85.3) |
20 (66.7) |
|
|
High-impact sports injury |
6 (5.9) |
6 (20.0) |
|
|
Fall from height (>1 m) |
3 (2.9) |
- |
|
|
Motor vehicle collision |
6 (5.9) |
4 (13.3) |
|
|
Follow-up duration (mo) |
19.5±12.0 (12.0–78.2) |
22.9±16.1 (12.0–72.0) |
0.293 |
Table 2.Comparison of radiographic outcomes between the <4.5 cm and ≥4.5 cm groups
|
Variable |
<4.5 cm group (n=102)
|
≥4.5 cm group (n=30)
|
P-valuea)
|
|
Crude |
Adjusted |
Crude |
Adjusted |
Independent t-test |
Multivariable analysis |
|
Lateral malleolar fracture |
|
|
|
|
|
|
|
Anterior height (mm) |
−1.1±4.7 |
−1.1±0.6 |
3.7±7.2 |
3.8±1.0 |
0.002 |
<0.001 |
|
Posterior height (mm) |
24.8±7.8 |
25.1±0.8 |
55.4±10.4 |
56.1±1.5 |
<0.001 |
<0.001 |
|
Fracture angle (°) |
38.1±9.1 |
37.8±0.8 |
20.5±3.8 |
21.4±1.5 |
<0.001 |
<0.001 |
|
Haraguchi classification |
|
|
|
|
<0.001 |
|
|
I |
55 (53.9) |
|
14 (46.7) |
|
|
|
|
II |
9 (8.8) |
|
11 (36.7) |
|
|
|
|
III |
38 (37.3) |
|
5 (16.7) |
|
|
|
|
Bartonicek classification |
|
|
|
|
<0.001 |
|
|
1 |
22 (21.6) |
|
4 (13.3) |
|
|
|
|
2 |
48 (47.1) |
|
6 (20.0) |
|
|
|
|
3 |
9 (8.8) |
|
11 (36.7) |
|
|
|
|
4 |
23 (22.5) |
|
9 (30.0) |
|
|
|
|
Posterior malleolar fracture |
|
|
|
|
|
|
|
Peak height (mm) |
15.2±8.7 |
15.2±0.9 |
21.0±9.1 |
21.0±1.6 |
0.002 |
0.003 |
|
Fragment area (mm2) |
140.7±99.5 |
140.0±10.2 |
242.2±122.2 |
244.6±19.5 |
<0.001 |
<0.001 |
|
Articular involvement (%) |
12.0±8.2 |
11.9±0.8 |
19.2±9.0 |
19.5±1.5 |
<0.001 |
<0.001 |
Table 3.ICCs for the interrater reliability of radiographic measurements
|
Interrater reliability |
ICC for agreement (95% CI) |
Category |
P-value |
|
Lateral malleolar fracture (n=132) |
|
|
|
Anterior height (mm) |
0.984 (0.977‒0.988) |
Excellent |
<0.001 |
|
Posterior height (mm) |
0.954 (0.935‒0.967) |
Excellent |
<0.001 |
|
Fracture angle (°) |
0.902 (0.864‒0.929) |
Excellent |
<0.001 |
|
Posterior malleolar fracture (n=132) |
|
|
|
Peak height (mm) |
0.888 (0.845‒0.919) |
Excellent |
<0.001 |
|
Fragment area (mm2) |
0.913 (0.879‒0.937) |
Excellent |
<0.001 |
|
Articular involvement (%) |
0.846 (0.784‒0.890) |
Excellent |
<0.001 |
References
- 1. Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures: an increasing problem. Acta Orthop Scand 1998;69:43-7.ArticlePubMed
- 2. Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma 1989;29:1565-70.
- 3. Berkes MB, Little MT, Lazaro LE, et al. Articular congruity is associated with short-term clinical outcomes of operatively treated SER IV ankle fractures. J Bone Joint Surg Am 2013;95:1769-75.Article
- 4. Bergman C, Morin M, Lawson K. Anatomy, classification, and management of ankle fractures involving the posterior malleolar fragment: a literature review. Foot Ankle Orthop 2019;4:2473011419887724.ArticlePubMedPMCPDF
- 5. Tosun B, Selek O, Gok U, Ceylan H. Posterior malleolus fractures in trimalleolar ankle fractures: malleolus versus transyndesmal fixation. Indian J Orthop 2018;52:309-14.ArticlePubMedPMCPDF
- 6. Macko VW, Matthews LS, Zwirkoski P, Goldstein SA. The joint-contact area of the ankle: the contribution of the posterior malleolus. J Bone Joint Surg Am 1991;73:347-51.Article
- 7. Lee GW, Jung DM, Kwak WK, Lee KB. Comparison of the size of the posterior malleolar fragment in trimalleolar ankle fractures measured using lateral plain radiography and three-dimensional computed tomography. J Korean Fract Soc 2022;35:91-6.ArticlePDF
- 8. Fitzpatrick DC, Otto JK, McKinley TO, Marsh JL, Brown TD. Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma 2004;18:271-8.ArticlePubMed
- 9. Hartford JM, Gorczyca JT, McNamara JL, Mayor MB. Tibiotalar contact area: contribution of posterior malleolus and deltoid ligament. Clin Orthop Relat Res 1995;(320):182-2.
- 10. Yuce A, Erkurt N, Yerli M, Saygili MS, Ozkan CB. Morphology of fibular incisura is a deciding factor between posterior malleolus avulsion fracture or syndesmotic ligament injury in ankle fractures. J Foot Ankle Surg 2024;63:18-21.
- 11. Blom RP, Meijer DT, de Muinck Keizer RO, et al. Posterior malleolar fracture morphology determines outcome in rotational type ankle fractures. Injury 2019;50:1392-7.Article
- 12. Mangnus L, Meijer DT, Stufkens SA, et al. Posterior malleolar fracture patterns. J Orthop Trauma 2015;29:428-35.ArticlePubMed
- 13. Yi Y, Chun DI, Won SH, Park S, Lee S, Cho J. Morphological characteristics of the posterior malleolar fragment according to ankle fracture patterns: a computed tomography-based study. BMC Musculoskelet Disord 2018;19:51.PubMedPMC
- 14. Patton BK, Orfield NJ, Clements JR. Does the Lauge-Hansen injury mechanism predict posterior malleolar fracture morphology. J Foot Ankle Surg 2022;61:1251-4.ArticlePubMed
- 15. Neumaier Probst E, Maas R, Meenen NM. Isolated fracture of the posterolateral tibial lip (Volkmann's triangle). Acta Radiol 1997;38:359-62.
- 16. Boden SD, Labropoulos PA, McCowin P, Lestini WF, Hurwitz SR. Mechanical considerations for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am 1989;71:1548-55.Article
- 17. Yamaguchi K, Martin CH, Boden SD, Labropoulos PA. Operative treatment of syndesmotic disruptions without use of a syndesmotic screw: a prospective clinical study. Foot Ankle Int 1994;15:407-14.ArticlePubMedPDF
- 18. Park CJ, Lee MS, Lee KB. Prediction of syndesmotic instability according to the lateral malleolus fracture pattern in supination-external rotation type ankle fractures: short oblique versus long oblique fracture. J Korean Fract Soc 2024;37:39-45.ArticlePDF
- 19. Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am 2006;88:1085-92.Article
- 20. Bartonicek J, Rammelt S, Kostlivy K, Vanecek V, Klika D, Tresl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 2015;135:505-16.
- 21. Terstegen J, Weel H, Frosch KH, Rolvien T, Schlickewei C, Mueller E. Classifications of posterior malleolar fractures: a systematic literature review. Arch Orthop Trauma Surg 2023;143:4181-220.ArticlePubMedPMCPDF
- 22. Briet JP, Houwert RM, Smeeing DP, et al. Differences in classification between mono- and polytrauma and low- and high-energy trauma patients with an ankle fracture: a retrospective cohort study. J Foot Ankle Surg 2017;56:793-6.ArticlePubMed
- 23. Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma 2002;53:55-60.Article
- 24. Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma 2010;69:666-9.ArticlePubMed
- 25. Weber M, Ganz R. Malunion following trimalleolar fracture with posterolateral subluxation of the talus--reconstruction including the posterior malleolus. Foot Ankle Int 2003;24:338-44.ArticlePubMedPDF
- 26. Solan MC, Sakellariou A. Posterior malleolus fractures: worth fixing. Bone Joint J 2017;99B:1413-9.PubMed
- 27. Rammelt S, Boszczyk A. Computed Tomography in the diagnosis and treatment of ankle fractures: a critical analysis review. JBJS Rev 2018;6:e7.Article
- 28. Büchler L, Tannast M, Bonel HM, Weber M. Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma 2009;23:208-12.PubMed
- 29. Meijer DT, Doornberg JN, Sierevelt IN, et al. Guesstimation of posterior malleolar fractures on lateral plain radiographs. Injury 2015;46:2024-9.PubMed
 , Chan-Jin Park1
, Chan-Jin Park1 , Jun-Young Lee2
, Jun-Young Lee2 , Keun-Bae Lee1,3
, Keun-Bae Lee1,3 , Gun-Woo Lee1,3
, Gun-Woo Lee1,3


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

