Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(3); 2020 > Article
- Original Article Clinical and Radiological Outcomes of Polished Cemented Bipolar Hemiarthroplasty for Intertrochanteric Fractures in Elderly Patients
- Suc-Hyun Kweon, Chang-Hyun Shin, Yeong-Chang Lee, Min-Woo Kim, Tae-Ho Kim
-
Journal of Musculoskeletal Trauma 2020;33(3):134-141.
DOI: https://doi.org/10.12671/jkfs.2020.33.3.134
Published online: July 31, 2020
2Department of Orthopedic Surgery, Presbyterian Medical Center, Jeonju, Korea
- 679 Views
- 4 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
To evaluate the clinical and radiological outcomes of bipolar hemiarthroplasty using a polished cemented femoral stem for intertrochanteric fractures in elderly patients.
Materials and Methods
From July 2005 to May 2015, 48 patients diagnosed with intertrochanteric fractures underwent bipolar hemiarthroplasty. The mean age and follow-up period were 80.5 years and 30.5 months, respectively. The postoperative results were evaluated clinically and radiologically.
Results
The mean operation time was 100 minutes (range, 90-120 minutes), and the mean amount of blood loss was 334 ml (range, 170-500 ml). At the last follow-up, the mean Harris hip score (HHS), visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores were 82.2 (range, 76-90), 0.8 (range, 1-3), and 36 (range, 30-40), respectively. Walking was initiated using a walker for partial weight-bearing, and the mean walking time was 5.8 days (range, 3-14 days). Ambulatory ability was restored to a walking state before the injury in 36 cases (75.0%), and wheelchair ambulation was possible in 12 cases (25.0%). The instrumental activities of daily living (IADLs) were 17 patients (35.4%), and the basic activities of daily living (BADLs) were 31 patients (64.6%).
Conclusion
Polished cemented bipolar hemiarthroplasty can achieve secure fixation with no postoperative thigh pain. Restoring the preoperative walking ability will be more helpful for intertrochanteric fractures in elderly patients.
Published online Jul 24, 2020.
https://doi.org/10.12671/jkfs.2020.33.3.134
Clinical and Radiological Outcomes of Polished Cemented Bipolar Hemiarthroplasty for Intertrochanteric Fractures in Elderly Patients
 , M.D.,
Chang-Hyun Shin
, M.D.,
Chang-Hyun Shin , M.D.,
Yeong-Chang Lee
, M.D.,
Yeong-Chang Lee , M.D.,
Min-Woo Kim
, M.D.,
Min-Woo Kim , M.D.,*
and Tae-Ho Kim
, M.D.,*
and Tae-Ho Kim , M.D.*
, M.D.*
Abstract
Purpose
To evaluate the clinical and radiological outcomes of bipolar hemiarthroplasty using a polished cemented femoral stem for intertrochanteric fractures in elderly patients.
Materials and Methods
From July 2005 to May 2015, 48 patients diagnosed with intertrochanteric fractures underwent bipolar hemiarthroplasty. The mean age and follow-up period were 80.5 years and 30.5 months, respectively. The postoperative results were evaluated clinically and radiologically.
Results
The mean operation time was 100 minutes (range, 90–120 minutes), and the mean amount of blood loss was 334 ml (range, 170–500 ml). At the last follow-up, the mean Harris hip score (HHS), visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores were 82.2 (range, 76–90), 0.8 (range, 1–3), and 36 (range, 30–40), respectively. Walking was initiated using a walker for partial weight-bearing, and the mean walking time was 5.8 days (range, 3–14 days). Ambulatory ability was restored to a walking state before the injury in 36 cases (75.0%), and wheelchair ambulation was possible in 12 cases (25.0%). The instrumental activities of daily living (IADLs) were 17 patients (35.4%), and the basic activities of daily living (BADLs) were 31 patients (64.6%).
Conclusion
Polished cemented bipolar hemiarthroplasty can achieve secure fixation with no postoperative thigh pain. Restoring the preoperative walking ability will be more helpful for intertrochanteric fractures in elderly patients.
Introduction
The goal of treatment of proximal hip fractures in elderly patients is to reduce complications that can occur in bed life by relieving pain and restoring preoperative walking ability through early walking and rehabilitation. Elderly patients often have poor bone quality due to osteoporosis; therefore, a reduction can be difficult, and concomitant complications such as nonunion, metal fixation failure, and lag screw perforation of the femoral head occur frequently.1) Bipolar hemiarthroplasty has disadvantages such as longer operation time and can result in more bleeding than internal fixation. However, there are limited implementations for early walking and return to daily life. Furthermore, there have been reports demonstrating the use of cementless femoral stems,2,3) but a firm fixation it is often difficult to obtain early, and many complications such as postoperative thigh pain or fractures around the stem are possible.4,5) The aim of this study was to evaluate the clinical and radiological results of bipolar hemiarthroplasty using polished cemented femoral stem in patients with intertrochanteric fractures.
Materials and Methods
1. Study subject
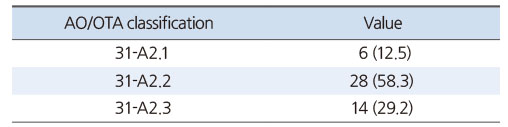
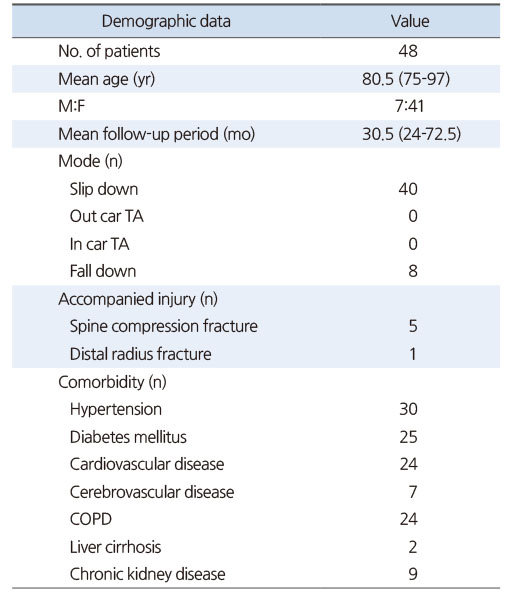
This study was approved by the local hospital ethics committee (No. 2019-08-008), and the informed consent was waived. From July 2005 to May 2015, Wonkwang University Hospital, among 238 patients with bipolar hemiarthroplasty who aged 75 years old or older and were diagnosed with intertrochanteric fracture of the femur classified by AO-Muller/Orthopaedic Trauma Association classification from 31-A2.1 to 31-A2.3, 52 patients were included who were able to walk outdoors without an assistive device. According to the AO classification, 31-A3 type fracture has the fracture line extending from the medial cortex to the cortical bone below the Greater Trochater (GT). So these type fractures were excluded from this study because they were not suitable for making GT as the landmark for lateralization of femoral components. Among them, 1 patient died during the follow-up period and 3 patients were not followed-up; therefore, a total of 48 cases were included who were followed-up for at least 2 years (Table 1). The study cohort included 41 females and 7 males with a mean age of 80.5 years (range, 75–97 years). The mean follow-up period was 30.5 months (range, 24–72.5 months). Of the 48 patients, 40 cases were occurred by slipping down and 8 cases by falling down, respectively. Concomitant injuries occurred in 5 cases of lumbar compression fracture and 1 case of distal radius fracture. Concomitant diseases included hypertension in 30 cases, diabetes in 25 cases, cardiovascular disease in 24 cases, cerebrovascular disease in 7 cases, chronic lung disease in 24 cases, liver cirrhosis in 2 cases, and chronic renal failure in 9 cases (Table 2).
Table 1
Classification of Intertrochanteric Fracture (n=48)
Table 2
Demographic Data
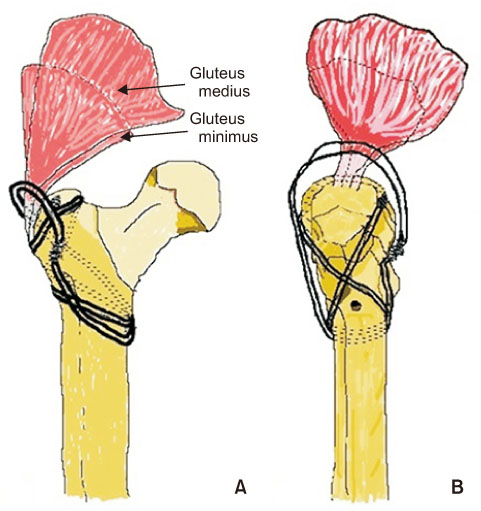
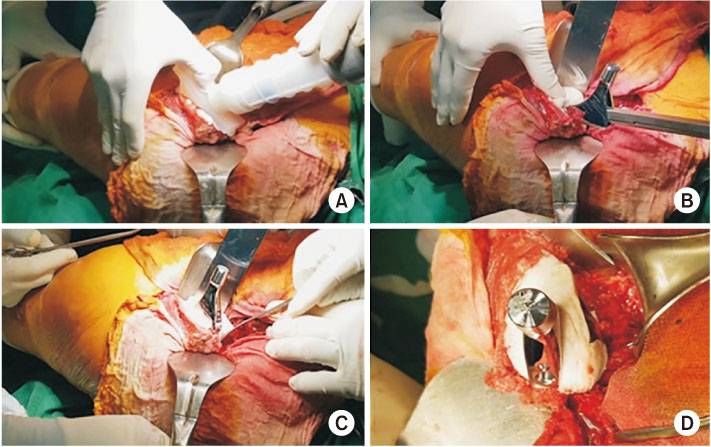
2. Surgical method
In all cases, the anterolateral approach (the modified Hardinge approach) was used. The femoral head was removed after cutting by oscillating saw along the intertrochanteric fracture while preserving the soft tissues around the exposed fracture area. Care was taken in the proximal femoral region, which is connected from the lesser trochanter to the greater trochanter, to avoid additional fractures because of the importance of maintaining the thickness of the proximal cement mantle. If the greater trochanteric fragments were displaced or additional fractures were existed, double loop wires were used to pass from the lesser trochanter to the greater trochanter to fix them firstly with figure eight shaped knot and then with an elliptical reinforcement (Fig. 1). In all cases, Cement was injected using the third-generation cement technique. In case of proximal femoral bone loss, an osteotome was placed around the bone defect to obtain an appropriate cement mantle thickness while maintaining the form (Fig. 2). After the cement was injected, pressure was applied using a proximal femoral sealing to distribute the cement evenly. Cement that flowed out of the form after the femoral stem was inserted was removed before hardening using a rongeur or thin osteotome. The degree of insertion of the femoral stem was determined by centering the three reference points on the femoral stem while maintaining a cement mantle thickness of at least 3 to 4 mm from the lesser trochanter up to 1 cm above. The femoral stem that extended with increased medial offset was used in all cases. Overall, 34 Exeter V40 (44 offset) cemented stems (Stryker, Mahwah, NJ, USA) and 14 collarless polished tapered (CPT) extended offset cemented stems (Zimmer, Warsaw, IN, USA) were used. Simplex (Stryker-Howmedica-Osteonics, Mahwah, NJ, USA) bone cement was used for the Exeter stem and CMW3 (Depuy, Warsaw, IN, USA) bone cement was used for the CPT stem.
Fig. 1
The 18 gauze wiring technique was used above the soft tissue on the trochanteric area with an eight-shape and second oval-shape. (A) Anteroposterior view. (B) Axial view.
Fig. 2
(A) Cement gun was used for retrograde insertion and pressurization. (B) Osteotome was positioned around the bone defect. (C, D) An appropriate cement mantle thickness was obtained while maintaining the form.
3. Methodsunstab
We encouraged patients to start the knee joint and Q-setting exercise 1 day postoperatively. Wheelchair ambulation or bed side standing was done at 4 to 5 days and walker ambulation at 6 to 7 days postoperatively, respectively. Patients with concomitant injuries and postoperative medical complications were treated with individualized rehabilitation method.
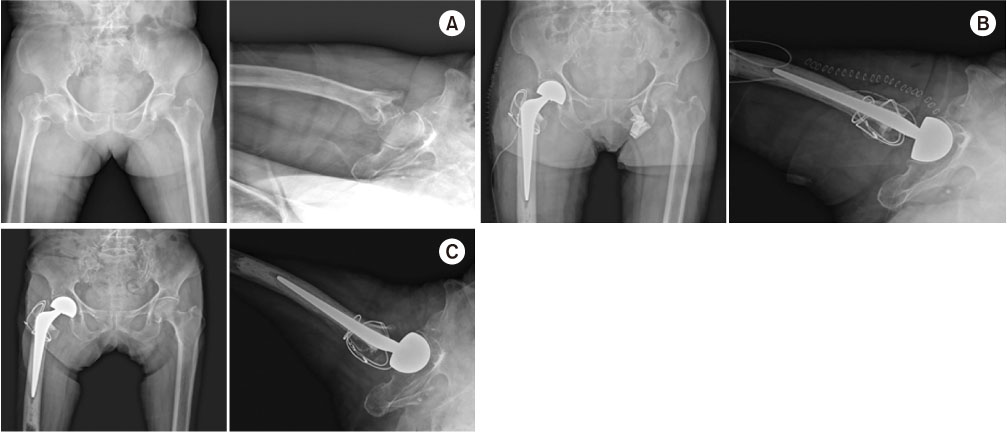
We used the Harris hip score (HHS), visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score for clinical evaluation. We assessed the degree of recovery to the ambulatory state before injury and postoperative total weight bearing time.6,7) We used anteroposterior and axial images for radiological evaluation of the hips at the time of operation and throughout the final follow-up (Fig. 3). Barrack classification was used for postoperative cementing technique evaluation to categorize the patients into four grades (Table 3).8)
Fig. 3
A 79-year-old female with an intertrochanteric fracture underwent bipolar hemiarthroplasty. (A) Preoperatively: anteroposterior and axial view. (B) Postoperatively: anteroposterior and axial view. (C) Two-year follow-up: anteroposterior and axial view.
Table 3
Barrack Classification of Cement Mantle Quality
We measured the vertical distance of the radiolucent line of the outer shoulder of the stem in zone 1 to assess subsidence of the femoral stem. When we could not measure this distance, the change in the distance between the end of the femoral stem and the lower part of the distal centralizer was assessed. As described previously by Gruen et al.,9) the femoral stem is divided into 7 zones for monitoring and a radiolucent line can be identified if the demarcation line of the bone cement and femoral stem is thicker than 2 mm.
Results
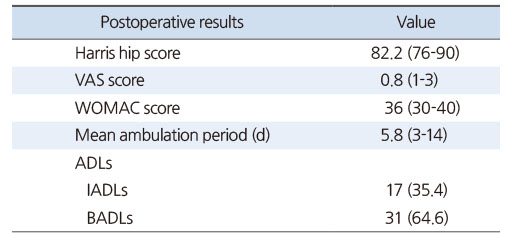
The mean operative time was 100 minutes (range, 90–120 minutes), and the mean blood loss was 334 ml (range, 170–500 ml). Systemic complications included pneumonia (3 cases), urinary tract infection (3 cases), and delirium (9 cases). There were no femoral pain or groin pain complaints and no postoperative dislocations in all cases. Superficial infection occurred in 3 patients; subsequently, 2 patients were treated with simple intravenous antibiotic therapy, and the remaining case was improved with marginal resection, implantation of antibiotic-embedded cement beads, and intravenous antibiotic therapy for 4 weeks. As a result of the clinical evaluation, the mean HHS was 82.2 (range, 76–90), the mean VAS was 0.8 (range, 1–3), and the WOMAC score was 36 (range, 30–40) at the last follow-up.
The gait was initiated using a walker to partially load weight, and the mean walking time was 5.8 days (range, 3–14 days). Walker ambulation was delayed in 2 patients with long-term pneumonia treatments and 6 patients with preoperative dementia. Walking ability recovered to preinjury state in 36 cases (75.0%), and 12 cases (25.0%) were able to be ambulated with wheelchairs. Instrumental activities of daily living (IADLs) were possible in 17 cases (35.4%), and basic activities of daily living (BADLs) were possible in 31 cases (64.6%) (Table 4).
Table 4
Postoperative Clinical Outcome (n=48)
In postoperative imaging, 30, 14, 4, and 0 patients were classified as grades A, B, C, and D, respectively, in a retrospective manner according to the Barrack classification. The mean subsidence of the femoral stem was 2.3 mm (range, 1–5 mm) at the final follow-up with no subsidence of bone cement in any case.
We did not find osteolysis and loosening of the femoral stem in any patient. Postoperative complications included fracture of the proximal part of the femoral stem due to slip down (1 patient, Vancouver type B). Proximal femoral stem fracture was managed with internal fixation using a metal plate without changing the femoral stem while maintaining the cement.
Discussion
Proximal femoral fractures in the elderly include severe osteoporotic comminuted fractures therefore, internal fixation can be difficult and complications such as nonunion and metal fixation failure can frequently occur.10) In addition, when internal fixation fails, the long bed life delays the return to normal life due to deterioration of systemic condition and muscle weakness, overall resulting in an increase in mortality rate. Treatment options should be based on the patient's general condition, the type of fracture, and the degree of osteoporosis. In elderly patients, bipolar hemiarthroplasty may be selected as an appropriate treatment option because it can reduce the complications associated with fractures and reduce systemic complications by allowing early ambulation and functional recovery.11,12) However, there has been debate over whether cementless or cemented stems are more appropriate for elderly patients. Many authors have reported no difference in mortality, functional outcomes, and reoperation rates between patients with cementless and cemented stems over long-term follow-up.13,14) Furthermore, it has been reported that the use of a cemented femoral stem may lead to complications such as increased bleeding, longer operation time, embolization, and decreased cardiac output during cement insertion.13) In this study, the mean intraoperative and postoperative transfusion volumes were 400 ml and 600 ml, respectively, and additional transfusion was performed only if the hemoglobin level was less than 7 g/dl. The operation time was delayed when the greater trochanteric bone was severely displaced and the double loop wire technique was used. In order to prevent embolism, the femoral cancellous bone was kept at its maximum, and the adipose tissue and cancellous bone were removed. After washing with 2 to 3 L of normal saline, gauze packing with hydrogen peroxide was used to prevent blood clots from remaining in the femur, and then cement was injected. Anesthesiologists need to pay close attention to prevent significant lowering of blood pressure during joint reduction after cement compression and femoral stem insertion. Choy et al.15) reported that 40 cementless Bipolar hemiarthroplasties with AML 5/8 porous-coated femoral stem (Depuy) for intertrochanteric fractures (A2 according to the AO classification) in elderly patients showed reasonable outcomes for more than 2 years of follow-up. The author emphasized the osteointegration rate in the diaphysis can be increased in osteoporotic elderly patients with pressfit fixation of implants. In this study, even though there was no radiologic complication, 7 patients (14.5%) and 5 patients (10.4%) complained of groin and thigh pain, respectively, requiring medication. Considering groin or thigh pain was not observed in our study, even if there is no particular problem in the surgical technique, the press-fit fixation of cementless arthroplasty itself can cause the pain.
Bipolar hemiarthroplasty in elderly patients has been performed for rapid recovery and functional needs.16,17) Firm fixation and less femoral pain are easy to obtain via cemented femoral stems, thus allowing for early wheelchair ambulation and standing after surgery while also being helpful for early rehabilitation treatment in elderly patients.18) Early treatment has also been reported to result in fewer complications and lower mortality.19) In this study, ambulation with a walker was performed on mean 4.5 days postoperatively. In cases of medical complications such as pneumonia or dementia, ambulation with walker was delayed. However, all patient began wheelchair ambulation three days after the operation.
In a proximal femoral fracture, a cemented femoral stem with a collar was used to distribute the pressure to the proximal bone and cement to prevent the femoral stem subsidence and to allow for the leg length to be set more easily.20) However, stress was applied to the proximal thigh, resulting in early dissociation of the femoral stem due to proximal femoral bone resorption and cement mantle fragment. Furthermore, when the varus position of the femoral stem is caused by a calcar pivot, the collar acts as a fulcrum, resulting in a femoral stem failure.9,21) However, this complication was reduced in the case of a polished cemented stem without collar when the proximal cement mantle thickness (3-4 mm proximal, 2 mm distal) is retained because hoop stress occurred on the cement-bone surface while the stem interlock within the cement mantle.22,23) In this study, we used a polished cemented stem without a collar in all cases. At the final follow-up, the mean femoral stem subsidence was 2.3 mm, and there was no osteolysis due to proximal femoral bone resorption and cement mantle fracture.
Because the gluteus medius and gluteus minimus, which are the abductors of the hip, are attached around the femur greater trochanter, rehabilitation is often delayed due to postoperative pain and tingling if there is no firm fixation. Various methods have been used to fix the greater trochanter. Grimsrud et al.24) reported that the standard cement femoral stem and the new cerclage cable technique in premature intertrochanteric fractures allow for early weight bearing and result in fewer complications. The double-stranded 18-gauge wire was used to fix the fractured trochanteric site first with a figure eight knot, and then fastened firmly in an elliptical shape once more to enable early walking.
Conclusion
In elderly patients with intertrochanteric fractures, bipolar hemiarthroplasty can be performed as an alternative to internal fixation, which has a high failure rate. The bipolar hemiarthroplasty using a polished cemented femoral stem, which is a third-generation cement technique, can be useful for early walking and restoration of preoperative gait due to earlier firm fixation and no thigh pain.
Financial support:This study was supported by grant from Wonkwang University, 2019.
Conflict of interests:None.
References
-
Tasyıkan L, Ugutmen E, Sanel S, Soylemez MS, Ozkan K, Solakoglu C. Short-term results of surgical treatment with cephalomedullary nails for basicervical proximal femoral fractures. Acta Orthop Belg 2015;81:427–434.
-
-
Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev 2010;16:CD001706
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

