Search
- Page Path
- HOME > Search
Review Article
- Treatment of avulsion fractures around the knee
- Jeong-Hyun Koh, Hyung Keun Song, Won-Tae Cho, Seungyeob Sakong, Sumin Lim
- J Musculoskelet Trauma 2025;38(2):63-73. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00073
-
 Abstract
Abstract
 PDF
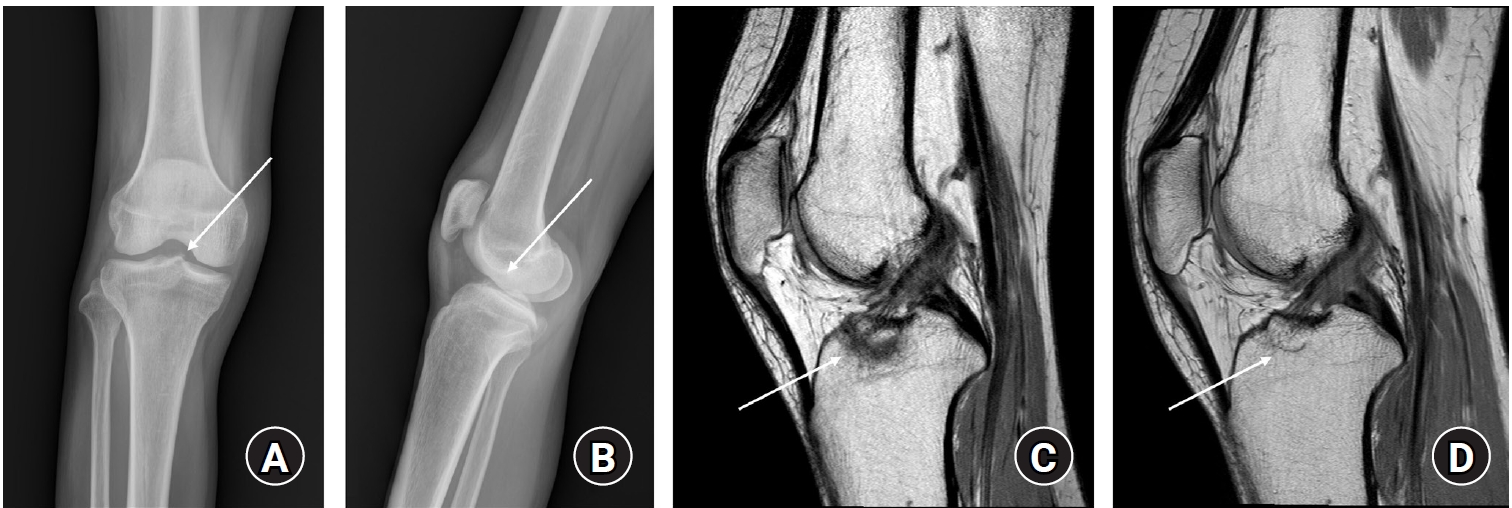
PDF - Avulsion fractures of the knee occur when tensile forces cause a bone fragment to separate at the site of soft tissue attachment. These injuries, which frequently affect adolescent athletes, can involve the cruciate and collateral ligaments, arcuate complex, iliotibial band, and patellar and quadriceps tendons. Radiographs aid in the initial diagnosis, while computed tomography and magnetic resonance imaging facilitate a comprehensive evaluation of injury severity and concomitant damage. Specific avulsion fracture types include: anterior cruciate ligament avulsions (tibial site, Meyers and McKeever classification), posterior cruciate ligament avulsions (tibial attachment, Griffith's classification), Segond fractures (anterolateral complex injury), iliotibial band avulsions, medial collateral ligament avulsions (reverse Segond, Stieda fractures), arcuate complex avulsions ("arcuate sign"), medial patellofemoral avulsions (patellar dislocations), and patellar/quadriceps tendon avulsions. The treatment depends on the fracture location, displacement, and associated injuries. Non-displaced fractures can be managed conservatively, while displaced fractures or those with instability require surgical reduction and fixation. Prompt recognition and appropriate intervention prevent complications such as deformity, nonunion, malunion, and residual instability. This review provides an overview of the pathogenesis, diagnosis, and management of knee avulsion fractures to guide clinical decision-making.
-
Citations
Citations to this article as recorded by- Lateral marginal fractures of the patella and patellofemoral pain
Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
Journal of Musculoskeletal Trauma.2025; 38(3): 152. CrossRef
- Lateral marginal fractures of the patella and patellofemoral pain
- 18,942 View
- 205 Download
- 1 Crossref

Original Article
- Clinical Outcomes of Triple Tension Band Wirings in Comminuted Patellar Fracture: A Comparison with Conventional Tension Band Wiring
- Hyun-Cheol Oh, Han-Kook Yoon, Joong-Won Ha, Sang Hoon Park, Sungwoo Lee
- J Korean Fract Soc 2024;37(2):82-86. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.82
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study devised triple tension band wirings (TTBW) fixation in patients with comminuted patella fractures to compare the clinical result of TTBW with that of tension band wiring (TBW).
Materials and Methods
This study was conducted on 91 patients who had undergone surgery diagnosed with acute patella fracture from January 2011 to December 2016. The study included 51 double TBW patients (Group 1) and 40 patients with TTBW (Group 2).
Results
Five out of 51 cases had a loss of reduction and fixation failure in Group 1, and no failure of fracture formation healing occurred in Group 2. Nonunion was noted in one case in Group 1 and no case in Group 2. Eight K-wire migration cases were observed in Group 1, which was not observed in Group 2. Six patients in Group 1 underwent revisional surgery. No patients in Group 2 had a reoperation. As a result of a one-year follow-up after the operation, the mean range of motion of the knee joint in groups 1 and 2 was 128.3°±11.3° and 127.9°±10.8°, respectively. The Lysholm’s scores for groups 1 and 2 were 90.8±4.2 and 90.3±3.8 points, respectively, which was not statistically significant.
Conclusion
TTBW is a helpful technique for the surgical treatment of comminuted patella fractures. The TTBW method has less reoperation due to nonunion and fixation failure. After a one-year followup, the clinical results were similar to the conventional TBW method. -
Citations
Citations to this article as recorded by- Lateral marginal fractures of the patella and patellofemoral pain
Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
Journal of Musculoskeletal Trauma.2025; 38(3): 152. CrossRef
- Lateral marginal fractures of the patella and patellofemoral pain
- 845 View
- 6 Download
- 1 Crossref

Review Article
- Treatment of Avulsion Fractures around the Knee
- Sumin Lim
- J Korean Fract Soc 2024;37(2):117-124. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.117
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures are common in athletes and result from high-impact or sudden, forceful movements involving the separation of a bone fragment at the ligament or tendon attachment site. The key focus areas include the anterior and posterior cruciate ligaments, medial collateral ligament, anterolateral complex, arcuate complex, medial patellofemoral ligament, patellar tendon, and quadriceps tendon. Diagnostic approaches combine radiography with advanced imaging techniques, such as computed tomography and magnetic resonance imaging, to elucidate the extent of injury and guide treatment decisions. Treatment ranges from conservative management for non-displaced fractures to surgical intervention for displaced fractures, with strategies customized based on the specific ligament involved and the nature of the fracture.
- 1,316 View
- 10 Download

Technical Note
- Operative Positioning Technique for an Intertrochanteric Fracture in a Patient with an Ipsilateral Above-the-Knee Amputation - Technical Note -
- Dae-Hyun Park, Yong-Uk Kwon, Dong-Seok Kim
- J Korean Fract Soc 2021;34(4):137-141. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.137
-
 Abstract
Abstract
 PDF
PDF - A 45-year-old man with a remote history of a left above-the-knee amputation presented to the emergency department with left hip pain after a mechanical fall. This case was an operative challenge because commonly used intraoperative traction methods could not be applied to a patient with an above-the-knee amputation. We describe a rarely utilized surgical technique of applying traction to an amputated extremity via a Steinmann pin during closed reduction and internal fixation of an intertrochanteric fracture.
-
Citations
Citations to this article as recorded by- Periprosthetic Femur Fractures in Osseointegration Amputees
Jason Shih Hoellwarth, S. Robert Rozbruch
JBJS Case Connector.2022;[Epub] CrossRef
- Periprosthetic Femur Fractures in Osseointegration Amputees
- 807 View
- 2 Download
- 1 Crossref

Review Article
- Periprosthetic Fractures following Total Knee Arthroplasty
- Byung Hoon Lee, Jae Ang Sim
- J Korean Fract Soc 2020;33(1):52-61. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.52
-
 Abstract
Abstract
 PDF
PDF - Recently, as the elderly population increases, the incidence of total knee arthroplasty has increased, with a concomitant increase in the frequency of periprosthetic fractures. To determine the treatment plan for fractures, the treatment method should be determined by the patient's age, osteoporosis, fixation status of the implant, and type of fracture. In recent years, operative treatment with reduction and stable fixation, rather than non-operative treatment, was used to promote early joint movement and gait. On the other hand, it is necessary to select an appropriate operative method to reduce complications of surgery, such as nonunion and infection, and expect a good prognosis. In this review, periprosthetic fractures were divided into femur, tibia, and patella fractures, and their causes, risk factors, classification, and treatment are discussed.
- 1,007 View
- 20 Download

Case Report
- Cortical Perforation Misidentified with Medial Condylar Fracture of Femur in Total Knee Arthroplasty: Case Report
- Seung Suk Seo, Sang Won Moon
- J Korean Fract Soc 2019;32(1):52-55. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.52
-
 Abstract
Abstract
 PDF
PDF - Intraoperative fracture in total knee arthroplasty (TKA) is a rare complication. However, when it happens, additional surgery to fix the fracture site is needed. Therefore, it is important to diagnose intraoperative fractures in TKA exactly. The authors experienced two cases of cortical perforation of medial femoral condyle misidentified as the fracture in TKA. Cortical perforation could be misdiagnosed as the fracture, which could lead to unnecessary surgery. This is the first report about cortical perforation in TKA. We report two cases of intraoperative cortical perforations and describe the radiological characteristics.
- 665 View
- 1 Download

Original Articles
- Arthroscopic Assisted Intra-Articular Reduction and Internal Fixation of Tibia Plateau Fracture
- Dong Hwi Kim, Gwang Chul Lee, Kwi Youn Choi, Sung Won Cho, Sang Ho Ha
- J Korean Fract Soc 2013;26(3):191-198. Published online July 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.3.191
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We evaluated the results of arthroscopic intra-articular reduction and internal fixation of tibial plateau fractures without cortical window along with any additional bone grafts.
MATERIALS AND METHODS
From March 2006 to March 2009, twelve patients with arthroscopic intra-articular reduction and internal fixation of tibial plateau fractures over 5 mm in depression and displacement on the articular surface in computed tomography (CT) were enrolled in this study. We reduced or removed the depressed fracture fragment using freer without making a cortical window. Then, we accomplished internal fixation by a cannulated screw. All cases have not received bone graft. Both the postoperative clinical and radiological results were evaluated by the Rasmussen system.
RESULTS
The fractures were healed completely in an average of 9 (range from 7 to 12) weeks. According to Rasmussen classification, we obtained satisfactory clinical results as excellent in 8 cases, good in 3 cases, and fair in 1 case; and radiological results were excellent in 7 cases and good in 5 cases.
CONCLUSION
We consider that arthroscopic intra-articular reduction and internal fixation of tibial plateau fractures without cortical window and any additional bone grafts is are a useful methods for attaining satisfactory results. -
Citations
Citations to this article as recorded by- Current Concepts in Management of Tibia Plateau Fracture
Sang Hak Lee, Kang-Il Kim
Journal of the Korean Fracture Society.2014; 27(3): 245. CrossRef
- Current Concepts in Management of Tibia Plateau Fracture
- 604 View
- 4 Download
- 1 Crossref

- Comparison of Floating Knee according to Presence of Knee Joint Injury
- Eau Sup Chung, Jong Hyuk Park, Hee Rack Choi, Joo Hong Lee, Kwang Bok Lee
- J Korean Fract Soc 2012;25(4):277-282. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.277
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the clinical outcomes of floating knee according to the presence of knee joint injury.
MATERIALS AND METHODS
Between March 2004 and March 2009, we investigated 36 patients, who underwent surgical treatment for floating knee injuries. We classified the floating knee into two groups as type I (12 cases) has no knee joint injury and type II (24 cases) has knee joint injury. We compared two groups about combined injury (orthopedics or other part), open fracture or not, neurovascular injury,union time, range of motion, and complication rate.
RESULTS
There is statistically no significant difference between two groups as type I (6 cases, 50%) and type II (13 cases, 54.2%) in orthopedic combined injury (p=0.813), and also same as type I (3 cases, 25%) and type II (12 cases, 50%) in combined injury on the other department (p=0.151), and in floating knee with open fracture as 4 type I (33%) and 12 type II (50%) of 16 cases (44%), and Gustilo-Anderson 3 type I, 4 type II, 1 IIIA, 4 IIIB, and 4 IIIC (p=0.423). There is statistically no significant difference between two groups in neurovascular injury as 1 type I (8.3%), and 3 type II (12.5%) (p=0.708). There is a statistically significant difference between two groups in the mean bone union time as 18.2+/-5.37 weeks (12~24 weeks) for type I and 24.95+/-9.85 weeks (16~33 weeks) for type II (p=0.045), and in the mean range of knee joint motion as 133+/-12.74 degree (120~150 degree) for type I and 105+/-19.00 degree (80~135 degree) for type II (p=0.012).
CONCLUSION
Floating knee with knee joint injury is severe itself and related with severe combined injuries, subsequent range of knee joint motion limitation, the delay of union time, and high complication rate. Therefore, we should take care in surgical treatment for this trauma entity.
- 397 View
- 0 Download

Case Report
- Combined Ipsilateral Fracture and Dislocation of Hip, Knee and Foot Joints: A Case Report
- Hyoung Soo Kim, Ju Hak Kim, Sang Joon Park, Jae Won Hyung
- J Korean Fract Soc 2012;25(1):73-76. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.73
-
 Abstract
Abstract
 PDF
PDF - Although clinical cases of ipsilateral knee and hip joint dislocation have been reported, there are no reports of simultaneous ipsilateral hip, knee, and foot dislocations. We report here a case of a patient who had ipsilateral hip, knee, and foot joint dislocations, and review the relevant literature.
- 512 View
- 3 Download

Original Articles
- Risk Factors of Periprosthetic Fracture after Total Knee Arthroplasty
- Ju Young Shin, Hyung Jun Kim, Seung Han Cha, Dong Heon Kim
- J Korean Fract Soc 2012;25(1):1-7. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the incidence rate and risk factors for periprosthetic fracture after total knee replacement (TKR).
MATERIALS AND METHODS
We carried out a retrospective case-control study of 596 patients (951 knees) who underwent TKR between 1999 and 2006 and who were followed up over 36 months. We classified patients into group I (study group) and group II (control group). We subdivided risk factors as pre-operative, intra-operative, and post-operative factors. Age, osteoporosis, revision arthroplasty, CVA, and alcohol dependence were categorized as pre-operative factors; anterior femoral notching and prosthetic types (mobile, fixed, and load-bearing) were considered intra-operative factors; and post-operative activity level was classified as a post-operative factor. We obtained information from the patients' charts, X-ray film, and telephone interviews.
RESULTS
The overall incidence rate was 2.25%; 3 patients were male, and 18 were female (14.28% and 85.72%, respectively). Old age (p<0.01, odds ratio=1.14), osteoporosis (p=0.01, odds ratio=4.74), revision arthroplasty (p=0.01, odds ratio=7.46), CVA (p=0.02, odds ratio=8.55), and alcohol dependence (p=0.03, odds ratio=44.54) were statistically significant among the pre-operative factors. Among the intra-operative factors, anterior femoral notching (p<0.01, odds ratio=11.74) was significant, and continued heavy labor (p<0.01, odds ratio=8.14) was significant among the post-operative factors.
CONCLUSION
We concluded that old age, osteoporosis, revision arthroplasty, comorbidity related with falling down, anterior femoral notching, and continued heavy labor were associated with periprosthetic fracture after TKR.
- 548 View
- 2 Download

- Anterior Knee Pain after Intramedullary Nailing for Tibial Shaft Fractures
- Suk Kyu Choo, Hyoung Keun Oh, Hyun Woo Choi, Jae Gwang Song
- J Korean Fract Soc 2011;24(1):28-32. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.28
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the possible causes and incidence of the chronic anterior knee pain follow after closed intramedullary nailing for the tibial shaft fractures, in a retrospective aspect.
MATERIALS AND METHODS
52 patients who treated with intramedullary nailing for the tibial shaft fractures from January 2001 to October 2008 were reviewed. We analyzed the relationship between knee pain and the variables (sex, age, types of fracture, protrusion extent of intramedullary nailing on proximal tibia). The aspects of pain, its onset and relieving time, and how much it influences on daily living were analyzed retrospectively. For categorical variables, group variences were estimated using Chi-square test.
RESULTS
34 patients of 52 (65%) complaint of anterior knee pain followed after intramedullary nailing, and there were no statistical differences between pain and sex/age (p>0.05). Incidence of anterior knee pain becomes higher as the severity of fracture increases, but there was no statistical difference between pain and intramedullary nailing protrusion. Pain severity was mostly not influencing on daily living, and it mostly responded to conservative treatment.
CONCLUSION
The incidence of anterior knee pain followed after intramedullary nailing was 65%, and its severity was mostly not influencing on daily living. There were no significant differences between pain and sex, age, protrusion extent of intramedullary nailing on proximal tibia, but as the severity of frature increases, the incidence of anterior knee pain became higher. -
Citations
Citations to this article as recorded by- Pain in Anterior Knee after Locked Nailing of Diaphyseal Tibia Fractures
V. V. Pisarev
Traumatology and Orthopedics of Russia.2020; 26(1): 85. CrossRef - Stress fractures of the tibia
Jung Min Park, Ki Sun Sung
Arthroscopy and Orthopedic Sports Medicine.2015; 2(2): 95. CrossRef - Tension Band Plating for a Stress Fracture of the Anterior Tibial Cortex in a Basketball Player - A Case Report -
Chul Hyun Park, Woo Chun Lee
Journal of the Korean Fracture Society.2012; 25(4): 323. CrossRef
- Pain in Anterior Knee after Locked Nailing of Diaphyseal Tibia Fractures
- 1,400 View
- 3 Download
- 3 Crossref

- The Use of Fresh Frozen Allogenic Bone Graft in the Impacted Tibial Plateau Fractures
- Yeung Jin Kim, Soo Uk Chae, Jung Hwan Yang, Ji Wan Lee, Dae Han Wi, Duk Hwa Choi
- J Korean Fract Soc 2010;23(1):26-33. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.26
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the behaviour of fresh frozen cancellous allograft used for supporting the reconstructed articular surface in impacted tibial plateau fractures.
MATERIALS AND METHODS
Between May 2004 and May 2008, 13 cases of impacted tibial plateau fracture were evaluated retrospectively. All fractures were treated with open reduction-internal fixation after restoration of the tibial plateau surface and insertion of fresh frozen cancellous allograft chips for subchondral support. Mean age was 46.6 (31~65) years. Average follow-up period was 36 (13~58) months. The radiological and clinical result for every patient was assessed according to the modified Rasmussen's system and Lysholm's knee score.
RESULTS
According to last follow-up weight bearing A-P X-ray, the fresh frozen cancellous allograft incorporated soundly in all cases and no complications such as joint depression, fracture reduction loss, angular deformity, and malunion were found. The mean time to complete bone union was postoperative 10+/-0.7 weeks. The mean range of motion was 135 (115~145) degrees. The mean Rasmussen's radiological score at last follow up was 15.3 (10 cases: excellent, 3 cases: good). The mean Lysholm's knee score at last follow up was 88.2+/-4.3.
CONCLUSION
We concluded that fresh frozen cancellous allograft in impacted tibial plateau fractures showed good results in terms of bone union and functional improvement and was considered to be a good structural supporter. -
Citations
Citations to this article as recorded by- Autograft versus allograft reconstruction of acute tibial plateau fractures: a comparative study of complications and outcome
Abolfazl Bagherifard, Hassan Ghandhari, Mahmoud Jabalameli, Mohammad Rahbar, Hosseinali Hadi, Mehdi Moayedfar, Mohammadreza Minatour Sajadi, Alireza Karimpour
European Journal of Orthopaedic Surgery & Traumatology.2017; 27(5): 665. CrossRef - Treatment of Tibial Plateau Fractures Using a Locking Plate and Minimally Invasive Percutaneous Osteosynthesis Technique
Hee-Gon Park, Dae-Hee Lee, Kyung Joon Lee
Journal of the Korean Fracture Society.2012; 25(2): 110. CrossRef
- Autograft versus allograft reconstruction of acute tibial plateau fractures: a comparative study of complications and outcome
- 729 View
- 2 Download
- 2 Crossref

Case Report
- Patient Accompanied with Simultaneous Anterior Dislocation of Hip and Anterior Dislocation of Knee : A Case Report
- Hee Gon Park
- J Korean Fract Soc 2009;22(3):185-188. Published online July 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.3.185
-
 Abstract
Abstract
 PDF
PDF - We are reporting a case that a 61-year-old patient who had simultaneous anterior dislocation of left hip and anterior dislocation of right knee after fall from a height injury was treated by closed reduction respectively.
-
Citations
Citations to this article as recorded by- Combined Ipsilateral Fracture and Dislocation of Hip, Knee and Foot Joints - A Case Report -
Hyoung-Soo Kim, Ju-Hak Kim, Sang-Joon Park, Jae-Won Hyung
Journal of the Korean Fracture Society.2012; 25(1): 73. CrossRef
- Combined Ipsilateral Fracture and Dislocation of Hip, Knee and Foot Joints - A Case Report -
- 590 View
- 1 Download
- 1 Crossref

Original Article
- Retrograde Nailing for Supracondylar Fracture after Total Knee Replacement: The Compatibility of Femoral Implant with Supracondylar Nail
- Moon Jib Yoo, You Jin Kim, Jin Won Lee
- J Korean Fract Soc 2008;21(1):19-23. Published online January 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.1.19
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Retrograde intrameullary nail is one of the treatment of periprosthetic supracondylar femoral fracture after total knee replacement (TKR), but all TKRs will not permit to insert a supracondylar nail. Therefore, we have investigated the compatibility of the TKRs with supracondylar nail.
MATERIALS AND METHODS
Using trial femoral component of the 5 used TKRs in Korea and saw bone model, we checked their compatibility and measured the dimensions of the intercondylar notches in both cruciate retaining (CR) and posterior stabilized (PS) type.
RESULTS
Although most CR prostheses had an intercondylar notch large enough to accept a supracondylar nail, in some case, this was not possible due to the notch being situated too far posteriorly. The position of the intercondylar notch is also important factor in the PS prostheses.
CONCLUSION
The notch position, rather than the notch size, was the most important factor in determining nail compatibility with femoral stem.
- 678 View
- 19 Download

Case Report
- Stiff Knee by Entrapment of Quadriceps Femoris Tendon at Fracture Site in Paediatric Distal Femur Shaft Fracture
- Suk Kang, Jong Pil Kim, Chung Soo Hwang, Phil Hyun Chung, Young Sung Kim, Sang Ho Lee, Jin Wook Chung
- J Korean Fract Soc 2007;20(4):339-344. Published online October 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.4.339
-
 Abstract
Abstract
 PDF
PDF - The complications following paediatric femur fracture are leg length discrepancy, angulation deformity, rotational deformity, ischemic limb. But, stiff knee is rarely expressed after trauma like paediatric femur fracture. We report a case of stiff knee due to entrapment of quadriceps femoris tendon at displaced fracture site after conservative treatment by Russel traction and hip spica cast in paediatric femur fracture. We treated successfully by resection of distal end of proximal segment of femur and release of quadriceps femoris tendon for flexion contracture of the knee.
- 376 View
- 0 Download

Original Articles
- Midterm Results of Treatment with a Retrograde Nail for Periprosthetic Fractures of the Femur Following Total Knee Arthroplasty
- Kyung Taek Kim, Jin Hun Kang, Lih Wang, Jae Sung Hwang
- J Korean Fract Soc 2007;20(4):309-314. Published online October 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.4.309
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the midterm results of the treatment with a retrograde nail for periprosthetic fractures of the femur following total knee arthroplasty.
MATERIALS AND METHODS
Between Jan 1998 and Jan 2004, 11 cases in 11 patients were treated for the periprosthetic fractures following total knee arthroplasty. The mean follow-up was 42.0 (30~98) months and the mean age was 66.0 (57~79) years old. 2 were males and 9 patients were females. In all cases, retrograde nailing was done for the periprosthetic fractures. Postoperative range of motion, HSS knee rating score, femorotibial angle, the time required for union, complications were evaluated.
RESULTS
Postoperative range of motion was 103.6° degrees on an average, HSS knee rating score was 83.5 points on an average at the last follow up. The mean angulation on radiograph was valgus 6.3°. The mean time required for union was 4 months. One had a newly fracture line at proximal part of supracondylar fracture, but there was no significant in clinical course. There was no prostheses required revision.
CONCLUSION
It appears that retrograde nail is a reliable surgical technique for periprosthetic fractures of the femur following total knee arthroplasty with low complication rate. The midterm results in our study showed that none of the prostheses required revision.
- 549 View
- 1 Download

- Effect of Alternative Splinting at Extension and 90degrees Flexion on Range of Motion after Open Reduction and Internal Fixation of Distal Femur Fracture
- Chong Kwan Kim, Jong Ho Yoon, Byung Woo Ahn, Chin Woo Jin, Dong Wook Kim, Young Il Kwan, Young Ho Lee
- J Korean Fract Soc 2005;18(2):144-148. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.144
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of early range of motion exercise by using 90degrees knee flexion splint after open reduction and internal fixation in fracture of distal femur.
MATERIALS AND METHODS
We reviewed twenty-six cases of distal femur fractures which were treated with open reduction and internal fixation from February 2002 to November 2003. One group (group A) were treated by using 30degrees knee flexion splint, the other group (group B) were treated by using 90degrees flexion and full extension splint alternativley by post-operative 1 week. The follow up period was minimally 12 months. The range of motion and Schatzker and Lambert criteria were evaluated.
RESULTS
The mean period to gain 90degrees knee flexion was 11.4 (7~14) weeks in group A, and 6.6 (3~8) weeks in group B. Mean range of motion was 94.7degrees (average flexion contracture 9.5degrees ) in A group and 108.7degrees (average flexion contracture 6.3degrees ) in B group at 12 weeks follow-up. According to Schatzker and Lambert criteria, excellent result was achieved in 10 cases (38%), good result in 13 cases (50%), fair result in 3 cases (12%).
CONCLUSION
This study demonstrates that alternative splinting at extension and 90degrees flexion contribute to early recovery of range of motion in distal femur fractures treated with internal fixation. -
Citations
Citations to this article as recorded by- Treatment of Femur Supracondylar Fracture with Locking Compression Plate
Seong Ho Bae, Seung Han Cha, Jeung Tak Suh
Journal of the Korean Fracture Society.2010; 23(3): 282. CrossRef
- Treatment of Femur Supracondylar Fracture with Locking Compression Plate
- 610 View
- 4 Download
- 1 Crossref

- Instability of Knee Associated with Ipsilateral Femoral and Tibial Shaft Fractures
- Whan Yong Chung, Woo Suk Lee, Woo Sik Kim, Yong Chan Kim, Taek Soo Jeon, Sun Hong Kim, Ji Hyuk Lim, Young Su Lim
- J Korean Fract Soc 2005;18(2):136-143. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.136
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To establish the incidence, type and significance of knee instability in patients with ipsilateral femoral and tibial shaft fracture, comparing with the patients with femoral shaft or tibial shaft fracture alone.
MATERIALS AND METHODS
Two hundreds and seventy-nine consecutive patients were retrospectively reviewed from February 2000 to April 2004. They were composed of 80 patients with femoral shaft fracture alone, 176 patients with tibial shaft fracture alone and 23 patient with ipsilateral femoral and tibial shaft fracture. We evaluate the instability of knee based on physical examinations, plain stress films and MRI. We analyze incidence and period to diagnosis of instability, period to complete bony union and Hospital for Special Surgery (HSS) knee score respectively.
RESULTS
There were 6.3% of knee instability in femoral shaft fracture alone, 9.7% in tibial shaft fracture alone and 30.4% in ipsilateral femoral and tibial shaft fracture. The average period to diagnosis of instability, average period to complete bony union and average HSS knee score were 9.2 months, 4.7 months and 65 points in femoral shaft fracture alone, 9.1 months, 4.2 months and 69 points in tibial shaft fracture alone, 8.7 months, 5.3 months (femur), 4.7 months (tibia) and 57 points in ipsilateral femoral and tibial shaft fracture respectively.
CONCLUSION
We should consider MRI to evaluate the knee instability in patient with ipsilateral femoral and tibial shaft fracture at the time of injury and make a plan early about the treatment of knee instability.
- 404 View
- 2 Download

- Management of Ipsilateral Femur and Tibia Fractures, with Retrograde and Antegrade Nailings from the Knee
- Chang Wug Oh, Jong Keon Oh, Woo Kie Min, In Ho Jeon, Hyung Soo Ahn, Hee Soo Kyung, Poong Taek Kim, Jung Ho Noh
- J Korean Fract Soc 2005;18(2):131-135. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.131
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To review the results in the management of ipsilateral femur and tibia fractures, using femoral and tibial intramedullary nailings with single incision on the knee.
MATERIALS AND METHODS
We treated 19 cases of ipsilateral femur and tibia fractures (floating knee), and the retrograde femoral nailing and antegrade tibial nailing were done with single incision on the knee. Except one patient of early death, 18 patients were included in this study. The mean age of index procedure was 34.1 years, and all of them had follow-up study for a mean of 2.4 years. The mean injury severity score was 18.8, and 12 patients had other fractures in the lower extremity.
RESULTS
Primary union was achieved in all, but one patient of femur and two of tibia. The average period for union was 27.6 weeks for femur and 24.5 weeks for tibia. One femoral nonunion occurred due to the metal failure after using short nail, and two tibial nonunion were caused by the bone loss with open tibial fractures. Most patients showed no limitation in knee motion. According to Karlstrom-Olerud criteria, functional results showed 14 excellent, 3 good and 1 acceptable. The protrusion of nail tip into the knee joint made the acceptable result with moderate limitation of knee motion, but it improved after the removal of nail.
CONCLUSION
CONCLUSION: Simultaneous retrograde femoral and antegrade tibial nailing with single incision on the knee, with an appropriate technique, can achieve the satisfactory result in the management of the ipsilateral femur and tibia fractures. -
Citations
Citations to this article as recorded by- Ipsilateral Femoral Segmental and Tibial Fractures: A Case Report
Oog Jin Sohn, Chul Hyun Park, Sang Keun Bae
Journal of the Korean Fracture Society.2009; 22(3): 193. CrossRef
- Ipsilateral Femoral Segmental and Tibial Fractures: A Case Report
- 661 View
- 5 Download
- 1 Crossref

Case Report
- Femoral Neck Fracture in Bilateral Above Knee Amputee: A Case Report
- Kye Young Han
- J Korean Soc Fract 2003;16(1):116-119. Published online January 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.1.116
-
 Abstract
Abstract
 PDF
PDF - Femoral neck fracture is a common fracture in elderly or osteoporotic women. But femoral neck fracture in previously amputed patients is rare, so the guideline of appropriate treatment is rarely discussed. Especially, femoral neck fracture in patients with above knee amputation was more rare. Hereby I report a case of femoral neck fracture occurred to 58-year-old male bilateral above knee amputee with the review of literatures.
- 398 View
- 2 Download

Original Articles
- Knee Pain Analysis After Tibia Intramedullary Nailing
- Kwang Won Lee, Jong Won Kang, Seung Hun Lee, Ha Yong Kim, Won Sik Choy
- J Korean Soc Fract 2001;14(2):278-284. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.278
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the incidence and clinical and radiological results of anterior knee pain following tibial intramedullary nailing.
MATERIALS AND METHODS
From January 1995 to April 1999, we retrospectively analyzed in 122 patients with tibial fracture who were treated by closed intramedullary nailing. All of 125 cases analyzed the age and sex distribution, mechanism of injury, fracture morphology, relationship of nail position on radiographs to knee pain and relationship of knee pain to the incision methods of patella tendon. Anterior knee pain was assessed with a 10-point analogue scale. Statistical analysis was performed using paired T-test.
RESULTS
At a mean follow-up period of thirty-eight months(12-64 months), sixtynine( 56%) patients(70 of 125 knees) had developed anterior knee pain. Insertion of the nail through the patella tendon splitting incision was associated with a higher incidence of knee pain compared to the paratendon site of nail insertion(62% and 35% respectively). According to the radiological analysis, the mean extent of nail protrusion of 122 patients was -1.4mm and the average nail protrusion of 69 patients with knee pain was 1.3mm respectively. Nail removal resolved or improved the symptoms in 69%.
CONCLUSION
Based on these data, we would recommend a parapatella tendon incision for nail insertion, and nail removal for those patients with a painful knee after bony union. -
Citations
Citations to this article as recorded by- Alteration of the Patella Tendon Length after Intramedullary Nail in Tibial Shaft Fractures
Dong-Eun Shin, Ki-Shik Nam, Jin-Young Bang, Ji-Hoon Chang
Journal of the Korean Fracture Society.2012; 25(4): 283. CrossRef - Anterior Knee Pain after Intramedullary Nailing for Tibial Shaft Fractures
Suk-Kyu Choo, Hyoung-Keun Oh, Hyun-Woo Choi, Jae-Gwang Song
Journal of the Korean Fracture Society.2011; 24(1): 28. CrossRef
- Alteration of the Patella Tendon Length after Intramedullary Nail in Tibial Shaft Fractures
- 821 View
- 2 Download
- 2 Crossref

- Popliteal Artery Injury Associated with Fracture and/or Dislocation of the Knee
- Jun Young Yang, Kwang Jin Rhee, June Kyu Lee, Deuk Soo Hwang, Ki Yong Byun, Taek Soo Jeon
- J Korean Soc Fract 2000;13(3):494-500. Published online July 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.3.494
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the outcome in patients who have popliteal artery injury associated with fracture and/or dislocation around the knee according to treatment option.
MATERIALS AND METHODS
We have reviewed fourteen cases of popliteal artery injury patients associated with fracture and/or dislocation injury around the knee who had visited at Chungnam National University Hospital from April 1997 to July 1999.
RESULTS
Combined skeletal injuries included fracture of distal femur, fracture of proximal tibia, and dislocation of the knee. Internal or external fixation was applied for skeletal injuries. We repaired the injured popliteal artery using end-to-end anastomosis (3 cases), interposed saphenous vein graft (9 cases), prosthetic vein graft (1 case), or thrombectomy alone (1 case). The amputation rate was 21 % (3 out of 14 patients). In limb salvage cases, we evaluated the function of knee joint, and the results were as follows : good 5 cases, fair 3 cases, and poor 3 cases.
CONCLUSION
Early diagnosis and prompt management for injuries of the popliteal artery is the most important factor to save the limb. Also, complete resection of all injured portion of vessel and reconstruction of patency through interposed saphenous vein graft are most useful method.
- 462 View
- 0 Download

- Delayed Diagnosed Thrombosis Associated with Closed Fractures Around the Knee
- Byung Moon Park, Hyung Koo Yoon, Kwang Pyo Jeon, Kyung Hoom Kang, Jin Il Kim, Dong Soo Kim, Yong Jae Lee
- J Korean Soc Fract 2000;13(2):289-295. Published online April 30, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.2.289
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
: The goal of this study is to decrease the chance of the lower limb loss resulting from the delayed diagnosis of arterial thrombosis after first operation in a patient of the closed fractures around the knee by early diagnosis and proper management via studying several prognostic factors.
MATERIALS AND METHODS
: We have reviewed 8 cases of delayed diagnosed arterial thrombosis patient who was follow up for 1 year or more March 1987 to February 1997, retrospectively. We have followed ip the clinical results.
RESULTS
: The amputation rate was 50%(4/8), and among associated injuries, tibial or peroneal nerve palsy was combined in 75%(6/8). The time interval from initial trauma to diagnosis was significantly different between amputation group(77hours) and non amputation group(34.25hours). Better results were obtained in cases who had early diagnosis and treated with end to end anastomosis than vein graft.
CONCLUSION
: It is very important that the vascular status should be assessed not only at the first examination but also repeatedly over the ensuing hours and days with caution, even though there was absence of ischemic sign.
- 374 View
- 0 Download

- Knee Fractures and Ligament Injuries Associated with Ipsilateral Femoral Shaft Fractures: Mechanism of Injury, Site of th Knee Fracture and Ligament Injury
- Dong Ju Chae, Phyl Hyun Chung, Won Suk Chae
- J Korean Soc Fract 2000;13(2):230-235. Published online April 30, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.2.230
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
: To establish the incidence and type of knee fractures, injury of knee ligament associated with ipsilateral femoral shaft fractures. What is the most common mechanism of these combined injuries? MATERIALS AND METHODS : From March 1995 to February 1999, evaluation of one hundred and twenty consecutive patients with fracture of the femoral shaft showed fractures and injuries of the ligaments of the ipsilateral knee in thirty-five(29%) of them. Of those thirty-five, nineteen patients had injured their knees and femoral shaft fractures by the dashboard injury. Twelve injuries were caused in a motor cycle accident, and two patients occurred in pedestrians struck by cars. Two injuries were caused by falls.
RESULTS
: There were twenty fractures of th knee and fifteen injuries of the ligament. Seventeen of the twenty fractures were in the patella, two in the bicondyle of the proximal tibia and one in the lateral condyle of the proximal tibia. Eleven of seventeen fractures of the patella were open fractures. Of fifteen injuries of the ligament, there were six posterior cruciate ligament tears (including 2 partial tears and 1 avulsion fracture), three posterior cruciate ligament tears with medial or lateral collateral ligament disruption , three anterior cruciate ligament tears(2 tibial spine fractures and 1 partial tear), two lateral collateral ligament disruptions and one medial collateral ligament tear. The locations of femoral shaft fracture were proximal in four patients, middle in thirty, and distal in one patient.
CONCLUSION
: We conclude that there is a high incidence of ipsilateral fracture of the patella and posterior cruciate ligament tears in patients with femoral shaft fractures. The dashboard injury is the most common mechanism of the ipsilateral knee fractures and ligament tears with femoral shaft fractures.
- 423 View
- 2 Download

- Results of Judet Quadricepsplasty in Knee Stiffness
- Kuhn Sung Whang, Ki Chul Park, Kyung Sik Kim
- J Korean Soc Fract 2000;13(1):96-102. Published online January 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.1.96
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
: We performed this study to evaluate the proper indication and complication of the Judet quadricepsplasty in the stiff knee.
MATERIALS AND METHODS
: Authors analyzed 15 cases in 14 patients treated by Judet quadricepsplasty from July 1990 to may 1998. There were 9 male and 5 female with an average age of 32.0 years. The average follow-up was 3 years 7 months. Causes of stiff knee sere femoral distal fracture in 7 cases, femoral midshaft fracture in 5 cases, tuberculosis osteomyelitis in 3 cases. The average interval between injury and quadricepsplasty was 1 year 10 months. We check the preoperative and last follow up range of motion in involved knee, and check the postoperative and last follow up extension lag and complication.
RESULTS
: By the Judet' classification, last follow up results were shown to be 5 cases in excellent, 5 cases in good, 5 cases in poor. Complications were patella fracture in 3 cases, infection in 1 case, femoral artery rupture in 1 case, and these 5 cases were shown to be poor results. Three patella fractures were arisen at the insertion of Quadriceps muscle. Infection was secondary type by the hematoma results from inappropriate hemostasis. Femoral artery rupture was arisen by the severe fibrosis at the surrounding arteries and tissues results from chronic infection due to long term application of Ilizarov apparatus. In the excellent and good results, average preoperative range of motion were 36.0 degrees, average last follow up range of motion were 96..5 degrees, average flexion gain were 60.5 degrees. Postperative extension lag were 16.5 degrees in 7 cases(70%), but last follow up extension lag were 8.7 degrees in 4 cases(40%).
CONCLUSION
: Judet quadricepsplasty was excellent method to solve the extra-articular stiff knee in the proper indication. Inappropriate indication were thought to severe intra-articular adhesion, severe osteoporosis of patella, severe fibrosis in the medial aspect of distal thigh. Postoperative early ROM exercise using CPM were thought to improve the range of motion of involved knee. -
Citations
Citations to this article as recorded by- A Modified Thompson Quadricepsplasty for Extension Contracture Resulting From Femoral and Periarticular Knee Fractures
Mohammad H. Ebbrahimzadeh, Ali Birjandi-Nejad, Said Ghorbani, Mohammad Reza Khorasani
Journal of Trauma: Injury, Infection & Critical Care.2010; 68(6): 1471. CrossRef
- A Modified Thompson Quadricepsplasty for Extension Contracture Resulting From Femoral and Periarticular Knee Fractures
- 643 View
- 2 Download
- 1 Crossref

Case Report
- Osteochondral Avulsion Fracture in Patella after Treatment of Abscess around Knee: A Case report
- Keun Soo Lee, Geon Woo Lee, Sang Ho Song, Hyun Seo
- J Korean Soc Fract 1999;12(2):290-293. Published online April 30, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.2.290
-
 Abstract
Abstract
 PDF
PDF - Osteochondral avulsion fracture of patella has been rarely reported. We experienced one case of osteochondral avulsion fracture which was developed after abscess around knee. The patient was a 16year old with the history of abscess. The presenting symptom was knee pain and loss of extension power. Radiologic and operative findings suggested that osteochondral avulsion fracture of the patella, was caused by minor trauma near the insertion site of quadriceps tendon. In usual case of quadriceps tendon rupture, the rupture occurred at the musculotendinous junction, caused by sudden contracture of the muscle without trauma history. This case was treated successfully with tension band wiring technique. Differential diagnosis between osteochondral avulsion fracture and osteomyelitis of patella was emphasized.
- 404 View
- 0 Download

Original Article
- Injuries of the Knee Associated with Fractures of the Tibial Shaft
- Kwang Won Lee, In Sung Hwang, Seung Hun Lee, Tae Gyoo Ahn, Ha Yong Kim, Whoan Jeang Kim, Won Sik Choy
- J Korean Soc Fract 1999;12(2):277-283. Published online April 30, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.2.277
-
 Abstract
Abstract
 PDF
PDF - Two hundred and seventeen consecutive patients with two hundred and twenty five diaphyseal tibia fractures were retrospectively reviewed to evaluate the frequencies, types and the results of treatments for the associated ipsilateral knee ligaments and menisci injuries from May 1993 to Feb 1997 at Eulji Medical College Hospital. Average follow-up period was 41 months(20~65 months). Thirteen patients with knee injuries(5.8%) were diagnosed by stress X-ray & MRI evaluation and confirmed by arthroscopic examination. Eleven patients(84.6%) were diagnosed as having a ligament or meniscus injury at the time of initial management. The posterior cruciate ligament(PCL) was injured in eight patients(50%); the anterior cruciate ligament(ACL), in three; the medial collateral ligament, in three; the lateral collateral ligament, in two: the medial meniscus, in two; and the lateral meniscus, in two. There was no relationship between specific ligament damage and the cause of the injury or level of fracture. Collateral ligament injuries, two ACL, and four PCL injuries were treated conservatively and one PCL injuries were treated with pull-out suture technique and another four PCL injuries were treated with reconstruction using bone-patella tendon-bone. One ACL injury was treated with reconstruction using semitendinosus tendon. As evaluated by the method of HSS knee score, there were seven(53.9%) excellent, four(30.8%) good, and two fair(15.3%). On the basis of the results of this study, we believe that, after stabilization of a fracture of the tibial shaft, it is essential to examine the knee throughly to identify any associated ligamentous injuries.
- 380 View
- 2 Download

Case Report
- Bilateral Floating Knees Treated by 4 Intramedullary Nails: A Case Report
- Phil Hyun Chung, Dong Ju Chae, Sang ho Moon, Ho Gyoon Bae
- J Korean Soc Fract 1999;12(2):267-271. Published online April 30, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.2.267
-
 Abstract
Abstract
 PDF
PDF - The treatment of simultaneous ipsilateral femoral and tibial fractures is a challenging therapeutic problem. Unfortunately, despites a number of reports on these fractures, guidelines for treatment have not been well established. Because the knee joint is isolated partially or completely, the term "floating knee"is used. But most of these injuries are ipsilateral and few bilateral cases were reported in the literatures. The authors reviewed a case of bilateral floating knee treated by 4 intramedullary nails without having any prolonged healing time or limited range of motion in both knee joint postoperatively.
- 373 View
- 0 Download

Original Articles
- Surgical Treatment of Ipsilateral Fracture of the Femur and Tibia("Floating Knee")
- Eu Sub Chung, Ki Sik Hong, Seung Soo Hwang
- J Korean Soc Fract 1998;11(4):825-832. Published online October 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.4.825
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fractures of the femur and tibia is also called "Floating knee", It is the term applied to the flail knee joint segment resulting from a fracture of the shaft or adjacent metaphysis of the ipsilateral femur and tibia. The principles of the treatment is focussed to the rigid fixation and early restoration of the knee function. Authors reviewed 24 patient in which were treated surgical management from January 1991 to June 1998. The results were as following : 1. The patient who had both diaphyseal fractures had better clinical result than metaphyseal fractures. And the metaphyseal fractures associated with intraarticular fractures were worse than other metaphyseal fractures. 2. At the last follow up, the excellent and good results were achieved in 71% of the patients treated with internal fixation of both fractures and 60% of the patient with external fixation of the tibia, but all of the patient with wxternal fixation of the femur were poor result by Karlstrom and Olerud criteria.
- 364 View
- 1 Download

- Clinical and Radiologic Analysis of Occult Osseous Lesion on Magnetic Resonance Imaging in Acute Knee Injury
- Seung Key Kim, Jong Hun Lee, Nam Gee Lee, Chang Beom Park, Han Chang
- J Korean Soc Fract 1997;10(4):843-850. Published online October 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.4.843
-
 Abstract
Abstract
 PDF
PDF - Bone bruise or occult osseous lesion on magnetic resonance imaging was focused on the indirect sign of acute anterior cruciate ligament injury. But there were few reports which compared the location of bone bruise with the injured structure. The purposes of this study were to identify the common pattern of location of bone bruise, and to analyze the relationship between the location and injured structure or mechanism of injury. The authors reviewed 76 magnetic resonance imaging studies of the knee from March 1993 to May 1994 which show the sign of bone bruise in acute knee injury within six weeks. The mean age of the patient was 26.3 years and the main cause of injury was traffic accident. The final diagnosis was 20 cases of isolated medial collateral ligament injury, 17 cases of isolated anterior cruciate ligament injury, 16 cases of combined anterior cruciate and medial collateral ligament injury, 7 cases of meniscus injury, 6 cases of combined posterior cruciate and medial collateral ligament injury, 5 cases of isolated posterior cruciate ligament injury, 2 cases of patella dislocation, 1 case of lateral collateral ligment injury, and 2 cases of undiagnosed knee injury. In isolated MCL injuries, bone bruises were all confined to the lateral compartment. In isolated injury of ACL, the most common pattern of location of bone bruises were lateral tibial plateau and lateral femoral condyle(47.1%). In combined ACL and MCL injury, the most common pattern of location was lateral tibial plateau, only(43.8%). Bone bruise on MRI may be easy to detect during interpretation and we can obtain much information to decide the diagnosis and prognosis.
- 452 View
- 0 Download

Case Report
- Treatment of Chronic Uncontrolled Infected Nonunion of Femur and Knee with the Ilizarov Instrument: 3 cases reports
- Duk Yong Lee, Jae Ik Shim, Taik Seon Kim, Sung Jong Lee, Suck Ha Lee, Hyung Gon Jee
- J Korean Soc Fract 1997;10(4):801-811. Published online October 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.4.801
-
 Abstract
Abstract
 PDF
PDF - We analysed three cases, repectively. The first case was chronic uncontrolled infected nonunion of femur due to open type III fracture which had been operated unsuccessfully at least 5 times. The second case was a infected nonunion and shortening of leg due to infecton of soft tissue surgery and then after knee arthrodesis. The third case was result from the total knee arthroplasty failure and then after knee arthrodesis. Ilizarov instrument was applied to this case for the knee joint arthrodesis. All cases showed bony union after average 14.6 months. The exact bony lengthening in the two cases after treatment was 11cm and 13cm and the healing index was 49.Odays/cm and 50.8days/cm The complications included the pin tract infection in all three cases and pin breakage in 2 of the cases. We achieved bony lengthening and bony union with relief of infection in 3 cases of chronic uncontrolled infected nonunion of femur treated with extensive saucerizaton and fixation using the Ilizarov instrument. These are the results of our treatment of chroic uncontrolled infected nonunion of femur using the Ilizarov instrument.
- 363 View
- 0 Download

Original Articles
- The Treatment and Complications of Ipsilateral Fracture of the Femur and tibia
- Kyu Min Kong, Ki Chan Ahn, Sung Seok Seo, Young Chang Kim, Jang Seok Choi, Young Goo Lee
- J Korean Soc Fract 1997;10(3):556-561. Published online July 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.3.556
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fracture of the femur and tibia is difficult to treat because it is often comminuted and combined with severe soft tissue injury. And The result of treatment is poor in most cases. The thirty-four cases were treated at Pusan Paik Hospital from March, 1992 to February, 1995. The result were as follows; 1. The bony union time was shorter in the intramedullary nailing than other methods. 2. There were less complications in the group of used intramedullary nailing than other methods. 3. The intramedullary nailing was relatively good treatment method for ipsilateral fracture of the femur and tibia.
- 339 View
- 0 Download

- The Results of the Treatment with Circular External Fixator for Severely Comminuted Intraarticular Fractures involving the Knee
- Gang Wook Lee, Je Hoon Lee, Byung Yun Hwang
- J Korean Soc Fract 1996;9(2):424-430. Published online April 30, 1996
- DOI: https://doi.org/10.12671/jksf.1996.9.2.424
-
 Abstract
Abstract
 PDF
PDF - In treating the patients having the intraarticular condylar fractures of the distal femur and the proximal tibia, many aulhors have recommended accurate anatomical reduction and rigid internal fixaion with early mobiliEation of the thee. But we cant often reduce the displaced bony fragments into the anatomical position and also fix them rigidly in severely comminuted and displaced fractures in proctice. Furthermore open wound makes surgeons face with some difficulties in using internal fixatives due to postoperative osteomyelitis. We treated 16 cases of severely comminuted intraarticular fractures involving the knee with circular fikator from March, 1992 to October 1994. Those were composed of 8 intraarticular femoral condylar fractures in which 7 cases were classified as C3 by AO classification and 6 cases had open wound, and 8 intraarticular tibil condylar fractures in which 8 cases were classified as type VI by Schatzkers classification and 6 cases showed open fractures. We could get bony union in all cases but we were not satisfied with the functional results of the treatment. So, we recommend the circular external fixation as a method for the treatment of these severely comminuted fractures involving the knee, and we think that further study for improving the functional results will be needed.
- 369 View
- 0 Download

- Treatment of the Ipsilateral fracture of Femur and Tibia in Children
- Jong Seok Park, Yoon Sik Kim, Hee Kwon, Jun Min Song, Soo Kyun Rah, Chang Uk Choi
- J Korean Soc Fract 1996;9(1):129-136. Published online January 31, 1996
- DOI: https://doi.org/10.12671/jksf.1996.9.1.129
-
 Abstract
Abstract
 PDF
PDF - Sixteen cases of fracture of the femur and tibia on the same leg in children below 16 year age were treated in Soonchunyang Univ. Hospital during the period 1988-1993. We studied all of these patients, classified by LettsNew classification of pediatric floating knee, retrospectively with analysis of treatment and results. The results were as follows; 1. Among the 16 cases,14 cases were male(88%), and 10 cases(63%) were at their first decade and 6 cases(37%) were at second decades. 2. The main cause of injury was traffic accident;15 cases(94%). 3. The most common concomitant injury was fracture in other site;5 cases(31%). 4. Among the 9 cases of conservative treatment, limping and leg length inequality were occurred in 6 cases(61%), and malunion in 5 cases(56fo). 5. Among the 7 cases of operative treatment, limping was occurred in 1 cases(14%), leg length inequality was in 2 cases(29%), and malunion in 3 cases(43%). 6. Among the 10 cases at first decade, limping was occurred in the 6 cases(75%) out of 8 cases of conservative treatment, but it was not occurred in 2 cases of operative treatment. According to the results, we suggest that at least one fracture should be rigidly fixed in all cases.
- 326 View
- 0 Download

- The Ilizarov Method for the Treatment of Open Intraarticular Fractures around the Knee Joint: Clinical Analysis of 6 Cases
- Chang Hyouk Choi, Koing Woo Kwun, Shin Kun Kim, Sang Wook Lee, Yong Joo Kim
- J Korean Soc Fract 1996;9(1):119-128. Published online January 31, 1996
- DOI: https://doi.org/10.12671/jksf.1996.9.1.119
-
 Abstract
Abstract
 PDF
PDF - There are many difficulties in treating open intraarticular fracture around the knee joint because of its combined neurovascular injury and comminution of fracture site. The difficulties lie in choosing a fixation method, postoperative care, and analyzing the results of the treatment. Recently there is growing preference in using Ilizarov apparatus. The merits of Ilizarov in fracture treatment are early weight bearing and easy compression and distraction. In cases of this study, difficulties were subclassified into problems, obstacles. and complications. Six cases of open intraarticular fracture around the knee joint were treated from Mar., 1993 to Aug.,1994 and the average follow up period was twenty months and the results were as follows: 1. Of the six patients, there were five males and one female patients. 2. The cause of the fractures was traffic accident in five and crushing injury in one. 3. Of the six cases, five cases were combined femoral and tibial fractures and one case was only femoral condylar fracture. 4. In follow up study, there was thirty cases of difficulties such as pin site problem, pain, limitation femotion, and nonunion etc. 5. Of the seventy-four wires, pin site problem occurred at twenty pins but open wounds were cured without infection evidence. 6. The results were poor in all cases. 7. The Ilizarov technique requires adequate implantation and management to reduce an overall complication rate and improve functional results.
- 418 View
- 0 Download

- Treatment of Ipsilateral Fracture of the Femur and Tibia("Floating Knee")
- Soo Bong Hahn, Gang Hee Koh
- J Korean Soc Fract 1995;8(3):488-496. Published online July 31, 1995
- DOI: https://doi.org/10.12671/jksf.1995.8.3.488
-
 Abstract
Abstract
 PDF
PDF - Concomitant ipsilateral femoral and tibial fractures present a challenging therapeutic problem. They are generally caused by high-energy trauma, primarily motor-vehicle accidents, and the local trauma to the soft tissue is often extensive. We retrospectively reviewed 48 cases of the ipsilateral fracture of femur and tibia from March 1983 to March 1993 and analyzed the clinical and functional results. The results were as follows. 1. The most common site of fracture was middle one-third and the most common type of the fracture was comminuted in both femur and tibia. 2. The most common associated injury was concomitant fracture and dislocation of other sites(28 cases) and fat embolism was developed in 4 cases and compartment syndrome was developed in 3 cases. 3. Satisfactory reults were achieved in 72% of the patients treated with internal fixation of both fracture, 63% of the patient with internal fixation for the femur and 43% of the patients managed conseuatively.
-
Citations
Citations to this article as recorded by- Comparison of Floating Knee according to Presence of Knee Joint Injury
Eau-Sup Chung, Jong Hyuk Park, Hee Rack Choi, Joo Hong Lee, Kwang-Bok Lee
Journal of the Korean Fracture Society.2012; 25(4): 277. CrossRef
- Comparison of Floating Knee according to Presence of Knee Joint Injury
- 557 View
- 1 Download
- 1 Crossref

Case Report
- Minimal Arthrotomy for Postoperative Knee Arthrofibrosis in Patella Fracture: Report of 3 Cases
- Koon Soon Kang, Jun Seop Jahng, Young Chul Cho
- J Korean Soc Fract 1994;7(2):397-403. Published online November 30, 1994
- DOI: https://doi.org/10.12671/jksf.1994.7.2.397
-
 Abstract
Abstract
 PDF
PDF - Significant and Permanent loss of knee flexion or extension is a recognized and disabling complication of either operative procedures or trauma about the knee. We have experienced 3 cases of the postoperative ankylosis of the knee after the patella fracture, in which the range of motion of the knee was not satisfactory after the trial of the arthroscopic Iysis of adhesion with manipulation of the knee, so minimal arthrotomy, limited lateral arthrotomy combined with medial arthrotomy, were performed and revealed the satisfactory results.
- 410 View
- 2 Download

Original Articles
- The Treatment of Supracondylar Femur Fracture after Total Knee Replacement
- Dae Kyung Bae, Hong Ku Lee, Chong Hoon Cho
- J Korean Soc Fract 1994;7(1):181-186. Published online May 31, 1994
- DOI: https://doi.org/10.12671/jksf.1994.7.1.181
-
 Abstract
Abstract
 PDF
PDF - We had five cases of the supracondylar fracture of the femur among 419 total knee arthroplasties in 330 patients that were done between January 1989 and december 1992 The incidence was 1.2%. Two cases were treated by non-operative methods. One case was treated by open reduction and screw fixation. And other two cases were treated by closed intramedullary Ender nailing. Prearthroplastic diagnosis was three cases of rheumatoid arthrltis, one degenerative arthritis and one tuberculous arthritis. The average age was 49.8 years(range, 34 to 71) and all patients were female. The supracondylar fractures occured by fall down injury and those were not associated with other injury The average duration between total knee arthroplasty and fracture was 1 year 8 months(range 9 months to 3 year 9 months). The average follow up period was 13 months(range, 6 months to 2 year 6 months). Posttreatment angulation was 2.3 degrees in AP plane and 6.7 degrees in lateral plane.
- 422 View
- 0 Download

- Yvascular Injuries Associated with Fracture and Dislocastion of the Knee
- Sung Joon Kim, Il Yong Choi, Jae Lim Cho, Soo Tai Chung
- J Korean Soc Fract 1990;3(1):40-45. Published online May 31, 1990
- DOI: https://doi.org/10.12671/jksf.1990.3.1.40
-
 Abstract
Abstract
 PDF
PDF - Injury of the popliteal artery associated with fracture and dislocastion of the knee is uncommon, But, when the fracture and dislocation of the knee occurs, it frequently associated with vascular injuries, and vascular injury can be a very serious one because of ischemia that necessitates amputation. Sixteen vascular injuries combined by fractures and dislocation of the knee between March, 1985 and February, 1989 have been reviewed and the results are as follows. 1. There were 11 cases of proximal tibial fracture, 2 cases of distal femoral fracture and 3 cases of knee dislocation. 2. The site of injury which is proximal to insertion of the soleus muscle were 15 cases. 3. There were contusion in 11 cases, rupture in 4 cases and laceration in 1 case. 4. One of the 2 cases(50%) that were treated within 12 hours after injury survived, while two to 10 cases(20%) that were treated after 24 hours following injury survived. 5. The open reduction and internal fixation was done in 5 cases, the skeletal traction in 1 case, and cast immobilization in 10 cases. 6. Finally, the B-K amputation was done in 4 cases, A-K amputation in 6 cases, knee disarticulation in 2 cases.
- 338 View
- 0 Download

- Conservative Treatment of Ligamentous Injury of Knee in Head Trauma Patients
- Joon Young Kim, Young An Choi, Young Chul Choi, Bo Seok Kong
- J Korean Soc Fract 1989;2(1):42-48. Published online June 30, 1989
- DOI: https://doi.org/10.12671/jksf.1989.2.1.42
-
 Abstract
Abstract
 PDF
PDF - Operative treatment has been used in unstable ligamentous imjury of knee joint. We experienced three cases of ligamentous injury of knee that was accompained with head trauma and other organ injury. Despite of sugical candidate, we did only conservative treatment due to poor general condition and difficulty of anesthesia. The result was realtively better than we expected. We reported these cases.
- 373 View
- 0 Download

- Popliteal Artery Injuries Associated with Trauma Around the Knee
- Myung Chul Yoo, Chung Soo Han, Kye Lim Lee, Moon Hwan Lee
- J Korean Soc Fract 1989;2(1):34-41. Published online June 30, 1989
- DOI: https://doi.org/10.12671/jksf.1989.2.1.34
-
 Abstract
Abstract
 PDF
PDF - Between Jan. 1980 and Dec. 1987, 47 cases in 44 patients with politeal artery injury associated with trauma around the knee joint were managed at Department of Orthopaedic Surgery, KMC. Authors analysed the diagonstic methods, operations with its results and prognostic factors, and the results were as follows: 1. The incidence was 3%(44/1473) from Jan. 1980 to Dec. 1987 2. 14 cases of 19 cases, who underwent the vascular surgery, were survived(74%) and further amputations were applied to failed 5 cases. 3. Doppler flowmeter was considered as very useful diagnostic tool because of simplicity, safety, and accuracy, therefore angiography was not necessary in all cases. 4. The length of ischemic time and the amount of associated soft tissue damage were considered as important prognostic factors. 5. Vein graft was considered as good operative technique, but thrombectomy alone was not enough method for politeal artery injury. 6. ligament repair was not always necessary in treatment of popliteal artery injury associated dislocation of knee. 7. Prophylatic decompression was necessary in all cases after vascular surqery and fibulectomy fasciotomy was considered as outstanding technique.
- 351 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


