Search
- Page Path
- HOME > Search
Original Articles
- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
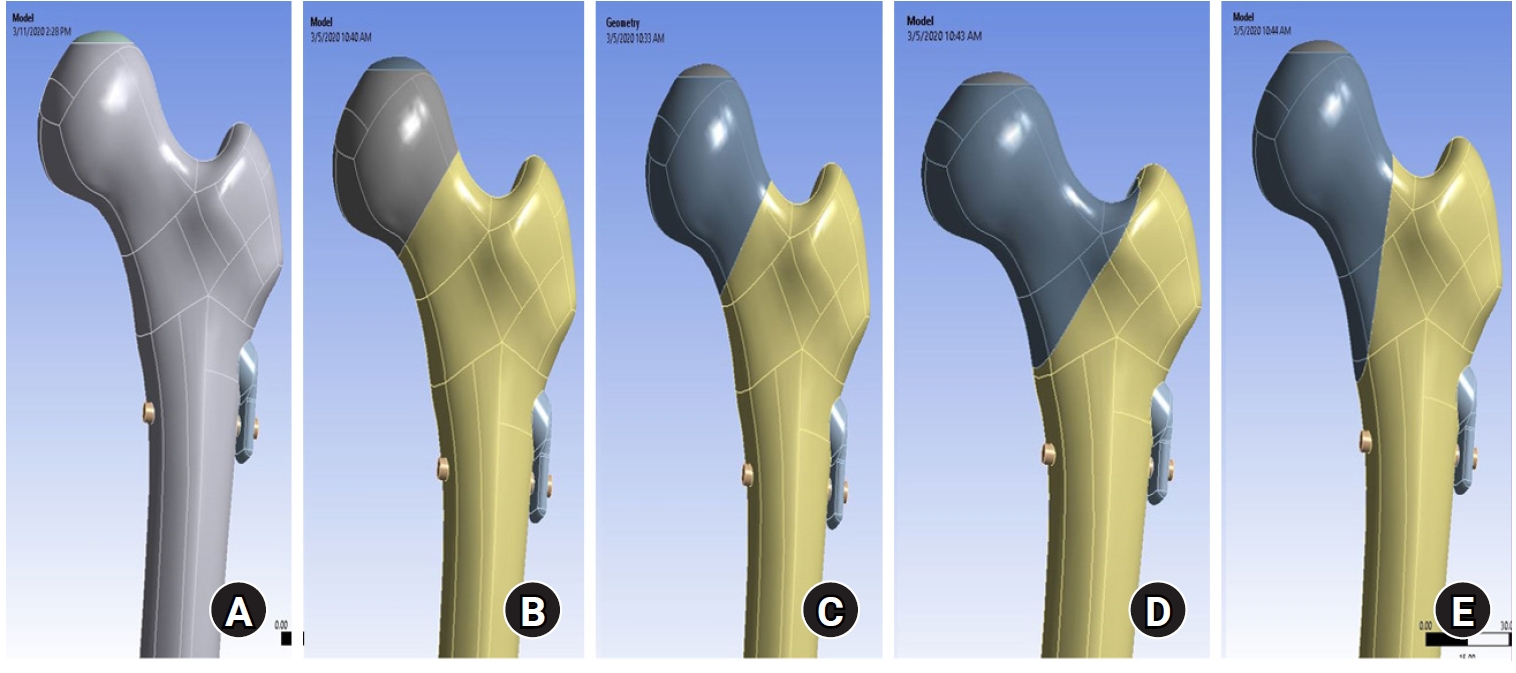
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV. -
Citations
Citations to this article as recorded by- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
Abdessamed Bachiri, Mustapha Amine Arab, Nadia Kadouri
Computer Methods in Biomechanics and Biomedical Engineering.2026; : 1. CrossRef
- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
- 1,927 View
- 82 Download
- 1 Crossref

- Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
- J Korean Fract Soc 2020;33(4):179-188. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 786 View
- 3 Download
- 1 Crossref

- Treatment of the Proximal Femoral Fractures with Proximal Femoral Nail Antirotation (PFNA)
- Myung Sik Park, Young Jin Lim, Young Sin Kim, Kyu Hyung Kim, Hong Man Cho
- J Korean Fract Soc 2009;22(2):91-97. Published online April 30, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.2.91
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the clinical and radiologic results of treatments in proximal femoral fracture with Proximal Femoral Nail-Antirotation (PFNA).
MATERIALS AND METHODS
We retrospectively reviewed the results of 21 cases of proximal femoral fracture treated with PFNA from September 2006 to October 2007 which could be followed up for minimum of more than a year. The mean age was 61.5 (20~88) years old. Male were involved in 12 cases, female in 9 cases. The mean follow up was 14.3 (12~18) months. The Garden alignment index, Cleveland index, tip apex distance were evaluated by post-operative radiologic evaluation and complications of bone union, failure of internal fixation and deformity were evaluated by follow up radiologic findings. Clinical results were assessed by social function score of Jensen and mobility score of Parker and Palmer at last follow up.
RESULTS
All fractures were united and the mean time to bone union was 15.7 (13~18) weeks. Garden alignment index showed good results of above 'good' in 15 cases (71.4%), Cleveland index showed 14 cases (66.4%) positioning in zone 5 and tip apex distance showed 17.81 (+/-5.65~27.52) mm in radiologic findings. The mean sliding of blade was 1.32 (0.34~2.94) mm in follow up radiologic findings and fracture of distal locking screw area was found in 1 case as a complication. Among 21 cases, the function before injury was completely recovered in 15 cases (71.4%) which were assessed by social function score of Jensen and 13 cases (61.9%) by mobility score of Parker and Palmer.
CONCLUSION
We think that PFNA is effective osteosynthetic device for proximal femur fracture with satisfactory radiologic and clinical outcomes. -
Citations
Citations to this article as recorded by- Clinical and radiological outcome of the Chimaera short nailing system in inter- and subtrochanteric fractures
Aurélien Traverso, Trieu-Hoai-Nam Ngo, Guillem Fernandez Gil, Xavier Lannes, Sylvain Steinmetz, Kevin Moerenhout
Injury.2023; 54(3): 970. CrossRef - Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
Jae-Cheon Sim, Tae-Ho Kim, Ki-Do Hong, Sung-Sik Ha, Jong-Seong Lee
Journal of the Korean Fracture Society.2013; 26(1): 37. CrossRef - The Treatment of Intertrochanteric Femoral Fracture with Proximal Femoral Nail Antirotation
Jong Won Kim, Hyun Soo Park, Young Soo Jang, Jae Hyuk Choi, Sung Ju Bae, Chan Il Bae
Journal of the Korean Fracture Society.2012; 25(4): 257. CrossRef - Cementless Bipolar Hemiarthroplasty Using a Rectangular Cross-section Stem for Type A2 or above Intertrochanteric Fractures
Bong-Ju Park, Hong-Man Cho, Cheol Park, Hwang-Se Bong
Hip & Pelvis.2012; 24(3): 222. CrossRef - Hip Arthroplasty for Failed Internal Fixation of Intertrochanteric Fractures
Ju-Oh Kim, Hong-Man Cho, Cheol Park, Ju-Hyun Sim
Hip & Pelvis.2012; 24(2): 94. CrossRef - Anatomical Measurement of Normal Korean Proximal Femur Using Plain Radiography: A Problem when using Proximal Femoral Nail Anti-rotation
Jong-Seok Park, Woo-Jong Kim, Jae-Wan Soh, Byung-Woong Jang, Tae-Heon Kim, You-Sung Suh
Hip & Pelvis.2011; 23(4): 303. CrossRef - The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
Journal of the Korean Fracture Society.2011; 24(3): 217. CrossRef - PFNA and PFN in Intertrochanteric Fractures - Comparison Study of Sliding -
Suk Kyu Choo, Hyoung Keun Oh, Jun Young Choi
Hip & Pelvis.2010; 22(1): 79. CrossRef - Proximal Femoral Nail Antirotation versus Compression Hip Screw with Trochanter Stabilizing Plate for Unstable Intertrochanteric Hip Fractures
Jae-Young Rho, Sang-Bum Kim, Youn-Moo Heo, Seong-Jin Cho, Dong-Sik Chae, Woo-Suk Lee
Journal of the Korean Fracture Society.2010; 23(2): 161. CrossRef - Treatment of the Unstable Intertrochanteric Fracture with Proximal Femoral Nail Antirotation: Comparison with Compression Hip Screw with Trochanteric Stabilizing Plate
Tae-Ho Kim, Jong-Oh Kim, Seung-Yup Lee, Geon-Ung Yun
Journal of the Korean Fracture Society.2010; 23(4): 353. CrossRef
- Clinical and radiological outcome of the Chimaera short nailing system in inter- and subtrochanteric fractures
- 1,115 View
- 3 Download
- 10 Crossref

- Structural Study of Proximal femur in the Elderly Femoral Neck & Trochanteric Fracture
- Byung Chul Park, Chang Wug Oh, Seung Hoon Oh
- J Korean Soc Fract 1998;11(1):175-180. Published online January 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.1.175
-
 Abstract
Abstract
 PDF
PDF - The factors that determine whether a proximal femoral fracture is neck or trochanteric area are a matter of controversy. So we studied the BMD(bone mineral density) and the morphology of the contralateral femur in subcapital fracture and intertrochanteric fracture(Boyd - Griffin Type I,II). The bone density of femoral neck, Ward's triangle and trochanteric region was measured by dual energy X-ray absortiometry(DEXA) in 41 patients with femoral neck fracture value and fracture type in same patients, we calculate the femoral neck length from the plain X-ray film. The results were as follows. 1. The ratio of BMD in the neck and trochanter area was higher in the trochanter fracture group. 2. The level of BMD of the trochanter fracture group was lower than the neck fracture group in all opints of measurement. 3. In the measurement of femoral neck length at plain X-ray film, the neck length of trochanter fracture group was longer than the neck fracture group. It may be that difference in BMD and femoral neck length is related to the site at which a proximal femoral fracture occurs.
- 385 View
- 0 Download

- Proximal Femral Fracture During Closed Intramedullary Interlocking Delta Nailing
- Phil Hyun Chung, Moon Jib Yoo, Suk Kang, Eung Nam Cha, Yong Min Kim, Jong Won Kim
- J Korean Soc Fract 1992;5(2):378-382. Published online November 30, 1992
- DOI: https://doi.org/10.12671/jksf.1992.5.2.378
-
 Abstract
Abstract
 PDF
PDF - Closed intramedullary nailing is a complex technique which usually requires fracture table and image intensifier, so that the patient and surgeon are exposed to the radiation. But this technique affords considerable advantages such as high rate of union, less infection rate and early weight bearing, etc. The main causes of failure or complication of this procedure are inapproprisate entry point and inadequate nail size. These are especially important problems in the patient who is femoral canal diameter is very small (8 or 9mm). The Delta femoral interlocking nails (diameter 10mm and 11mm)were devised for the femurs with narrow canal diameter. However, proximal portion of the Delta nail (about 7cm from the proximal end)is thick (diameter 13mm)to gain strength enough for holding the insertion device and fixation of the interlocking screws. If the insertion point is not correct or proximal reaming is inadequate, iatrogenic proximal femoral fracture may occur during final insertion of the nail. We experienced 2 cases of this complication during fixation of femoral shaft fractures using the Delta nails. We managed thls problem with hip spica cast immobilization in one case, and multiple pinning of femur neck in the other.
- 380 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


