Search
- Page Path
- HOME > Search
Original Articles
- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 897 View
- 2,147,483,670 Download

- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
-
 Abstract
Abstract
 PDF
PDF - Background
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
Methods
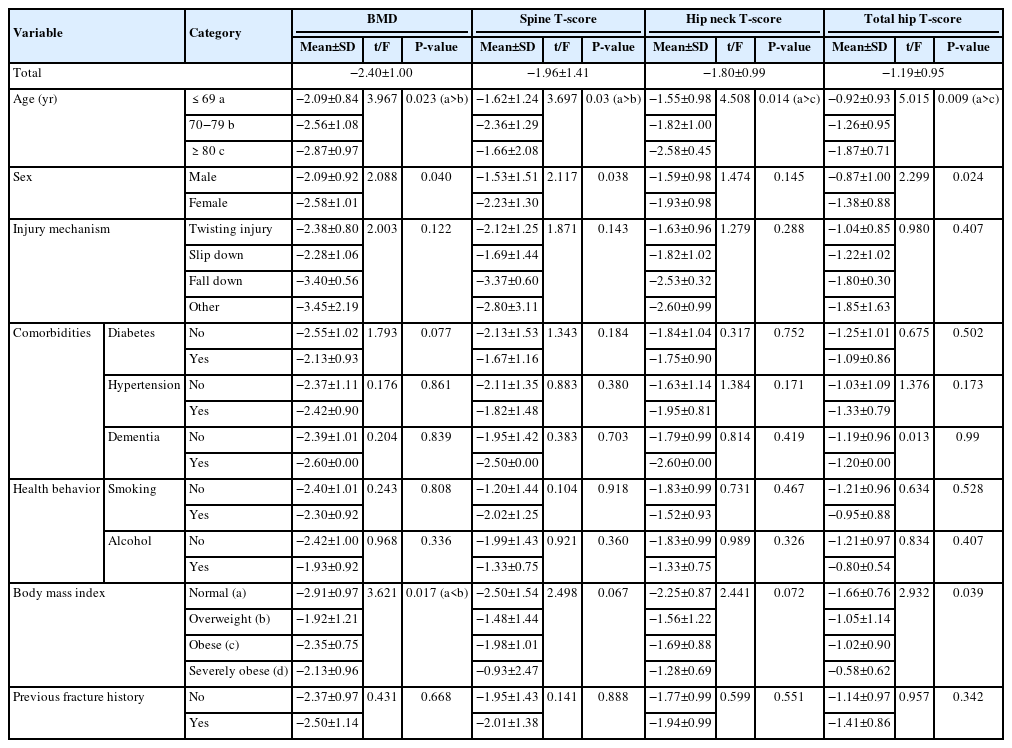
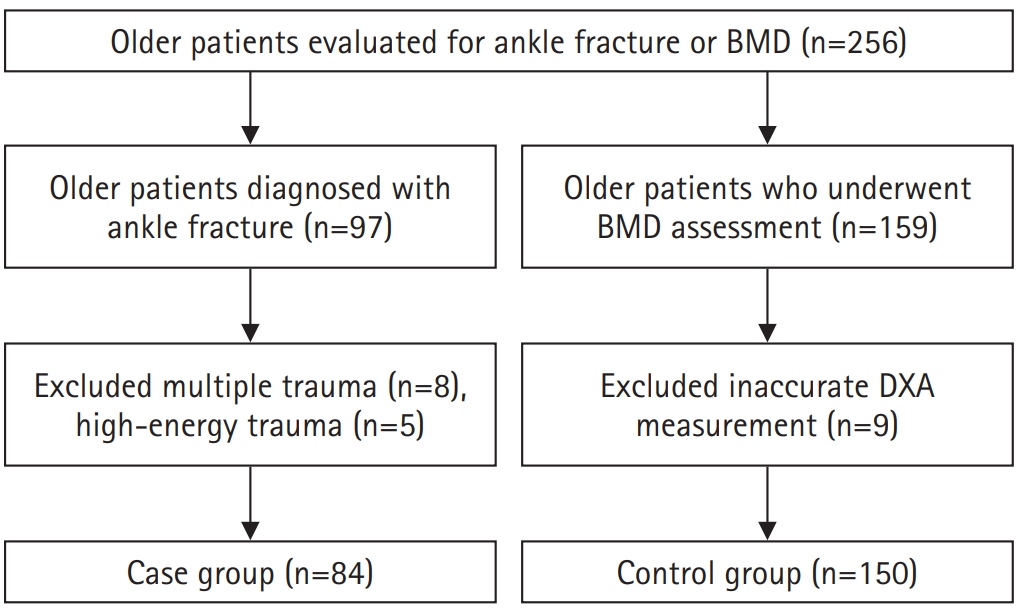
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 1,165 View
- 22 Download

- Biomechanical Investigation to Establish Stable Fixation Strategies for Distal Tibial Fractures in Various Situations: Finite Element Analysis Studies
- Sung Hun Yang, Jun Young Lee, Gu-Hee Jung, Hyoung Tae Kim, Ba Woo Ko
- J Korean Fract Soc 2024;37(2):71-81. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.71
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the structural and mechanical stability as well as the clinical significance of various fixation constructs for distal tibial fractures using finite element analysis.
Materials and Methods
Fracture models with 20 mm and 120 mm defects were produced, and implants of an intramedullary nail and anatomical plate model were applied. An axial load of 800 N with 60% distribution in the medial compartment and 40% in the lateral compartment was applied and analyzed using Ansys ® software.
Results
In the intramedullary nail model, the maximum von Mises stress occurred at the primary lag screw hole and adjacent medial cortex, while in the plate model, it occurred at the locking holes around the fracture. The maximum shear stress on the bone and metal implant in the fracture model with a 20 mm defect was highest in the plate assembly model, and in the fracture model with a 120 mm defect, it was highest in the two-lag screw assembly model.
Conclusion
Based on an analysis of the maximum shear stress distribution, securing the fixation strength of the primary lag screw hole is crucial, and the assembly model of the intramedullary nail with two lag screws and a blocking screw applied was the model that best withstood the optimal load. Securing the locking hole directly above the fracture is believed to provide the maximum fixation strength because the maximum pressure in the plate model is concentrated in the proximal locking hole and the surrounding cortex. -
Citations
Citations to this article as recorded by- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
Journal of Musculoskeletal Trauma.2025; 38(2): 74. CrossRef
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- 953 View
- 19 Download
- 1 Crossref

- Treatment Results of Reamed Exchange Nailing in Aseptic Nonunion of Tibial Shaft Fracture
- Yongjin Cho, Jun Young Lee, Jehong Ryu, Hyoung Tae Kim, Jong Jin Moon
- J Korean Fract Soc 2023;36(4):125-132. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.125
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intramedullary nailing is used widely for treating tibial diaphysis fractures because of its relatively rigid internal fixation, which allows weight bearing, resulting in rapid bone healing and functional recovery. This study evaluated the results of exchange nailing in treating aseptic nonunion of tibial shaft fractures.
Materials and Methods
From November 2015 to December 2021, a retrospective study was conducted on patients who had undergone intramedullary nailing for tibial diaphysis fractures. Among them, this study focused on patients diagnosed with nonunion and who underwent exchange nailing. Twenty patients with a minimum follow-up period of at least 12 months were included in the study.
Results
The mean ages of patients were 60 years (range, 30-79 years). Of the 20 cases in which exchange nailing was performed, bone union was achieved in 18 cases (90.0%), and the mean period was 23 weeks (range, 14-46 weeks). Among the 18 cases of bone union, one case exhibited delayed union and achieved union without additional treatment after 46 weeks, while two cases of nonunion failed to achieve union and were lost to follow-up until the final assessment.
Conclusion
Reamed exchange nailing performed on aseptic nonunion after intramedullary nailing for tibial diaphysis fractures had satisfactory clinical outcomes.
- 518 View
- 4 Download

- Outcomes of Minimally Invasive Surgery in Intra-Articular Calcaneal Fractures: Sanders Type III, Joint Depressive Type Calcaneal Fracture
- Je Hong Ryu, Jun Young Lee, Kang Yeol Ko, Sung Min Jo, Hyoung Tae Kim
- J Korean Fract Soc 2023;36(3):85-94. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.85
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the radiologic and clinical outcomes of a minimally invasive technique using the tarsal sinus approach in the management of Sanders type III, joint depressive type calcaneal fractures.
Materials and Methods
Between July 2011 and September 2019, data of 29 patients who underwent a minimally invasive procedure with the sinus tarsi approach for Sanders type III joint depressive intra-articular calcaneal fractures, and were followed up for more than 1 year were analyzed. We evaluated the radiologic outcomes by assessing the radiologic parameters (Böhler angle, Gissane angle, calca-neal length, calcaneal height, calcaneal width). We also evaluated the clinical outcomes based on the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score and the complications associated with the technique.
Results
The radiological results showed an improvement in the Böhler angle from 2.5° to 18.6° and the Gissane angle from 132.4° to 119.1° after the operation. The mean AOFAS score during the clini-cal evaluation was 79.5. We observed 13 cases of posttraumatic arthritis, 1 case of subtalar arthrodesis, and no case of wound complication.
Conclusion
Minimally invasive technique for Sanders type III joint depressive calcaneal fractures resulted in relatively satisfactory radiologic and clinical outcomes. Open reduction and internal fixation through the sinus tarsi approach reduce complications including wound problems. This approach offers satisfactory results without long-term complications.
- 564 View
- 2 Download

- Comparison of Surgical Outcomes for Lisfranc Joint Injuries: Dorsal Bridge Plating versus Transarticular Screw versus Combination
- Ba Rom Kim, Jun Young Lee, Sung Hun Yang, Seung Hyun Lee
- J Korean Fract Soc 2023;36(1):17-24. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.17
-
 Abstract
Abstract
 PDF
PDF - Purpose
In Lisfranc joint injury, the traditional treatment has been open reduction and internal fixation with a transarticular screw. Despite this, additional complications, such as damage to the articular surface and breakage of the screw, have been reported. Therefore, this study compared the clinical and radiological outcomes of dorsal bridge plating with those of transarticular screws and combination treatment in Lisfranc joint injury.
Materials and Methods
Among the 43 patients who underwent surgical treatment due to Lisfranc joint injury from June 2015 to March 2021, 40 cases followed for more than six months after surgery were analyzed, excluding three patients: one lost to follow-up, one had to amputate, and one expired. The radiological parameters were measured using the Wilppula classification in the last follow-up. The clinical outcomes were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) midfoot score.
Results
The AOFAS midfoot score, according to the surgical method, was significantly higher in the dorsal bridge plating (p=0.003). The radiological outcomes showed significantly better anatomical reduction when dorsal bridge plating was used (p=0.040). According to the Wilppula classification, the AOFAS midfoot score improved as the quality of anatomical reduction improved (p=0.018). Finally, the AOFAS midfoot score decreased as the number of column fixations increased (p=0.002). There were two complications: screw breakage in dorsal bridge plating and superficial skin necrosis in the combination treatment. Skin defects caused by necrosis improved after negative pressure wound therapy and split-thickness skin graft.
Conclusion
In treating Lisfranc joint injuries, open reduction and internal fixation by dorsal bridge plating can be an appropriate treatment option. Nevertheless, studies, such as long-term follow-up research, on complications, such as osteoarthritis, will be needed.
- 764 View
- 10 Download

- Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
- Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
- J Korean Fract Soc 2022;35(4):135-141. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.135
-
 Abstract
Abstract
 PDF
PDF - Purpose
Patients with diabetes are known to have poor clinical outcomes due to the high incidence of complications after ankle joint fracture surgery. This study reports the clinical and functional outcomes based on glycemic control status among patients with ankle joint fractures who underwent surgical treatment.
Materials and Methods
Among patients who underwent surgical treatment due to ankle joint fractures from January 2015 to October 2019, 253 patients with a minimum follow-up of 12 months were identified. We divided them into 3 groups: 195 patients with no diabetes (Group A), 26 patients with well-controlled diabetes (Group B), and 32 patients with uncontrolled diabetes (Group C). In addition, patients with lateral, medial malleolar, bimalleolar, and trimalleolar fractures were identified using radi-ography. The functional outcome measures used for evaluation were the Revised Foot Function Index (FFI), Short Musculoskeletal Function Assessment (SMFA), and the Foot and Ankle Outcome Score (FAOS).
Results
Bone union at 3 months after surgery was high in Group A, showing significant differences compared to the other groups. There was a significant difference between the groups in the incidence of arthropathy and one or more complications. However, the FFI, SMFA, and FAOS did not show significant differences between the groups.
Conclusion
The incidence of complications was high in patients with uncontrolled diabetes compared to the patients with well-controlled diabetes and those with no diabetes. However, functional outcomes showed no significant difference.
- 676 View
- 6 Download

- Posterior Anti-Glide Plating for Supination External Rotation Type Lateral Malleolar Fractures: Clinical Comparison of Locking versus Non-Locking One-Third Semi-Tubular Plate Fixation
- Jun Young Lee, Yong Jin Cho, Dong Hyuk Cha, Hyun Bai Choi, Jung Ho Lee
- J Korean Fract Soc 2022;35(2):57-62. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study was to evaluate and compare the clinical and radiological outcomes between locking plates and non-locking plates using posterior anti-glide plating for supination external rotation type lateral malleolar fractures.
Materials and Methods
A total of 50 patients who underwent internal fixation of posterior anti-glide plating due to lateral malleolar fractures, classified as supination-external rotation (SER) as per the Lauge-Hansen classification system, at our hospital from January 2017 to November 2018 were retro-spectively evaluated. Patients were divided into two groups: 1/3 semi-tubular locking plate (24 patients) and 1/3 semi-tubular non-locking plate (26 patients). A radiographic assessment was performed after surgery to evaluate the time of bone union. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot functional score was measured after the surgery to evaluate the clinical outcomes.
Results
The two groups showed similar distributions in sex, age, height, body mass index, fracture pattern, and mean follow-up period. Complete bone union was obtained in all cases and the mean bone union time was 13.00±3.38 weeks in Group 1 and 12.92±3.26 weeks in Group 2 (p=0.87). The mean AOFAS score at 24 weeks was 95.66±2.86 in Group 1 and 95.84±2.79 in Group 2 (p=0.82). The mean AOFAS score at 48 weeks was 97.25±3.54 in Group 1 and 96.57±3.07 in Group 2 (p=0.47). Two cases of complications were observed in the non-locking plate group.
Conclusion
For the treatment of Lauge-Hansen SER type lateral malleolar fracture, internal fixation us-ing locking 1/3 semi-tubular plate and non-locking 1/3 semi-tubular plate are both favorable fixation methods.
- 358 View
- 2 Download

- Comparison of the Results between Plating and Intramedullary Nailing for Ipsilateral Fibular Fractures in Pilon Fractures
- Yong Jin Cho, Jun Young Lee, Jae Hwan Lim, Je Hong Ryu, Jung Ho Lee
- J Korean Fract Soc 2021;34(3):97-104. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.97
-
 Abstract
Abstract
 PDF
PDF - Purpose
To compare the results between plating and intramedullary nailing for ipsilateral fibular fractures in pilon fractures.
Materials and Methods
Among 124 patients with pilon fractures from November 2008 to March 2019, 50 patients with a fibular fracture were studied retrospectively and divided into two groups: Group A using a plate and Group B using a Rush pin. The radiological tests confirmed the fracture pat-terns (Rüedi–Allgöwer classification, AO/OTA classification) and evaluated the degree of reduction of fibular and tibial fractures after surgery. The American Orthopaedic Foot & Ankle Society (AOFAS) was examined for a clinical evaluation, and the complications were checked.
Results
The two groups showed similar distributions in gender, age, injury mechanism, diabetes, smoking, mean follow-up period, Rüedi–Allgöwer classification, AO/OTA classification, and open fracture. The fibular fractures were classified as simple, wedge, multiple, and segmental, showing significant differences between the two groups (p=0.03). There was no difference in the Talocrural angle, Shenton line, and Dime sign. In the reduction of pilon fractures, the appropriate reduction was obtained in 22 cases (88.0%) for both groups. The AOFAS averaged 83.24 in Group A and 80.44 points in Group B, showing no significant difference in complications (nonunion, malunion, infection, and arthritis).
Conclusion
Regardless of how the fibular fracture was fixed, the reduction of pilon fractures in both groups showed good results. Both intramedullary nail and plate fixation could be a suitable fixation method for ipsilateral fibular fractures with a low risk of shortening in pilon fractures.
- 463 View
- 3 Download

- Results of Intramedullary Nailing for Distal Metaphyseal Intra-Articular Fractures of Tibia
- Jun Young Lee, Yongjin Cho, Hyung Seok Park, Se Woong Jang
- J Korean Fract Soc 2020;33(4):196-203. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.196
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the results of internal fixation using an intramedullary nail in the treatment of distal metaphyseal fractures involving the articular surface.
Materials and Methods
From November 2009 to November 2018, distal tibia fractures involving the articular surface were treated with intramedullary nailing only for fractures corresponding to AO type 43 B and 43 C1, twenty-four cases were studied retrospectively. The tibial alignment was measured preoperatively and postoperatively, and the bone union time and nonunion were assessed. In addition, the clinical evaluation of ankle joint function was assessed using the Olerud and Molander ankle score (OMAS).
Results
Complete bone union was obtained in all cases, and the mean union time was 17.7±1.87 weeks (range, 15-20 weeks). The average preoperative coronal alignment was 6.4°±1.0° (range, 5.2°-8.4°), and sagittal alignment was 2.7°±0.6° (range, 1.9°-3.8°). The average postoperative coronal alignment was 2.5°±0.13° (range, 2.2°-2.6°) and sagittal alignment was 0.4°±0.25° (range, 0.09°-0.95°). There was no nonunion. The OMAS had an average of 85±7.9 points (range, 70-95 points).
Conclusion
In the treatment of distal metaphyseal fractures involving the articular surface, internal fixation using an intramedullary nail reduces complications and achieves satisfactory reduction and union. This method is considered an excellent treatment to obtain good clinical results.
- 538 View
- 4 Download

- Clinical Outcome after Treatment of Tibia Segmental Fracture with Intramedullary Nailing and Minimal Invasive Plate Osteosynthesis
- Jun Young Lee, Hyung Seok Park, Dong Hyuk Cha
- J Korean Fract Soc 2020;33(3):142-147. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.142
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the clinical outcomes after the treatment of a tibia segmental fracture with intramedullary nailing (IM nailing) and minimal invasive plate osteosynthesis (MIPO).
Materials and Methods
From July 2012 to December 2017, 14 out of 17 cases from a treatment cohort of 32 cases of AO type 42 C2 tibia segmental fractures with IM nailing and MIPO were studied retrospectively. Periodic radiographs were used to evaluate the presence of union, union time, and radiographic evaluation of bony union (varus-valgus deformity, anteroposterior angular deformity, shortening). To evaluate the postoperative clinical function, modified Rasmussen’s system was used for proximal fractures, and the American Orthopaedic Foot and Ankle Society functional score was used for distal fractures.
Results
Bony union was achieved in all 14 cases, and the average union time was 26 weeks. In one case of soil contamination, there were no other complications other than simple debridement after a soft tissue infection. The mean varus was two degrees; the mean anteroposterior angular deformity was three degrees of anterior oblique; the mean length shortening was 5 mm (2-9 mm). The mean functional score of the knee joint with the Modified Rasmussen’s system measured for the postoperative clinical function was relatively good (excellent 9, good 4, fair 1, and poor 0). The results of the Molander and Olerud Functional scores of the ankle joints were also good (excellent 8, good 3, fair 2, poor 0).
Conclusion
The treatment of tibia segmental fractures with IM nailing and MIPO can effectively reduce the gap of fracture sites. Hence, it is possible to increase the bony union probability and obtain relatively satisfactory alignment. Overall, the treatment of tibia segmental fractures with IM nailing and minimally invasive plate osteosynthesis appears to be a useful treatment, considering the preservation of the soft tissue and the alignment of the tibia.
- 648 View
- 4 Download

- Clinical Outcomes of Minimally Invasive Surgery in Sanders Type IV Intra-Articular Calcaneal Fractures
- Jun Young Lee, Hyunwoong Jang, Young Wook Kim
- J Korean Fract Soc 2019;32(4):181-187. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.181
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study evaluated the radiologic and clinical results in patients who underwent minimal invasive surgery using sinus tarsi approach in Sanders type IV calcaneal fracture.
MATERIALS AND METHODS
This retrospective study evaluated 13 cases of Sanders type IV calcaneus fractures that were treated by minimal invasive surgery using the sinus tarsi approach from July 2012 to April 2017. Further, these cases could be followed up for more than 12 months. Bone union, radiologic parameters such as Böhler's angle, Gissane's angle, calcaneal height, length, and width, the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, and the postoperative complications were evaluated.
RESULTS
Bony union was achieved in all the cases at the final follow up, and the mean union time was 5.5 months. One patient underwent reoperation for a surgical site infection, six patients had post traumatic arthritis, and two of them underwent subtalar joint fusion. The mean AOFAS ankle-hindfoot score was 81.2. At the final follow-up, the mean values of Böhler's angle and Gissane's angle were 20° and 119.8°, respectively, and the mean values of the calcaneus height, length, and width were 46.8 mm, 81.8 mm, and 45.6 mm, respectively.
CONCLUSION
Minimal invasive surgery using the sinus tarsi approach for Sanders type IV calcaneal fracture resulted in satisfactory anatomic reduction and stable fixation, and satisfactory clinical and radiologic results were obtained in most of the patients. Minimal invasive surgery is thought to reduce the soft tissue-related complications as compared to surgery using the extensile lateral approach.
- 1,034 View
- 16 Download

- Results of Exchange Nailing in Hypertrophic Nonunion of Femoral Shaft Fracture Treated with Nailing
- Suenghwan Jo, Gwang Chul Lee, Sang Hong Lee, Jun Young Lee, Dong Hwi Kim, Sung Hae Park, Young Min Cho
- J Korean Fract Soc 2019;32(2):83-88. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.83
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study examined the outcomes of exchange nailing for the hypertrophic nonunion of femoral shaft fractures treated with intramedullary nailing as well as the factors affecting the treatment outcomes.
MATERIALS AND METHODS
From January 1999 to March 2015, 35 patients, who had undergone intramedullary nailing with a femoral shaft fracture and underwent exchange nailing due to hypertrophic nonunion, were reviewed. This study investigated the time of union and complications, such as nonunion after exchange nailing, and analyzed the factors affecting the results.
RESULTS
Bone union was achieved in 31 cases (88.6%) after exchange nailing and the average bone union period was 22 weeks (14–44 weeks). Complications included persistent nonunion in four cases, delayed union in one case, and superficial wound infection in one case. All four cases with nonunion were related to smoking, three of them were distal shaft fractures, and one was a midshaft fracture with underlying disease.
CONCLUSION
Exchange nailing produced satisfactory results as the treatment of hypertrophic nonunion after intramedullary nailing. Smoking is considered a factor for continuing nonunion even after exchange nailing. In the case of a distal shaft, where the intramedullary fixation is relatively weak, additional efforts are needed for stability.
- 843 View
- 8 Download

- The Result of Using an Additional Mini-Locking Plate for Tibial Pilon Fractures
- Suenghwan Jo, Jun Young Lee, Boseon Kim, Kang Hyeon Ryu
- J Korean Fract Soc 2017;30(2):75-82. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.75
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We evaluated the usefulness of an additional, 2.7 mm mini-locking plate for tibial pilon fractures.
MATERIALS AND METHODS
We studied 21 patients (14 males and 7 females), who were treated with a 2.7 mm mini-locking plate via the anterolateral approach for tibial pilon fractures between September 2012 and April 2014. The mean age was 43.85 years, and the mean follow-up period was 16.6 months. The radiologic outcomes were graded by the Burwell and Charnley modified system and clinical outcomes were evaluated by the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hind foot score and visual analogue scale (VAS) score.
RESULTS
The mean union period was 14.3 weeks. At the final follow-up, radiologic results showed 16 excellent results, 4 fair results, and 1 poor result. The average VAS was 3.4 points; the average AOFAS score was 81.8 points. During the follow-up period, there were three cases of posttraumatic osteoarthritis and one case of superficial skin infection.
CONCLUSION
Additional anterolateral, 2.7 mm mini-locking plate may be a good treatment method to manage tibial pilon fractures.
- 538 View
- 5 Download

- The Result of Open Reduction and Mini-Plate Fixation for Displaced Talar Neck Fracture
- Woong Chae Na, Sang Hong Lee, Jun Young Lee, Sang Jun Lee, Boseon Kim
- J Korean Fract Soc 2015;28(4):215-222. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.215
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We evaluated the complications, radiological and clinical results after operative treatment using a mini-plate for fixation of displaced talar neck fractures.
MATERIALS AND METHODS
There were 20 cases of displaced talar neck fractures from May 2006 to December 2011; we performed a retrospective chart review of 15 patients treated by open reduction and internal fixation using a mini-plate who had more than 2 years of follow-up. According to Hawkin's classification, there were 7 cases of type II fractures and 8 cases of type III fractures. During postoperative 12-16 weeks we checked magnetic resonance imaging. The assessment of clinical results was based on the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot scale.
RESULTS
Mean union period was 11.6 weeks (10-15 weeks). Nonunion and malunion did not occur in all cases. The mean AOFAS score was 88.2 points (80-97 points). There were 5 cases of avascular necrosis. Of these, there were 3 cases of body collapse and 4 cases of post-traumatic arthritis. In the statistical analysis, there was no correlation between the elements including gender, Hawkin's classification and union rates and clinical results.
CONCLUSION
Mini-plate fixation of a displaced talar neck fracture is thought to be a good technique, with a low rate of malunion and also showed satisfactory results in radiological and clinical assessment. -
Citations
Citations to this article as recorded by- Outcome of Type 3 Talar Neck Fractures by Means of Medial Malleolar Osteotomy and Large Distractor
Sung Hae Park, Jun Young Lee, Jung Woo Lee
Journal of the Korean Orthopaedic Association.2019; 54(1): 45. CrossRef - The Measurement of Normal Talus in Korean Cadaver
Dong-Jun Ha, Heui-Chul Gwak, Jeon-Gyo Kim, Jung-Han Kim, Chang-Rak Lee, Young-Jun Kim, Jeong-Han Lee, Byung-Ho Ha, Ui-Cheol Kim
Journal of Korean Foot and Ankle Society.2016; 20(4): 163. CrossRef
- Outcome of Type 3 Talar Neck Fractures by Means of Medial Malleolar Osteotomy and Large Distractor
- 611 View
- 1 Download
- 2 Crossref

Review Article
- Current Concepts in Management of Pilon Fracture
- Jun Young Lee, Sang Joon Lee
- J Korean Fract Soc 2014;27(2):173-184. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.173
- 914 View
- 33 Download

Original Articles
- Outcomes and Analysis of Factors Affecting Bone Union after Interlocking Intramedullary Nailing in Segmental Tibia Fractures
- Sang Soo Park, Jun Young Lee, Sang Ho Ha, Sung Hae Park
- J Korean Fract Soc 2013;26(4):275-283. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.275
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the radiological results and complications of interlocking intramedullary nailing for segmental tibia fractures.
MATERIALS AND METHODS
Twenty-six patients (26 cases) who underwent interlocking intramedullary nailing for segmental tibia fractures between January 2003 and May 2011 were followed for more than one year. We evaluated the complications and statistically analyzed the factors influencing bone union, including open fracture, fracture site, reaming, postoperative angulation, and postoperative fracture gap.
RESULTS
Nineteen cases (73%) achieved bone union with one operation at an average of 7 months (range, 5 to 11). Seven cases had secondary procedures before achieving union. Complications included 7 cases of nonunion, 3 cases of incomplete peroneal nerve injury, 2 cases of superficial infection, 1 case of compartment syndrome. Factors showing statistically significant differences were open fracture, postoperative angulation, and postoperative fracture gap. Factors showing no statistically significant difference were fracture site and reaming.
CONCLUSION
Nonunion is the most common complication in interlocking intramedullary nailing for segmental tibia fractures. To minimize this complication, comprehension of surgical techniques to reduce anatomically and careful evaluation of the fracture are required. -
Citations
Citations to this article as recorded by- Clinical Outcome after Treatment of Tibia Segmental Fracture with Intramedullary Nailing and Minimal Invasive Plate Osteosynthesis
Jun Young Lee, Hyung Seok Park, Dong Hyuk Cha
Journal of the Korean Fracture Society.2020; 33(3): 142. CrossRef
- Clinical Outcome after Treatment of Tibia Segmental Fracture with Intramedullary Nailing and Minimal Invasive Plate Osteosynthesis
- 702 View
- 3 Download
- 1 Crossref

- The Result Treated by Open Reduction and Internal Fixation with Minimally Invasive Technique in Joint Depressive Calcaneal Fracture
- Sueng Hwan Jo, Jun Young Lee, Sang Ho Ha, Sung Won Cho, Sang Ha Park
- J Korean Fract Soc 2013;26(2):126-132. Published online April 30, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.2.126
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the short term follow-up results of minimally invasive technique in the management of Sanders type II, III, and IV joint depressive calcaneal fracture.
MATERIALS AND METHODS
Between May 2008 and May 2011, we studied 17 cases undergoing treatment with minimally invasive technique with modified sinus tarsi approach for Sanders II, III, and IV joint depressive intra-articular calcaneal fracture and were followed up for more than 1 year. We evaluated the treatment result by assessing the radiologic parameters (Bohler angle, Gissane angle, and calcaneal height/width/length) and clinical outcomes (American Orthopaedic Foot and Ankle Society [AOFAS] score and visual analog scale [VAS]) and investigating the complication.
RESULTS
Radiological results improved from 7.9degrees to 19.8degrees in the Bohler angle after the operation. Satisfactory results were obtained in clinical assessment with average AOFAS score of 82.45 and the average VAS score of 3.94. We experienced 3 cases of complications, 1 case of superficial wound infection and radiologic findings of subtalar arthritis in 2 cases.
CONCLUSION
Minimally invasive technique may be a useful alternative surgical method in the management of Sanders type II, III, and IV joint depressive calcaneal fracture that cannot adopt extensile approach, which enable to obtain good radiological and clinical results. -
Citations
Citations to this article as recorded by- Outcomes of Minimally Invasive Surgery in Intra-Articular Calcaneal Fractures: Sanders Type III, Joint Depressive Type Calcaneal Fracture
Je Hong Ryu, Jun Young Lee, Kang Yeol Ko, Sung Min Jo, Hyoung Tae Kim
Journal of the Korean Fracture Society.2023; 36(3): 85. CrossRef - Towards uniformity in communication and a tailor-made treatment for displaced intra-articular calcaneal fractures
Tim Schepers
International Orthopaedics.2014; 38(3): 663. CrossRef
- Outcomes of Minimally Invasive Surgery in Intra-Articular Calcaneal Fractures: Sanders Type III, Joint Depressive Type Calcaneal Fracture
- 678 View
- 2 Download
- 2 Crossref

- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture
- Jun Young Lee, Sang Ho Ha, Sung Won Cho, Sung Hae Park
- J Korean Fract Soc 2013;26(2):118-125. Published online April 30, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.2.118
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical and radiological results of minimally invasive plate, osteosynthesis, using either a locking compression plate-distal tibia (LCP-DT) or Zimmer periarticular locking plate (ZPLP) for distal tibia fractures.
MATERIALS AND METHODS
Fifty one patients (51 cases), who underwent minimally invasive osteosynthesis using locking compression plate for distal tibia fractures between October 2008 and August 2011, were followed for more than six months. Eighteen patients were treated with LCP-DT and 33 patients with ZPLP. Time to bony union and anatomic alignment were evaluated radiologically. Clinically, American Orthopedic Foot & Ankle Society ankle-hindfoot scales (AOFAS score) and range of ankle motion were assessed and compared between two groups.
RESULTS
All patients achieved bony union at an average of 18 weeks on LCP-DT group and 16weeks on ZPLP group. The average American Orthopedic Foot & Ankle Society ankle-hindfoot scales was 83.3 points on the LCP-DT group, 84.6 points on the ZPLP group, and range of ankle motion averaged at 45 degrees, 48 degrees, respectively.
CONCLUSION
Both types of locking compression plates were effective when performing minimally invasive osteosynthesis for distal tibia fractures. -
Citations
Citations to this article as recorded by- Biomechanical analysis and clinical effects of bridge combined fixation system for femoral fractures
Da-xing Wang, Ying Xiong, Hong Deng, Fu Jia, Shao Gu, Bai-lian Liu, Qun-hui Li, Qi Pu, Zhong-zi Zhang
Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine.2014; 228(9): 899. CrossRef
- Biomechanical analysis and clinical effects of bridge combined fixation system for femoral fractures
- 630 View
- 0 Download
- 1 Crossref

- The Results of Two Stage Surgical Treatment of Pilon Fractures
- Hong Moon Sohn, Jun Young Lee, Sang Ho Ha, Sang Hong Lee, Gwang Chul Lee, Kwang Hyo Seo
- J Korean Fract Soc 2012;25(3):177-184. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.177
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the good results of two-stage treatment in pilon fractures.
MATERIALS AND METHODS
A retrospective study of 23 patients among 30 patients with pilon fractures from March 2006 to November 2008, who underwent two-stage treatment of pilon fractures with a minimum of 24 months follow-up. The mean follow-up period was 28 months (24~41 months). In the first stage of the operation, open reduction of the articular surface and external fixation were performed after minimal incision. As the soft tissue healed, locking compression plate fixation was performed with the Minimally invasive plate osteosynthesis. Radiographic evaluation was graded by the criteria of Burwell and Charnley, and functional assessment of the ankle was evaluated by the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score.
RESULTS
The fractures were united within 16 weeks (12~30 weeks). The radiologic results showed anatomical reduction in 18 cases and a mean AOFAS score of 81. The mean range of ankle motion was 44 degrees. There were four complications: 1 case of wound infection and 3 cases of ankle osteoarthritis.
CONCLUSION
Two-stage treatment of pilon fractures is a good treatment method because it is designed to obtain early anatomical reduction, definitive stable fixation, low rates of soft tissue complication, and good range of ankle motion. -
Citations
Citations to this article as recorded by- Current Concepts in Management of Pilon Fracture
Jun-Young Lee, Sang-Joon Lee
Journal of the Korean Fracture Society.2014; 27(2): 173. CrossRef
- Current Concepts in Management of Pilon Fracture
- 746 View
- 4 Download
- 1 Crossref

- Comparative Analysis of Minimally Invasive Plate Osteosynthesis Using Periarticular Plate and Intramedullary Nailing in Distal Tibial Metaphyseal Fractures
- Gwang Chul Lee, Jun Young Lee, Sang Ho Ha, Hong Moon Sohn, Yi Kyu Park
- J Korean Fract Soc 2012;25(1):20-25. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.20
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare results between minimally invasive plate osteosynthesis using a periarticular plate and intramedullary nailing in distal tibial metaphyseal fractures in two treatment groups.
MATERIALS AND METHODS
Sixty-one cases of distal tibial metaphyseal fractures from December 2008 to December 2009 were evaluated. The minimal follow-up period was 12 months. Thirty patients treated by minimally invasive plate osteosynthesis using a periarticular plate were Group A; 31 patients treated by intramedullary nailing were Group B. We compared and analyzed the results of each group by radiological and clinical assessments.
RESULTS
The mean bony union time was 16.4 weeks in Group A and 17.2 weeks in Group B. The mean operation time was 45 minutes in Group A and 48 minutes in Group B. The mean radiation exposure times were 4.2 minutes and 4.8 minutes, respectively. VAS scores were 0.7 points and 0.5 points in each respective group. In Group A, the VAS score was 1.7 points when we applied pressure on the skin around the plate. The mean Olerud and Molander Ankle Score was 87.4 points and 86.3 points, respectively. A superficial wound infection occurred in 1 case in each group, and angular deformities more than 5 degrees occurred in 2 Group B cases.
CONCLUSION
No significant differences in results were observed between the two groups. However, a higher incidence of angular deformity was seen in the intramedullary nailing group. Therefore, we must be careful during surgery. -
Citations
Citations to this article as recorded by- Comparative Analysis of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing in the Treatment of the Distal Tibia Fractures
Ho-Min Lee, Young-Sung Kim, Jong-Pil Kim, Phil-Hyun Chung, Suk Kang, Kaung Suk Jo
Journal of the Korean Fracture Society.2018; 31(3): 94. CrossRef - A Comparison of the Results between Intramedullary Nailing and Minimally Invasive Plate Osteosynthesis in Distal Tibia Fractures
Chul-Hyun Park, Chi-Bum Choi, Bum-Jin Shim, Dong-Chul Lee, Oog-Jin Shon
Journal of the Korean Orthopaedic Association.2014; 49(4): 285. CrossRef
- Comparative Analysis of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing in the Treatment of the Distal Tibia Fractures
- 625 View
- 0 Download
- 2 Crossref

- Treatment of the Trimalleolar Fracture Using Posterolateral Approach: Minimum 2-year Follow Up Results
- Gwang Chul Lee, Jun Young Lee, Sang Ho Ha, Jae Won You, Sang Hong Lee, Hong Moon Sohn, Ki Young Nam, Kwang Hyo Seo
- J Korean Fract Soc 2011;24(4):328-334. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.328
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the long term follow up results of treatment with posterolateral approach and to investigate its usefulness in the patients of trimalleolar fracture with posterior fragment which is above 25% of articular involvement.
MATERIALS AND METHODS
There were 34 cases of trimalleolar fracture in our hospital from May 2004 to April 2008. We investigated 20 patients who underwent operation with the posterolateral approach and over-2 years follow up cases. The mean follow up period was 34 (24~58) months. Preoperative posterior malleolar fragment involved above 25% of articular surface in all cases and displaced more than 2 mm in 11 cases. We analyzed the radiologic type of posterior malleolar fragments and evaluated the function and pain through AOFAS score and complications.
RESULTS
All cases showed primary union at mean 13.1 weeks. The complications are that partial ankylosis result of soft tissue contracture is seen in 2 cases (10%) and post-traumatic arthritis is seen in 1 cases (5%) and 17 cases (85%) of all patients are showed excellent AOFAS score.
CONCLUSION
The posterolateral approach is a valuable method because that it enables us to easily reduction and internal fixation of the posterior malleolus and lateral malleolus at one time and the results are satisfied for a long time follow up. -
Citations
Citations to this article as recorded by- Outcomes of Immediate Operative Treatment of Ankle Trimalleolar Open Fractures
Jun-Young Lee, Yong-Jin Cho, Sin-Wook Kang, Yung-Min Cho, Hyun-Bai Choi
Journal of Korean Foot and Ankle Society.2020; 24(1): 25. CrossRef
- Outcomes of Immediate Operative Treatment of Ankle Trimalleolar Open Fractures
- 675 View
- 3 Download
- 1 Crossref

- Intra-articular Calcaneal Fractures Treated with Open Reduction and Internal Fixation: A Comparative Study between Groups with and without Bone Graft
- Hong Moon Sohn, Sang Ho Ha, Jun Young Lee, Sung Hwan Jo, Hoon Yang
- J Korean Fract Soc 2010;23(2):180-186. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.180
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study compares the clinical results of open reduction and internal fixation with and without bone graft for the treatment of intra-articular calcaneal fractures.
MATERIALS AND METHODS
Twenty-five patients who had open reduction and internal fixation for intra-articular calcaneal fractures and available for at least 1 year of follow-up were included in this study. Fifteen cases were operated with bone graft. Period to bone union and functional evaluation score were compared between both groups with analysis of complications.
RESULTS
Bone union was achieved in all cases with average bone union time of 11.6 weeks and 12.8 weeks in group with and without bone graft respectively. Creighton-Nebraska Health Foundation (CNHF) functional score was 86.5 points and 80.3 points respectively. The period to bone union and the CNHF score in the comparison of two groups were statistically insignificant. Complications were observed in four cases of group without bone graft and 5 cases of group with bone graft.
CONCLUSION
This study indicates that bone graft does not play a significant role in bone union and functional outcome when intra-articular calcaneal fractures are treated with open reduction and internal fixation. -
Citations
Citations to this article as recorded by- Surgical Treatment for Displaced Intra-Articular Calcaneal Fractures
Chul Hyun Park, Oog Jin Shon
Journal of the Korean Fracture Society.2016; 29(3): 221. CrossRef
- Surgical Treatment for Displaced Intra-Articular Calcaneal Fractures
- 707 View
- 1 Download
- 1 Crossref

- Treatment of Proximal Tibia Fractures Using LCP by MIPO Technique
- Sang Ho Ha, Dong Hui Kim, Jun Young Lee
- J Korean Fract Soc 2010;23(1):34-41. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.34
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We wanted to evaluate the efficacy of MIPO (minimal invasive plate osteosynthesis) technique by LCP (locking compression plate) for treating proximal tibia fractures.
MATERIALS AND METHODS
Twenty-three patients, who had operation due to proximal tibia fracture and available for follow up for more than 1 year were included in this study. Cause of injury and accompanied injuries were checked. Operation time, period to bone union, range of joint motion and alignment were evaluated with complications.
RESULTS
Mean bone union time was 13.7 weeks (10~20). Twenty-one cases of the patients showed angulation of less than 5 degrees and 17 cases had normal range of motion. Five cases showed skin irritation by the plate and 2 cases had superficial infection.
CONCLUSION
LCP by MIPO technique for treating proximal tibia fracture showed excellent results. Delicate technique is required for the proper adjustment of LCP and the alignment of the lower leg. -
Citations
Citations to this article as recorded by- EVALUATION OF FUNCTIONAL OUTCOME OF SURGICAL TREATMENT FOR FRACTURE AROUND KNEE WITH LOCKING PLATE
VIKAS KUNTWAD, AMOL WAGH, SATYAJEET A HORE
Asian Journal of Pharmaceutical and Clinical Research.2023; : 213. CrossRef - Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
Jae-Ang Sim, Kwang-Hui Kim, Yong-Seuk Lee, Sang-Jin Lee, Beom-Koo Lee
Journal of the Korean Orthopaedic Association.2014; 49(4): 278. CrossRef - Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures - Technical Note -
Jae Ang Sim, Beom Koo Lee, Kwang Hui Kim, Yong Seuk Lee
Journal of the Korean Fracture Society.2013; 26(4): 327. CrossRef
- EVALUATION OF FUNCTIONAL OUTCOME OF SURGICAL TREATMENT FOR FRACTURE AROUND KNEE WITH LOCKING PLATE
- 1,025 View
- 13 Download
- 3 Crossref

- Limited Open Reduction and Intramedullary Nailing of Proximal Femoral Shaft Fracture
- Sang Ho Ha, Jun Young Lee, Sang Hong Lee, Sung Hwan Jo, Jae Cheul Yu
- J Korean Fract Soc 2009;22(4):225-231. Published online October 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.4.225
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the result of treatment of proximal femoral shaft fracture with limited open reduction and intramedullary nailing. MATERIALS AND METHODS: Fifteen patients who had limited open reduction and intramedullary nailing due to proximal femoral shaft fracture for follow-up for more than 12 months were selected between March 2001 and December 2005. The clinical and radiologic results were analyzed. Winquist-Hansen classification and OTA/AO classification were used. RESULTS: Thirteen cases achieved bone union and 2 cases showed delayed union. The mean bone union period was 21.3 weeks (14~32). There was no postoperative infection. Nonunion was observed in 2 cases of which bone union was acquired with the exchange of intramedullary nail and bone graft in one case and with the additional plate fixation and bone graft in the other case. CONCLUSION: Treating proximal femoral shaft fracture with limited open reduction and intramedullary nailing seems to be a technique to manage proximal femoral shaft fracture that has combined fracture or ipsilateral femoral fracture or is unable to acquire acceptable reduction with closed reduction.
- 766 View
- 2 Download

- Treatment of Intra-articular Calcaneal Fractures Using Minimally Invasive Sinus Tarsi Approach in Diabetic Patients
- Hong Moon Sohn, Sang Ho Ha, Sang Hong Lee, Jun Young Lee, Jeong Ho Kim, Sang Jun Lee
- J Korean Fract Soc 2008;21(3):195-199. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.195
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Wound problems occur in 5~30% of intra-articular calcaneal fractures following operation. Diabetes mellitus, large incisions and abundant dissection can increase the risk of wound problems that may require skin graft or other additional care. The authors used minimally invasive technique to treat intra-articular calcaneal fractures in diabetic patients and evaluated the results and complications of this method. MATERIALS AND METHODS: Between January 2002 and July 2005, 12 patients with intra-articular calcaneal fractures who had underlying diabetes mellitus were treated using minimally invasive technique with a modified sinus tarsi approach. The patients had an average age of 47 years (39~67) and were followed an average of 19 months (13~32). The mean period between injury and operation was 8 days (5~14). Crutch assisted partial weight bearing was advised for an average of 7.3 weeks (6~9) and full weight bearing was allowed after average of 9.3 weeks (7~11).
RESULTS
According to AOFAS scale for ankle and hindfoot, patients had the following results: excellent - 1 patient (8%), good - 9 patients (75%), fair - 1 patient (8%), unsatisfied - 1 patient (8%). Bone union was achieved in all cases and there were no events of deep infection or skin necrosis.
CONCLUSION
Treating intra-articular calcaneal fractures by minimally invasive technique is an excellent operative method for patients with diabetes mellitus, as this method can minimize soft tissue incision and resulting deep infection and skin necrosis.
- 569 View
- 2 Download

- The Comparison of Radiographic Parameters and Clinical Results after Operative Treatment of Displaced Intraarticular Calcaneal Fractures
- Hong Moon Sohn, Jun Young Lee, Sang Ho Ha, Sueng Hwan Jo
- J Korean Fract Soc 2007;20(3):227-232. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.227
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the relationship between radiographic parameters and clinical results after operative treatment of the displaced intra-articular calcaneal fractures.
MATERIALS AND METHODS
We analyzed 35 patients of unilateral displaced intraarticular calcaneal fractures who had operative treatment with minimum follow up of 1 year. At the last follow up, we measured the radiographic parameters including Bohler angle, Gissane angle, heel height, calcaneal length, talocalcaneal angle, talar declination angle, subtalar incongruity between normal and affected site. Clinical results were measured by Creighton-Nebraska Health Foundation Assessment Score (CNH). The correlation between the radiographic parameters and the clinical results were analysed by Pearson correlation method.
RESULTS
Among the all radiographic parameters we analyzed, only subtalar incongruity shows strong negative linear correlation with clinical results. The average difference of subtalar incongruity between normal and affected site was 0.54 mm (0~2.5) and the correlation coefficients with CNH score was -0.784 (p=0.002).
CONCLUSION
We suggest that the subtalar incongruity is significantly correlated with the clinical results after operative treatment of the displaced intraarticular calcaneal fractures. -
Citations
Citations to this article as recorded by- Results in Operative Treatment of Open Calcaneal Fracture
Ba Rom Kim, Jun Young Lee, Donghyuk Cha
Journal of Korean Foot and Ankle Society.2021; 25(3): 133. CrossRef - Measurement of Normal Calcaneus in Korean Cadavers: A Preliminary Report
Jung-Han Kim, Heui-Chul Gwak, Jeon-Gyo Kim, Yang Hwan Jung
Journal of Korean Foot and Ankle Society.2014; 18(1): 14. CrossRef
- Results in Operative Treatment of Open Calcaneal Fracture
- 538 View
- 2 Download
- 2 Crossref

- Treatment of Senile Osteoporotic Intertrochanteric Fracture using Proximal Femoral Nail
- Dong Hui Kim, Sang Hong Lee, Young Lae Moon, Jun Young Lee, Kun Sang Song
- J Korean Fract Soc 2007;20(3):215-221. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.215
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Clinical and radiologic results of femur intertrochanteric fractures treated with ITST nail in elderly patients with osteoporosis were analysized to evaluate the efficacy and complication of ITST nailing.
MATERIALS AND METHODS
32 patients who were treated with ITST nail due to femur intertrochanteric fracture and were followed up for more than 1 year were analysed. According to Evans classification, 11 cases were stable fractures and 21 cases were unstable fractures. Clinically, ambulatory function was compared and radiologically, BMD of healthy leg was checked with analysis of postoperative bone union and complication.
RESULTS
In ambulatory function comparison before and after the operation, there were 9 cases of good, 17 cases of moderate and 6 cases of poor. Considering social activity after the operation, 7 cases showed normal ambulation, 9 cases showed ambulatory with one cane, 5 cases showed two cane ambulation and 11 cases showed dependent ambulation. In radiologic evaluation, T-score of ward triangle in healthy femoral neck showed BMD of -3.12. In 20 cases, bone union was observed within 3 months. The patients with low BMD result had poor outcome. There were 2 cases of intraoperative proximal femur fracture, 3 cases of nonunion and 4 cases of death within 1 year.
CONCLUSION
In elderly patients with intertrochanteric fracture, ITST nailing is relatively efficient treatment. However, in pateint with severe osteoporosis (T-score<-3.0) and unstable fracture pattern, arthroplasty should be considered due to relatively high complicaton rate. -
Citations
Citations to this article as recorded by- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
Journal of the Korean Fracture Society.2011; 24(3): 217. CrossRef - Results of Osteoporotic Treatment Drug after Periarticular Fracture of Hip
Soo Jae Yim, Young Koo Lee, Cheong Kwan Kim, Hyun Seok Song, Hee Kyung Kang
Journal of the Korean Fracture Society.2010; 23(2): 167. CrossRef
- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
- 835 View
- 2 Download
- 2 Crossref

- Treatment of High-energy Distal Tibia Intraarticular Fractures with Two-staged Delayed Minimal Invasive Plate Osteosynthesis
- Hong Moon Sohn, Jun Young Lee, Sang Ho Ha, Jae Won You, Sang Hong Lee, Kwang Chul Lee
- J Korean Fract Soc 2007;20(1):19-25. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.19
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the short-term results of two-staged delayed minimal invasive plate osteosynthesis in high-energy intraarticular fractures of the distal tibia.
MATERIALS AND METHODS
Thirteen patients, who underwent two-staged delayed minimal invasive plate osteosynthesis for intraarticular fractures of the distal tibia between January 2002 and July 2004, were followed for more than one year. The mean interval time between first stage and second stage of the procedures was 28.6 days (range, 14~34 days). By Ruedi-Allgower classification, there were two cases in type I, three cases in type II, and eight cases in type III. There were six cases in type B and seven cases in type C patients according to AO/OTA classification. Radiographs were graded by the criteria of Burwell and Charnley and ankle functions were graded by the criteria of Mast and Teipner. Union time and postoperative complications were also analysed.
RESULTS
Average union time was 16.9 weeks (range, 14~20 weeks) in twelve of the thirteen fractures, but there was one fracture resulting in soft tissue complication and infected nonunion. At the latest follow-up, review of the radiographic results showed that ten cases of fractures (77%) achieved an anatomic reduction, two cases (15%) achieved fair reduction and one case (8%) achieved a poor reduction. And clinical functional assessment showed that nine cases (69%) were good results, three cases were (23%) fair results and one case (8%) was poor result.
CONCLUSION
Two-staged delayed minimal invasive plate osteosynthesis is an excellent option for the treatment of high-energy intraarticular fractures of the distal tibia. -
Citations
Citations to this article as recorded by- Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
Sung-Ki Park, Chang-Wug Oh, Jong-Keon Oh, Kyung-Hoon Kim, Woo-Kie Min, Byung-Chul Park, Won-Ju Jeong, Joo-Chul Ihn
Journal of the Korean Fracture Society.2010; 23(3): 289. CrossRef - The Comparison of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing in the Treatment of the Proximal and Distal Tibia Fracture
Joon Soon Kang, Seung Rim Park, Sang Rim Kim, Yong Geun Park, Jae Ho Jung, Sung Wook Choi
Journal of the Korean Fracture Society.2010; 23(2): 172. CrossRef - Two-staged Delayed Minimally Invasive Percutaneous Plate Osteosynthesis for Distal Tibial Open Fractures
Jung Hwan Yang, Seok Hyun Kweon, Jeung Woo Kim, Jin Young Park, Hyun Jun Kim, Chul Min Lim
Journal of the Korean Fracture Society.2008; 21(1): 24. CrossRef
- Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
- 628 View
- 2 Download
- 3 Crossref

- Delayed Operative Treatment of Long Bone Fractures in Patients with Brain Injury
- Hong Moon Sohn, Sang Ho Ha, Jun Young Lee, Young Kwan Lee
- J Korean Fract Soc 2006;19(2):157-162. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.157
-
 Abstract
Abstract
- PURPOSE
To evaluate the postoperative progress and outcomes of bone injured patients with long bone fracture showing callus formation and deformity due to delayed surgical treatment.
MATERIALS AND METHODS
10 cases with more than 1 year follow up were chosen from 12 patients with long bone fracture whose surgical treatment was delayed due to brain injury. Exuberant callus formation and deformations were observed. Average delayed period was 6.7 weeks (4~10 weeks). Preoperative callus formation, shortening and angulation were evaluated using plain radiographs. Total operation time and transfusion amount were compared with that from operations done within 2 weeks following accident. Postoperative bone union was checked.
RESULTS
In all cases, preformed angulation and hypertrophic ossification made reduction difficult and this increased total operation time and transfusion amount but had no statistical importance. In patients with humerus and femur fractures accompanying brain injury, massive hypertrophic ossification was observed both in preoperative period and in postoperative period. Average bone union period was 13.5 weeks in humerus fractures, 17.9 weeks in femur fractures. The bone union period was shorter in subject group but had no statistical importance.
CONCLUSION
Early surgical treatment is essential to patients with long bone fracture accompanying brain injury but if early surgical treatment can not be done, proper immobilization to fracture site should be done. -
Citations
Citations to this article as recorded by- Alterations in Serum Levels of Receptor Activator of Nuclear Factor-κB Ligand and Osteoprotegerin in Patients with Head Injury and Fracture
Shin Young Park, Kuen Tak Suh, Chang Hoon Ryu, Seung Hun Woo, Jung Sub Lee, Seong-Gang Kim
Journal of the Korean Fracture Society.2008; 21(2): 145. CrossRef
- Alterations in Serum Levels of Receptor Activator of Nuclear Factor-κB Ligand and Osteoprotegerin in Patients with Head Injury and Fracture
- 925 View
- 0 Download
- 1 Crossref

- Ender Nailing of the Tibial Shaft Fractures under the Local Anesthesia
- Sang Ho Ha, Jun Young Lee, Deog Yong Kim
- J Korean Fract Soc 2006;19(2):147-152. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.147
-
 Abstract
Abstract
- PURPOSE
To evaluate the clinical result of ender nailing under local anesthesis was done to patient with tibia shaft fracture who had high risk for general anesthesia or spinal anesthesia.
MATERIALS AND METHODS
10 cases with ender nailing procedure under local anesthesia due to high anesthetic risk were selected from total of 20 cases with tibia shaft fracture operated with ender nailing. In each patient, hepatic, diabetic, cadiopulmonary complication and thromboembolism which can be initiated or aggravated by general or spinal anesthesia, were evaluated. Radiologic and clinical evaluation were used to check bone union.
RESULTS
There were no complication of local anesthesia. Bone union were acquired in all cases with average bone union period of 18 weeks. There were no evidence of flexion deformity, limb shortening or joint contracture.
CONCLUSION
Ender nail fixations under local anesthesia enable close reduction and intramedullary nailing and is effective in patient care but has no problem with bone union. For this reason, ender nail fixation under local anesthesia seem to be effective method if general of spinal anesthesia is difficult.
- 431 View
- 0 Download

- Treatment of Distal Femoral Shaft and Supracondylar Fracture with aRetrograde Intramedullary Nailing
- Sang Hong Lee, Jun Young Lee, Sang Ho Ha, Hong Moon Sohn, Kwang Chul Lee
- J Korean Fract Soc 2004;17(2):103-109. Published online April 30, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.2.103
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Retrograde intramedullary nailing has been recommended as one of the treatment options for the distal femoral fracture, particularly in patients who are obese, are pregnant, has sustained ipsilateral femoral neck fracture, have multiple injuries. However there are some disadvantage such as post-arthrotomy infection, knee joint stiffness. This paper is to evaluate the result and complication of treatment of distal femoral fracture with a retrograde intramedullary nailing.
MATERIALS AND METHODS
We reviewed 13 cases (distal femoral shaft fracture: 6 cases, supracondylar fracture: 7 cases) of the distal femoral fracture who had been treated with retrograde intramedullary nailing and follow up for more than 12 months from January 1999 to December 2001. The rate of bony union, range of motion of the knee, complications were evaluated.
RESULTS
The mean duration of bony union was 20 weeks (range, 16~25 weeks). A case of delayed union was developed. In 4 cases of 13 cases showed posterior angulation below 6 degree, which did not need further treatment. According to Saunder's criteria, excellent result was achieved in 8 patients, good result in 5 patients, respectively.
CONCLUSION
This study showed good clinical and radiological results of union with retrograde intramedullary nailing at the distal femoral fracture and ipsilateral multiple fracture -
Citations
Citations to this article as recorded by- Analysis of Risk Factors for Nonunion after Intramedullary Nailing of Femoral Shaft Fracture in Adult
Yong-Woon Shin, Yerl-Bo Sung, Jeong Yoon Choi, Minkyu Kim
Journal of the Korean Fracture Society.2011; 24(4): 313. CrossRef - Axial Malalignment after Minimally Invasive Plate Osteosynthesis in Distal Femur Fractures with Metaphyseal Comminution
Jae-Ho Jang, Gu-Hee Jung, Jae-Do Kim, Cheung-Kue Kim
Journal of the Korean Orthopaedic Association.2011; 46(4): 326. CrossRef
- Analysis of Risk Factors for Nonunion after Intramedullary Nailing of Femoral Shaft Fracture in Adult
- 547 View
- 0 Download
- 2 Crossref

- Surgical Treatment for the Non-union of the Lateral Humeral Condyle Fracture using Closing Wedge Osteotomy and Bone Graft
- Sang Ho Ha, Hong Moon Sohn, Jun Young Lee, Sun Jong Oh
- J Korean Soc Fract 2003;16(3):379-384. Published online July 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.3.379
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical results of the surgical treatment for established nonunion of lateral humeral condyle fracture using closing wedge osteotomy and bone graft.
MATERIALS AND METHODS
Six patients diagnosed as symptomatic established nonunion of lateral humeral condyle fracture and cubitus valgus deformity were reviewed retrospectively. The average age was 23 years old and mean follow up period was 32 months. We investigate the changes of the symptoms and radiographic findings, and determine the results by Oppenheim's criteria.
RESULTS
According to Oppenheim's criteria, 3 patients showed excellent, 2 good, 1 poor. Carrying angle is improved to 10.2 degrees and range of motion was decreased by mean 9 degrees. All of the patients' muscle weakness and pain were improved, and was achieved solid union at the last follow up.
CONCLUSION
In the treatment of symptomatic established lateral humeral fracture and cubitus valgus deformity, better functional and cosmetic results are anticipated by a closing wedge osteotomy and bone graft. -
Citations
Citations to this article as recorded by- In SituLate Metaphyseal Osteosynthesis for the Fractures of the Lateral Humeral Condyle in Children
Kun Bo Park, Seung Whan Lee, Hyun Woo Kim, Hui Wan Park, Ki Seok Lee
Journal of the Korean Fracture Society.2008; 21(2): 151. CrossRef
- In SituLate Metaphyseal Osteosynthesis for the Fractures of the Lateral Humeral Condyle in Children
- 535 View
- 2 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


