Comparison of Percutaneous versus Open Pedicle Screw Fixation for Treating Unstable Thoracolumbar Fractures
Article information
Abstract
Abstract
Purpose
This study compared the clinical and radiological results between two groups of patients with percutaneous fixation or conventional fixation after hardware removal.
Materials and Methods
The study analyzed 68 patients (43 open fixation and 43 percutaneous screw fixation [PSF] 25) who had undergone fixation for unstable thoracolumbar fractures. The radiologic results were obtained using the lateral radiographs taken before and after the fixation and at the time of hardware removal. The clinical results included the time of operation, blood loss, time to ambulation, duration of the hospital stay and the visual analogue scale.
Results
The percutaneous pedicle screw fixation (PPSF) group showed better results than did the conventional posterior fixation (CPF) group (p<0.05) in regard to the perioperative data such as operation time, blood loss, and duration of the hospital stay. There were no significant differences in wedge angle, local kyphotic angle, and the ΔKyphotic angle on the postoperative plane radiographs between the two groups (p>0.05). There were no significant differences in the wedge angle and local kyphotic angle after implant removal (p>0.05) between the two groups as well. However, there were significant differences in the segmental montion angle (p<0.001), and the PPSF group showed a larger segmental motion angle than did the CPF group (CPF 1.7°±1.2° vs PPSF 5.9°±3.2°, respectively).
Conclusion
For the treatment of unstable thoracolumbar fractures, the PPSF technique could achieve better clinical results and an improved segmental motion angle after implant removal within a year than that of the conventional fixation method.

Radiography showing linear and angular measurement. Wedge angle (∠AB°), local kyphotic angle (∠CD°), anterior body height (200× b/(a+c) %), posterior body height (200×e/(d+f) %).
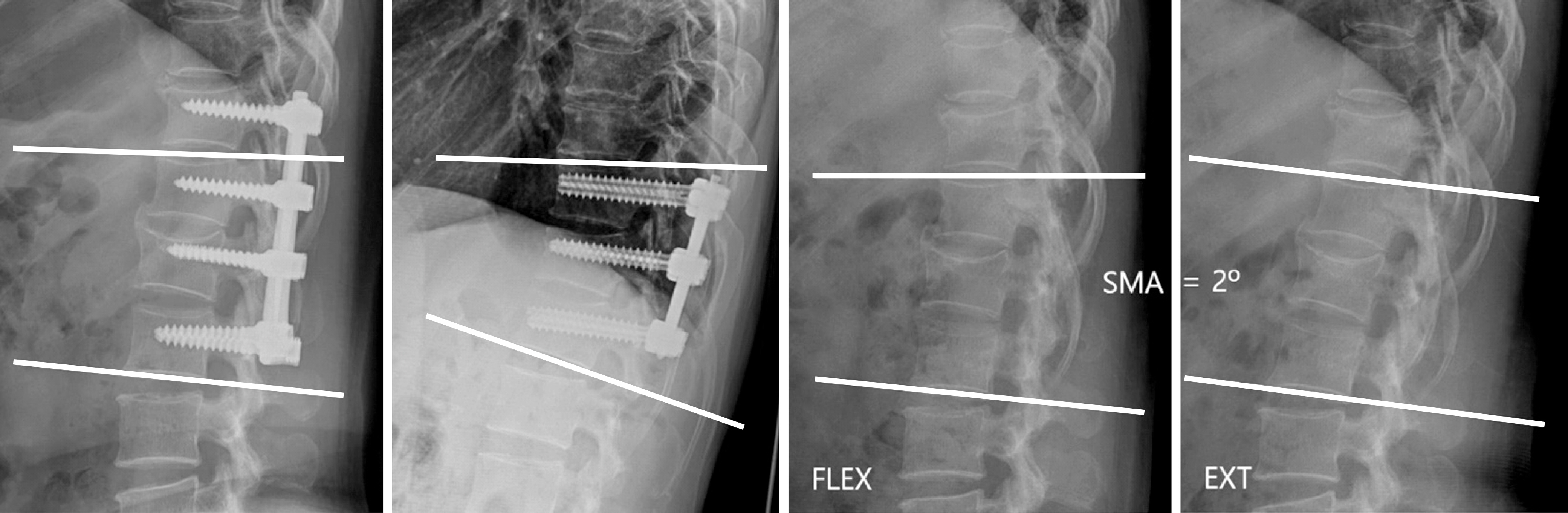
The segmental motion angle (SMA) was calculated as the difference between the local kyphotic angle on the flexion (FLEX) and extension (EXT) plain radiograph.
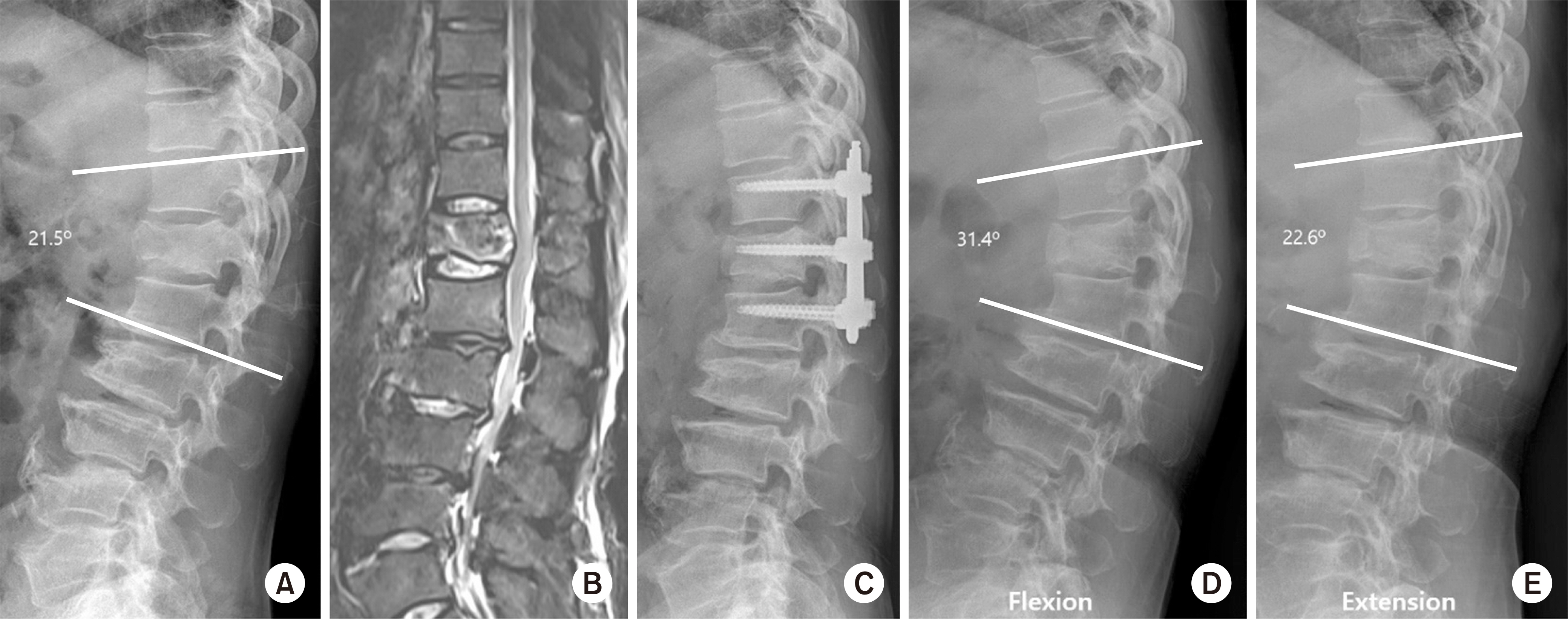
A 64-year-old male with flexion-distraction injury on T12. (A) The preoperative lateral X-ray shows fracture of the T12 body and spinous process. (B) On the magnetic resonance imaging (T2 weighted fat suppression), there was acute compression fracture with a spinous process fracture. (C) The lateral radiograph, taken immediately after surgery, shows anatomical reduction. (D, E) Lateral X-ray of the flexion (D)/extension (E) views that show the range of motion of no fusion segment.



