Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 27(4); 2014 > Article
-
Original Article
- The Efficacy of Preserved Posterior Cortex in the Treatment of Infected Nonunion of the Tibia
- Hyoung-Min Kim, M.D., Il-Jung Park, M.D., Youn-Tae Roh, M.D., Byung-Min Kang, M.D., Hyun-Jin Lee, M.D., Jae-Young Lee, M.D.
-
Journal of the Korean Fracture Society 2014;27(4):301-307.
DOI: https://doi.org/10.12671/jkfs.2014.27.4.301
Published online: October 20, 2014
Department of Orthopedic Surgery, The Catholic University of Korea, Buchon St. Mary's Hospital, Bucheon, Korea.
- Address reprint requests to: Jae-Young Lee, M.D. Department of Orthopedic Surgery, The Catholic University of Korea, Buchon St. Mary's Hospital, 327 Sosa-ro, Wonmi-gu, Bucheon 420-717, Korea. Tel: 82-32-340-7099, Fax: 82-32-340-2671, osleejy@catholic.ac.kr
• Received: April 30, 2014 • Revised: June 22, 2014 • Accepted: August 28, 2014
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 468 Views
- 2 Download
Abstract
-
Purpose
- We studied the efficacy of preserved posterior cortex connecting to adjacent muscle or periosteum during wide debridement in the treatment of infected nonunion of the tibia.
-
Materials and Methods
- From January 2001 to May 2011, 12 cases of infected nonunion of the tibia with segmental defect larger than 4 cm after wide debridement were selected. The selected cases were categorized according to two groups; group 1 with preserved posterior cortex in the segmental defect site - six cases, group 2 without posterior cortex - six cases. The results were compared by assessing the size of bone defect, the interval between wide debridement and bone reconstruction, bony union time, complications, and clinical results.
-
Results
- The mean length of bone defect of group 1 was 7.6 cm (range 4.3-11.0 cm) and that of group 2 was 6.4 cm (range 4.0-12.0 cm). The interval between wide debridement and bone reconstruction was 10.0 weeks (range 5-18 weeks) for group 1, and 12.1 weeks (range 0-24 weeks) for group 2. The time for bony union of group 1 was 6.2 months (range 5-7 months), and that of group 2 was 10.8 months (range 7-18 months). In group 2, there were two cases of fatigue fracture and two cases of docking site nonunion after distraction osteogenesis.
-
Conclusion
- The preserved posterior cortex after wide debridement of infected nonunion of the tibia helps bony union and reduces the treatment period.
- 1. Kim HM, Kim YS, Chu IT, Choi MG, Cho YG. Free vascularized fibular graft for the treatment of the large bone defect. J Korean Orthop Assoc, 1995;30:1224-1231.ArticlePDF
- 2. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am, 1976;58:453-458.PubMed
- 3. Patzakis MJ, Abdollahi K, Sherman R, Holtom PD, Wilkins J. Treatment of chronic osteomyelitis with muscle flaps. Orthop Clin North Am, 1993;24:505-509.Article
- 4. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res, 1989;(243):36-40.Article
- 5. Damholt VV. Treatment of chronic osteomyelitis; a prospective study of 55 cases treated with radical surgery and primary wound closure. Acta Orthop Scand, 1982;53:715-720.Article
- 6. Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg, 2005;13:417-427.Article
- 7. Weiland AJ, Daniel RK. Microvascular anastomoses for bone grafts in the treatment of massive defects in bone. J Bone Joint Surg Am, 1979;61:98-104.Article
- 8. Vail TP, Urbaniak JR. Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg Am, 1996;78:204-211.Article
- 9. Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res, 1994;(301):111-117.Article
- 10. DeCoster TA, Gehlert RJ, Mikola EA, Pirela-Cruz MA. Management of posttraumatic segmental bone defects. J Am Acad Orthop Surg, 2004;12:28-38.Article
- 11. Christian EP, Bosse MJ, Robb G. Reconstruction of large diaphyseal defects, without free fibular transfer, in Grade-IIIB tibial fractures. J Bone Joint Surg Am, 1989;71:994-1004.Article
- 12. Reckling FW, Waters CH 3rd. Treatment of non-unions of fractures of the tibial diaphysis by posterolateral cortical cancellous bone-grafting. J Bone Joint Surg Am, 1980;62:936-941.
- 13. Simpson JM, Ebraheim NA, An HS, Jackson WT. Posterolateral bone graft of the tibia. Clin Orthop Relat Res, 1990;(251):200-206.
- 14. Song JM, Kim JI, Park JS, et al. A clinical study of free vascularized osteocutaneous fibular transplantation in infected nonunion of tibia. J Korean Soc Microsurg, 2000;9:27-36.
REFERENCES
Fig. 1A 62-year-old male with an open comminuted fracture showing a segmental defect of the left tibia and fibula. Infection developed after external and internal fixation with a vascularized fibular graft. (A) Approximately 10.0 cm sized segmental bone loss with soft tissue defect. (B) Preserved posterior cortex (arrow) after wide debridement of the infected bone. (C) Proximal tibia plating with autogenous cancellous iliac bone graft. (D) A successful union six months after autogenous cancellous iliac bone graft.
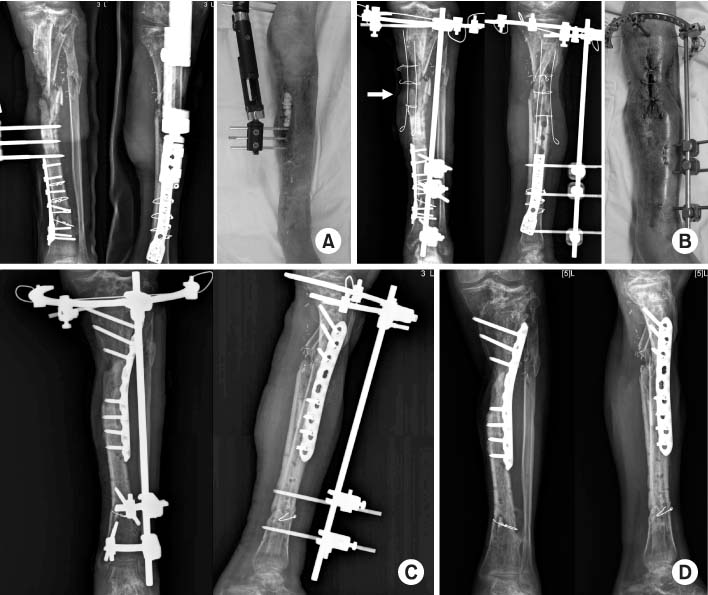
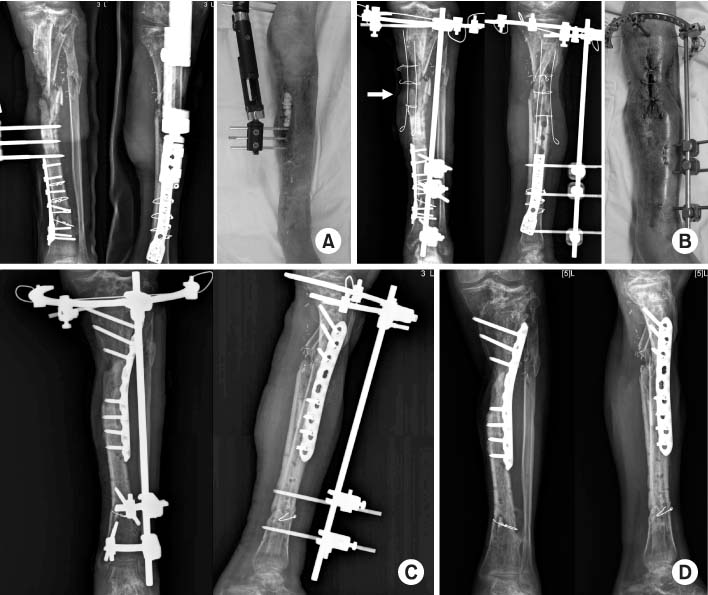
Fig. 2A 44-year-old male with a comminuted fracture of the right tibia and fibula. Infection developed after open reduction and internal fixation using plates. (A) Active draining nonunion with soft tissue defect. (B) Isolated healthy posterior cortex (arrow) is preserved after wide debridement. Approximately 11 cm sized segmental bone defect is noted. (C) Autogenous cancellous iliac bone graft and plating three months after wide debridement. (D) A successful union seven months after autogenous cancellous iliac bone graft.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

The Efficacy of Preserved Posterior Cortex in the Treatment of Infected Nonunion of the Tibia
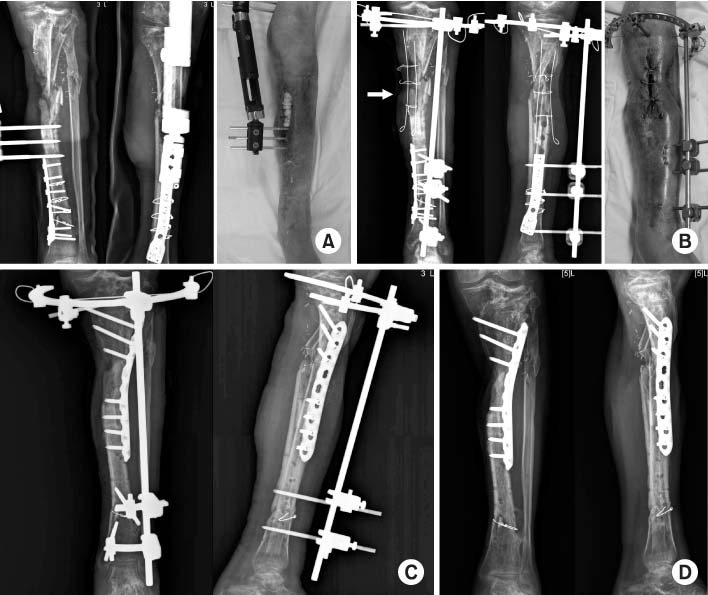

Fig. 1
A 62-year-old male with an open comminuted fracture showing a segmental defect of the left tibia and fibula. Infection developed after external and internal fixation with a vascularized fibular graft. (A) Approximately 10.0 cm sized segmental bone loss with soft tissue defect. (B) Preserved posterior cortex (arrow) after wide debridement of the infected bone. (C) Proximal tibia plating with autogenous cancellous iliac bone graft. (D) A successful union six months after autogenous cancellous iliac bone graft.
Fig. 2
A 44-year-old male with a comminuted fracture of the right tibia and fibula. Infection developed after open reduction and internal fixation using plates. (A) Active draining nonunion with soft tissue defect. (B) Isolated healthy posterior cortex (arrow) is preserved after wide debridement. Approximately 11 cm sized segmental bone defect is noted. (C) Autogenous cancellous iliac bone graft and plating three months after wide debridement. (D) A successful union seven months after autogenous cancellous iliac bone graft.
Fig. 1
Fig. 2
The Efficacy of Preserved Posterior Cortex in the Treatment of Infected Nonunion of the Tibia
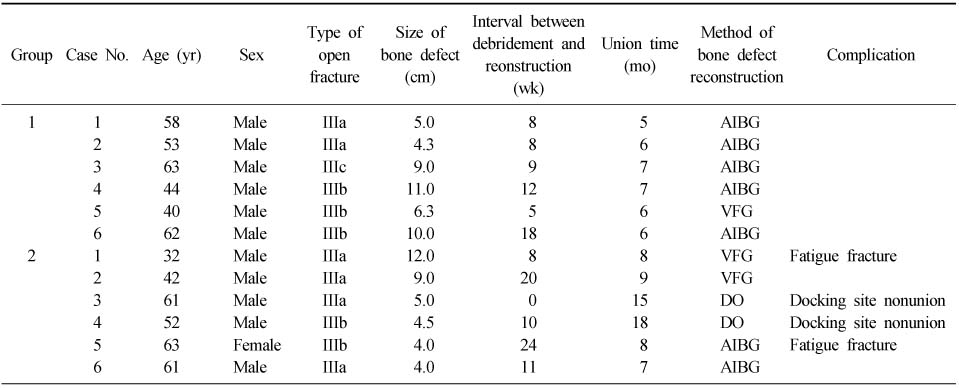
Summary of Cases
AIBG: Autogenous iliac bone graft, VFG: Vascularized fibular graft, DO: Distraction osteogenesis.
Table 1
Summary of Cases
AIBG: Autogenous iliac bone graft, VFG: Vascularized fibular graft, DO: Distraction osteogenesis.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

