Search
- Page Path
- HOME > Search
Review Articles
- Complications of hand fractures: strategies for prevention and management
- Jong Woo Kang
- J Musculoskelet Trauma 2026;39(1):1-11. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00304

-
 Abstract
Abstract
 PDF
PDF - Various complications can occur after hand fractures. Among them, joint stiffness and malunion are the most common and significant complications, which are often accompanied by tendon adhesions and joint contracture. Careful evaluations of injury characteristics, such as fracture patterns, alignment, and soft tissue injury, are the first step to select appropriate management strategies and prevent complications of hand fractures. Close observation of its clinical prognosis is also essential for early detection and preemptive management of complications. Management of complications includes immobilization, rehabilitation, and various surgical techniques such as tenolysis or capsular release for joint stiffness, corrective osteotomy for malunion, and revisional fixation with bone graft for nonunion. The authors discuss prevention, early recognition, and management strategies for complications of hand fractures in this review.
- 322 View
- 11 Download

- Innovative applications of artificial intelligence in orthopedics focusing on fracture and trauma treatment: a narrative review
- Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(4):178-185. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00283
-
 Abstract
Abstract
 PDF
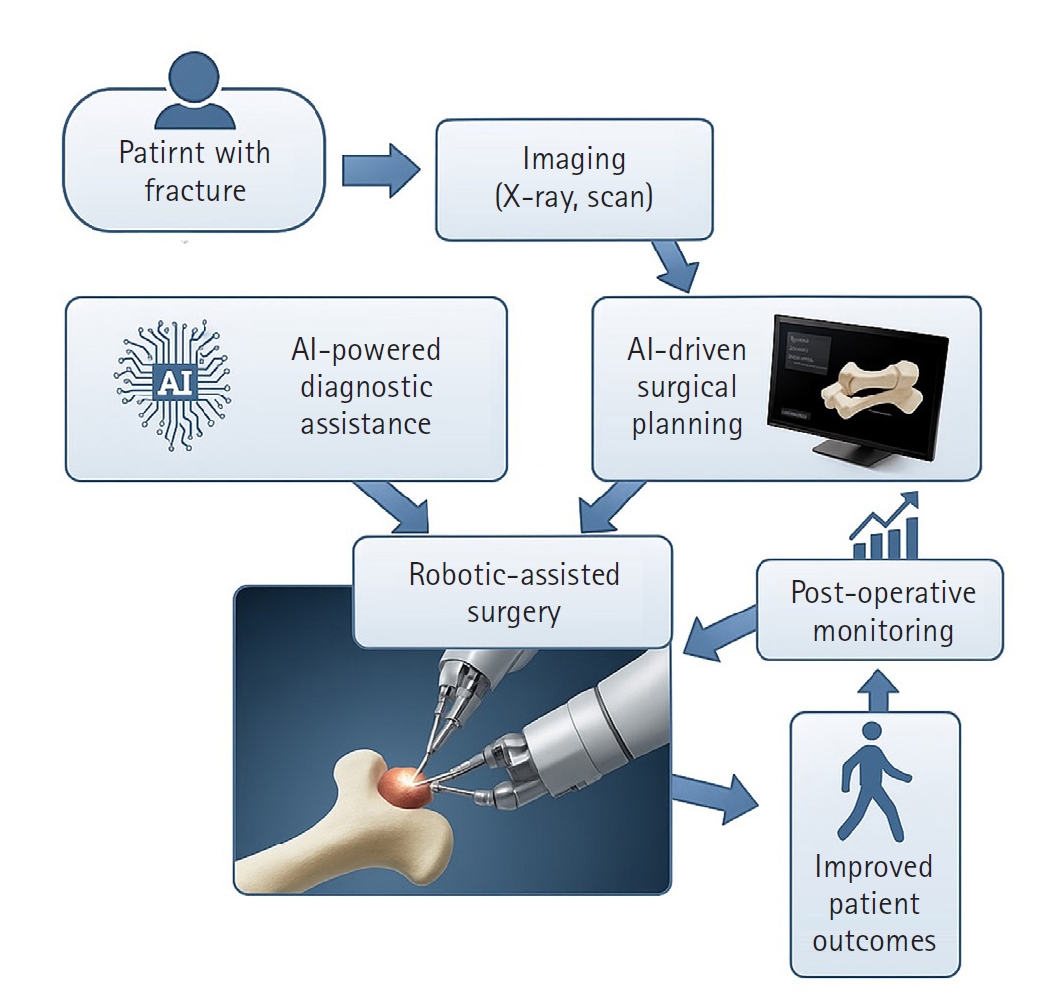
PDF - Artificial intelligence (AI) is bringing about transformative changes in orthopedic surgery, with its potential being particularly prominent in the field of fracture and trauma treatment. This review explores the current applications and future prospects of AI-driven surgical planning and simulation, robot and image-based navigation surgery, and image-assisted diagnostic technologies. Robotic assistance in orthopedic surgery, which was initially applied to improve accuracy in component implantation for knee and hip arthroplasty and to achieve high precision in spinal screw placement, has recently expanded its use to include accurate, minimally invasive reduction of pelvic fractures. In diagnostics, AI aids in the early prediction and classification of ambiguous fractures in various anatomical regions—for example, detecting shoulder or hip fractures, identifying incomplete atypical femur fractures, and classifying femoral neck fractures—through X-ray image analysis. This improves diagnostic accuracy and reduces medical costs. However, significant challenges remain, including high initial costs, steep learning curves, a lack of long-term studies, data bias, and ethical concerns. Continued research, interdisciplinary collaboration, and policy support are crucial for the widespread adoption of these technologies.
- 969 View
- 2,147,483,661 Download

Original Article
- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- Hyun-Jae Park, Joo-Hak Kim
- J Musculoskelet Trauma 2025;38(4):221-228. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00241
-
 Abstract
Abstract
 PDF
PDF - Background
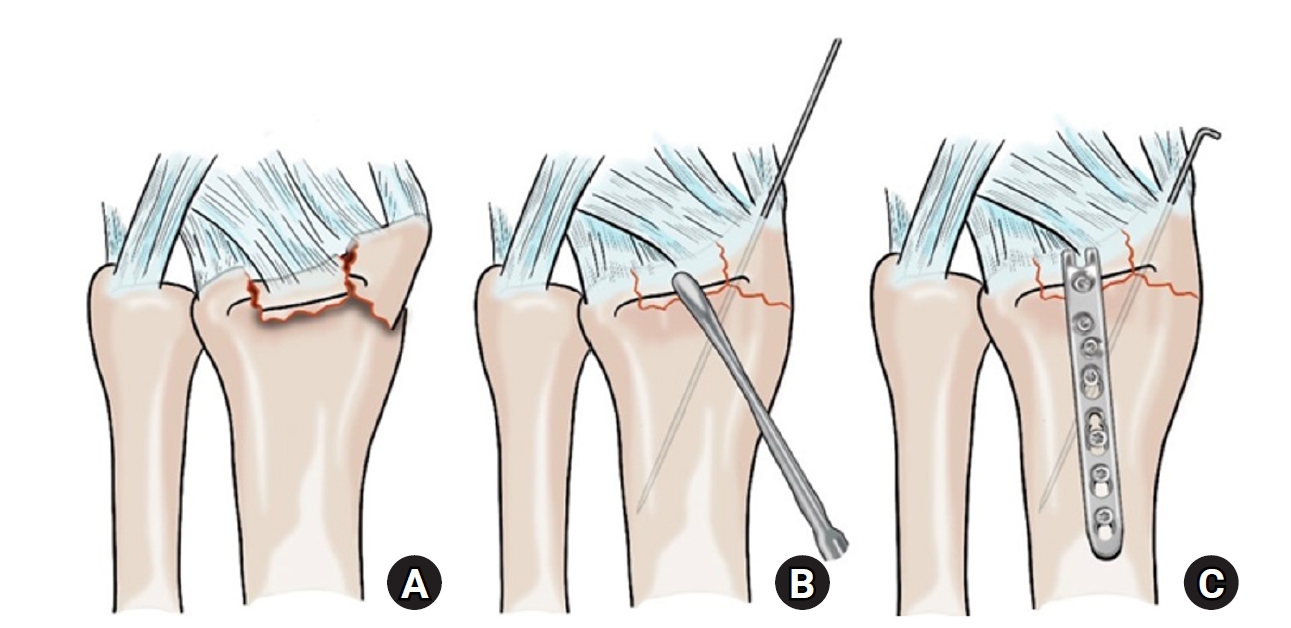
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures. Level of evidence: IV.
- 382 View
- 11 Download

Case Report
- Two-Year Follow-Up Results after Tendon Graft and Corrective Osteotomy for the Delayed Rupture of the 2nd-5th Flexor Tendons due to a Malunion of a Distal Radius Fracture - A Case Report -
- Jeung-Hwan Seo, Hyun-Gon Gwak, Jae Hoon Lee
- J Korean Fract Soc 2022;35(2):63-67. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.63
-
 Abstract
Abstract
 PDF
PDF - The delayed rupture of the flexor tendons is a rare complication of malunited distal radius fractures after nonoperative management. The known cause of a flexor tendon rupture is attrition between the palmarly displaced ulnar head and the involved tendons. Sharp bony spurs on the volar side of the malunited distal radius can also cause flexor tendon rupture. About 30 cases have been reported in literature. There were only four case reports about the delayed rupture of the 2nd, 3rd, 4th, and 5th flexor tendons. In this case, we experienced flexor digitorum superficialis and flexor digitorum profundus tendon ruptures of the index, middle, ring, and little fingers, after 8 months following the malunion of a distal radius fracture. At two years follow-up after tendon graft and corrective osteotomy, the range of motion and motor weakness of the 2nd, 3rd, 4th, and 5th fingers improved.
- 461 View
- 2 Download

Review Article
- Diagnosis and Management of Ligament Injuries of the Wrist
- Ki Tae Na, Joo Yup Lee
- J Korean Fract Soc 2016;29(2):160-170. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.160
-
 Abstract
Abstract
 PDF
PDF - The wrist joint is formed by the distal end of the radius and ulna proximally, and eight carpal bones distally. It has many ligaments to maintain stability of the complex bony structures. The incidence of ligament injuries of the wrist has increased due to sports activities. However, diagnosis and management of these injuries are sometimes difficult because of the anatomic complexity and variable injury patterns. Among them, scapholunate ligament injury and triangular fibrocartilage tears are the two most common injuries resulting in chronic disabling wrist pain. Thorough understanding of the wrist anatomy and physical and radiologic examination is mandatory for proper diagnosis and management of these conditions. This article will briefly discuss the wrist joint anatomy and biomechanics, and review the diagnosis and management of the scapholunate ligament injury and triangular fibrocartilage injury.
- 1,075 View
- 16 Download

Original Articles
- Treatment of Type IIIb Open Tibial Fractures
- Seong Yeon Lim, Il Jae Lee, Jae Ho Joe, Hyung Keun Song
- J Korean Fract Soc 2014;27(4):267-273. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.267
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the outcome of treatment for patients with Type IIIb open tibial fractures.
MATERIALS AND METHODS
This study targeted 35 adult patients for whom follow-up was possible over one year after undergoing surgical treatment. There were 29 males and six females with an average age of 45 years.
RESULTS
Fracture location was proximal in 10 cases, midshaft in 13 cases, and the distal part of the tibia in 12 cases. An average of 10 days was observed for definitive fixation with soft tissue coverage of the injury. The mean time to radiographic union was 27 weeks. Sixteen cases (45.7%) of complications were observed. Three cases of superficial infection, two cases of deep infection, four cases of partial flap necrosis, three cases of mal-alignment, three cases of joint stiffness, and one case of hardware breakage were observed. The mean lower extremity functional scale score was 68.5 and the factors influencing the clinical results were severity of open wound (p=0.000) and occurrence of complications (p=0.000) according to results of multiple regression analysis.
CONCLUSION
In treatment of Type IIIb open tibial fractures, good clinical results can be expected provided that complications are prevented through proper reduction, firm fixation, early soft tissue reconstruction, and early rehabilitation. -
Citations
Citations to this article as recorded by- Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
Jung Min Lee, Eun-Jung Lee
Journal of Korean Medicine Rehabilitation.2020; 30(3): 141. CrossRef
- Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
- 1,155 View
- 6 Download
- 1 Crossref

- Analysis of Elbow Injuries 'pattern in Children
- Soon Hyuck Lee, Jong Woong Park, Sang Won Park, Kwang Suk Lee, Dang Jae Im, Tae Ha Kim, Sang Won Lee
- J Korean Soc Fract 2003;16(1):98-103. Published online January 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.1.98
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this report is to describe the pattern of elbow injuries and the incidence of the different fracture types in children.
MATERIALS AND METHODS
The records of 445 in-patient children treated for the elbow injuries for 5 years were reviewed and analyzed statistically.
RESULTS
The average age of 445 children was 6.7 years. The average age of boys(6.9 years) was about 1 year older than girls(5.9 years). The age group of 4 - 7 years is the majority(50%), followed by the age group of 8 - 11 years(22%). The boy to girl ratio was approximately 2:1. The male predominance changed with the age and appeared dramatically in the age group of 12-16 years( 6.7:1 ). Left elbow was injured more frequently(60%). Left side predominance was accentuated in girls compared to boys(69% vs 55%), especially in the age group of 8 - 16 years (80% vs 50%). Thirty percent of the fractures occurred during the summer, followed by 27% the autumn, 26% the spring months and 17% the winter. The most common fracture was the supracondylar fractures of the humerus(52.3%), followed by lateral condylar fractures(25.4%), olecranon fractures(5.3%), radial head fractures(4.8%), medial epicondyle fractures(4.6%), transphyseal fractures(2.8%) and Monteggia fractures(2.2%). Medial condylar fractures(1.1%) and elbow dislocation(0.8%) were rare injuries. The average age was higher in radial head fracture(10.6 years) and medial epicondylar fracture(12.4years). Closed reduction and percutaneous pinning was the method of treatment in more than half(52%). Open reduction was performed in 32%. Sixteen percent was treated by closed reduction and cast immobilization.
CONCLUSION
The incidence and pattern of elbow injuries in children, which needed operative treatment in the majority, occured closely correlated with the amount of injury prone play and the pattern of behavior during the causative accidents.
- 317 View
- 0 Download

- Neural Injuries in Elbow Fracture in Children
- Kyung Chul Kim, Bon Sub Koo, Hae Du Sung
- J Korean Soc Fract 1997;10(2):388-392. Published online April 30, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.2.388
-
 Abstract
Abstract
 PDF
PDF - Due to the unique anatomical characteristics of elbow, it is well known that fracture involving elbow joint, relatively common in children, frequently accompanies nerve injuries. In recent studies, most of these injury are reported to be resolved within average 2~3months spontaneously. The authors reviewed 91 elbow fractures revealing 9 neural injuries in children at Kangbuk Samsung Hospital from January 1990 to December 1995 retrospectively. These injuries occurred in 9 patient whose age ranged from 5~8 years. The overall incidence of neural injuries appeared to be around 9.8%. There were three radial, three ulnar, two interosseous, one median neuropathies detected. Two of the ulnar nerve injuries were iatrogenic, resulting from closed reduction and percutaneous pinning. All of the deficit, resolved spontaneously within a range 1~7 months(average 2.6months).
- 343 View
- 1 Download

- Injuries of the Tarsometatarsal Joint
- Chong Il Yoo, Jeung Tak Suh, Kuen Tak Suh, Yong Jin Kim, Hui Taeg Kim, Kie Bong Wang
- J Korean Soc Fract 1992;5(2):219-226. Published online November 30, 1992
- DOI: https://doi.org/10.12671/jksf.1992.5.2.219
-
 Abstract
Abstract
 PDF
PDF - Because of the anatomical configuration of the tarsornetatarsal joints with their strong ligmanet connections, the injries in this regicon are rare. But the injury is associated with a high potential for chronic disability.Authors reviewed and clinically analysed 18 cases of tarsometatarsal joint injuries which were followed more than one year at the orthopedic department of Pusan National University durging the period from January 1986 to December 1990. The results were as follows ; 1. The incidence was higher in male and young active age group. 2. The most common cause of the injury was traffic accident (50.0%). 3. Tarsal and metatarsal fractures were commonly combined (61.1%) 4. The most frequent injury type by Hardcastles classification was total inconjgrulty type (55.5%). 5. Overall result estimated by Hardcastles criteria was good in 5 cases (27.8%), fair in 8 cases (44.4%), and poor in 5 cases (27.8%). 6. The causes of poor resulted cases were severe crushing injury, inadequate anatomical reduction, delayed treatment due to combind injury and loss of medial longitudinal arch. 7. Late complications such as traumatir arthrltis, paln and foot deformity were seen more than half of the cases.
- 396 View
- 0 Download

- A clinical study of ankle fractures
- In Hwan Jeong, Jeong Hwan Oh, Eui Hwan Ahn, Kyung Jong Ham
- J Korean Soc Fract 1991;4(2):347-355. Published online November 30, 1991
- DOI: https://doi.org/10.12671/jksf.1991.4.2.347
- 392 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


