Search
- Page Path
- HOME > Search
Review Article
- Easily missed nondisplaced fractures accompanying complete fractures in the lower extremity and pelvis: a narrative review
- Young-Chang Park
- J Musculoskelet Trauma 2025;38(1):5-12. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00017
-
 Abstract
Abstract
 PDF
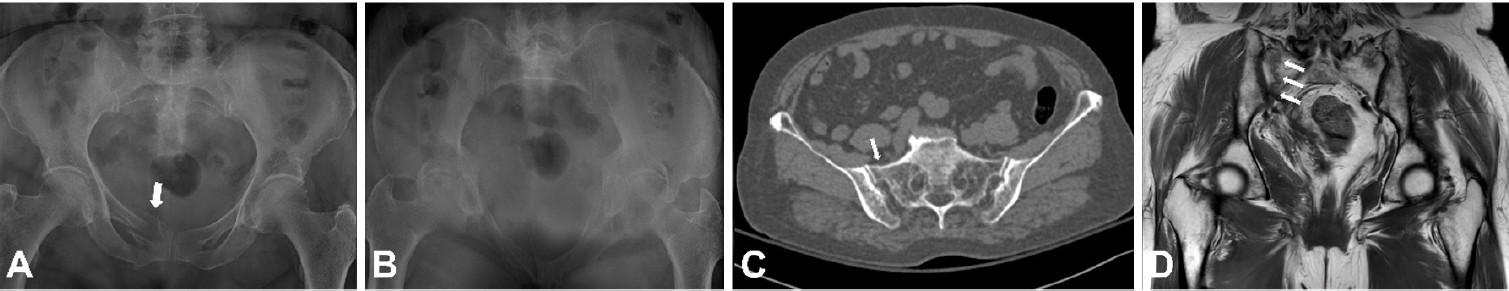
PDF - Nondisplaced fractures accompanying complete fractures are often difficult to detect on plain radiographs or computed tomography scans, posing a diagnostic challenge. The diagnosis of these frequently overlooked injuries can be delayed, potentially leading to suboptimal patient outcomes. This review discusses four commonly missed fracture patterns in the lower extremity and pelvis, including posterior involvement in fragility fractures of the pelvis, intertrochanteric extensions in isolated greater trochanter fractures, ipsilateral femoral neck fractures in high energy femoral shaft fractures, and posterior malleolar fractures in distal spiral tibial shaft fractures. An accurate diagnosis of these accompanying nondisplaced fractures is critical for optimizing surgical outcomes. Surgeons should incorporate thorough preoperative evaluations into their clinical practice to facilitate early detection and appropriate treatment strategies. Prompt identification and comprehensive management remain essential for improving patient outcomes.
- 1,376 View
- 47 Download

Original Article
- Surgical Treatment of Pediatric Intra-Articular Proximal Phalangeal Head Fracture of the Big Toe
- Yeun Soo Kim, Geunwu Gimm, Il ung Hwang, Goo Hyun Baek, Jihyeung Kim
- J Korean Fract Soc 2020;33(1):9-15. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.9
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Pediatric intra-articularproximal phalangeal head fractures of the big toe are very rare and few studies on this have been published. The purpose of this study is to present the diagnostic approach and surgical management of these extremely rare fractures, which might be easily underestimated or misdiagnosed.
MATERIALS AND METHODS
The study retrospectively reviewed all the patients who were diagnosed as intra-articular proximal phalangeal head fracture of the big toe and who underwent surgical intervention in our institution. The size of the bony fragment and hallux valgus interphalangeus angle were measured on the preoperative X-rays. The size and rotation of the osteochondral fragment, the presence of avascular necrosis, ligamentous injury and soft tissue entrapment were assessed on the preoperative magnetic resonance images (MRIs). The radiologic and functional evaluation were performed at 1 year postoperatively.
RESULTS
The average size of the bony fragments measured on the X-rays was 4.1 mm in width and 2.3 mm in length. Two cases showed hallux valgus interphalangeus. Preoperative MRI was performed in four cases and the average size of any osteochondral lesion was 5.3 mm in width, 3.9 mm in length, and 4.7 mm in height. Rotation of the osteochondral fragment was observed in one patient, and soft tissue entrapment was noted in two patients. Postoperatively, successful bony union was achieved in all the patients and the average time to union was 74.4 days.
CONCLUSION
Intra-articular proximal phalangeal head fractures of the big toe are very rare and often neglected due to incomplete ossification in the pediatric population. It is important to suspect the presence of this intra-articular fracture and to appropriately implement further evaluation. Nonunion of chronic cases as well as acute fractures can be successfully treated through open reduction and internal fixation using multiple K-wires.
- 1,000 View
- 10 Download

Case Report
- Pediatric Cartilaginous Tibia Eminence Fracture Overlooked on Plain Radiograph: A Report of Two Cases
- Seong Eun Byun, Yunseong Choi, Wonchul Choi
- J Korean Fract Soc 2017;30(1):29-34. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.29
-
 Abstract
Abstract
 PDF
PDF - In children with open physis, avulsion fracture of the tibia eminence, as an anterior cruciate ligament (ACL) injury, is more commonly observed than an ACL rupture. Pure cartilaginous avulsions of the ACL tibia insertion seldom occurs. In such case, cartilaginous lesion is frequently overlooked or misdiagnosed on plain radiograph and may result in a less favorable treatment outcome. We report two cases of cartilaginous tibia eminence fractures of the children that were initially overlooked from plain radiographs, and then diagnosed by magnetic resonance imaging, which was ultimately treated by arthroscopyassisted headless compression screw fixation.
- 495 View
- 4 Download

Original Articles
- MRI Findings of Posterior Ligament Complex Injury in Thorcolumbar Bursting Fractures
- Young Do Koh, Yeo Heon Yun, Hoon Jeong
- J Korean Soc Fract 2003;16(4):541-547. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.541
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the MR findings of structures injured in the burst fractures of thoracolumbar spine.
MATERIALS AND METHODS
Twenty-one patients who had thoracolumbar burst fractures with posterior ligament complex injury on MRI were studied. For the evaluation of stability of fractures, we used the scheme described by Oner et al. We identified the state of posterior ligament complex on surgery.
RESULTS
The MRI findings of ALL were state 1 in four, state 2 in fourteen, and state 3 in three. Those of PLL were state 1 in twelve, state 2 in six, and state 3 in three. The findings of posterior ligament complex were state 2 in one, state 3 in three, and state 4 in seventeen. The endplate state 1 was in four, state 2 in six, state 3 in seven, and state 4 in four. The disc state 1 was in twelve, state 2 in six, state 3 in two, state 4 in one. The vertebral body involvement state was 1 in four, state 2 in nine, and state 3 in eight. The injuries of posterior ligament complex were confirmed intraoperatively in all twenty-one patients.
CONCLUSION
We recommend the use of MRI to evaluate stability of fractures and state of posterior ligament complex in thoracolumbar burst fractures.
- 420 View
- 1 Download

- Insufficiency Fracture of the Sacrum: Report of two cases
- Young Kil Han, Young Su Jang
- J Korean Soc Fract 2000;13(4):749-753. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.749
-
 Abstract
Abstract
 PDF
PDF - Insufficiency fractures of the sacrum are rare but a distinct subgroup of pathologic fractures characterized by reduced osseous elastic resistance due to structural alterations of the bone. Stress fractures occurring in the settings have been defined as insufficiency fractures. Insufficiency fracture of the sacrum are difficult to diagnose, as plain radiographic findings are either unhelpful or misleadining. Bone scan is very sensitive and shows moderate to high uptake but the characteristic of H-shaped pattern of increased uptake of sacroiliac joint, specific for an insufficiency fracture, is only rarely seen. M.R.I is clearly the examination of choice, as it reveals early medullary edema and frequently a fracture line in a typical location. M.R.I helps in distinguishing tumoral disease from an insufficiency fracture. In this report, two cases of insufficiency fracture of the sacrum are discribed and compared with those previous studies.
- 347 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 First
First Prev
Prev


