Search
- Page Path
- HOME > Search
Original Articles
- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
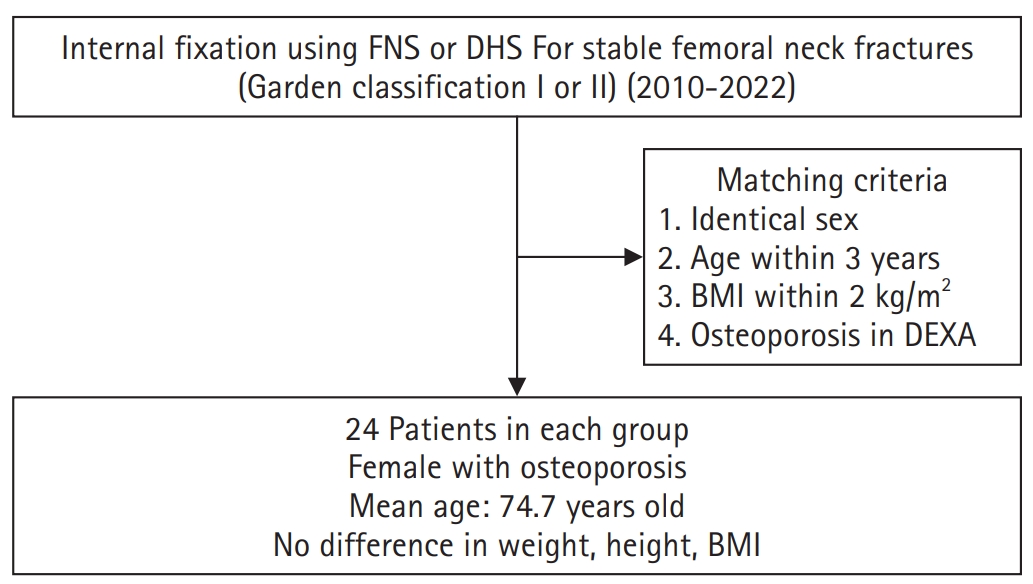
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,682 View
- 21 Download

- The Role of Beta-Tricalcium Phosphate Graft in the Dynamic Hip Screw Fixation of Unstable Intertrochanter Fracture
- Chul Ho Kim, Ji Wan Kim, Eic Ju Lim, Jae Suk Chang
- J Korean Fract Soc 2016;29(4):250-257. Published online October 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.4.250
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to introduce our method of stabilizing unstable intertrochanteric fractures by using the dynamic hip screw (DHS) with a beta-tricalcium phosphate (β-TCP) graft and to compare the outcomes of this procedure with those of the conventional DHS without β-TCP.
MATERIALS AND METHODS
Patients who underwent surgery by using DHS between March 2002 and January 2016 were retrospectively reviewed for analysis of the outcomes. The inclusion criteria were: 1) age of 60 years and older; 2) low-energy fracture resulting from a fall from no greater than the standing height; 3) multifragmentary pertrochanteric fracture (AO classification 31-A2.2, 2.3); and 4) follow-up of over 3 months. We compared 29 patients (29 hips) who underwent surgery, using DHS without β-TCP, with 29 age-sex matched patients (29 hips) who underwent surgery using DHS with grafted β-TCP granules to empty the trochanter area after reaming. We investigated the fracture union rate, union time, and length of lag screw sliding.
RESULTS
Bone union was achieved in all cases. The mean union time was 7.0 weeks in the β-TCP group and 8 .8 weeks in the non-β-TCP group. The length of lag screw sliding was 3.6 mm in the β-TCP group and 5 .5 mm in the non-β-TCP group. There were no implant failure cases in both groups.
CONCLUSION
The β-TCP graft for reinforcement DHS acquired satisfactory clinical outcomes for treating unstable intertrochanteric fractures.
- 437 View
- 3 Download

- Surgical Treatment for Stable 2-Part Intertrochanteric Femur Fracture Using Dynamic Hip Screw with 2-Hole Side Plate in Elderly Patients
- Kyung Hoon Lee, Suk Ku Han, Seung Jae Chung, Jongho Noh, Kee Haeng Lee
- J Korean Fract Soc 2016;29(3):192-199. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.192
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the postoperative outcomes of elderly patients with stable 2-part intertrochanteric femur fractures surgically treated using dynamic hip screw with 2-hole side plate.
MATERIALS AND METHODS
From February 2008 to January 2014, 50 patients older than the age of 65 years, who had been followed-up for more than 6 months after the operation at The Catholic University of Korea, Bucheon St. Mary's Hospital were enrolled. A clinical evaluation of the skin incision length, operating time, and ambulatory status, using Clawson's Ambulation Capacity Classification, was performed, and a radiologic evaluation of Fogagnolo reduction quality, tip-apex distance (TAD), Cleveland index, sliding extent of lag screws, time duration till bony union, and complications was also done.
RESULTS
The mean skin incision length was 9.8 cm (range, 8-13 cm), the mean operating time was 41.4 minutes (range, 30-60 minutes), and 32 patients recovered their ambulatory function. Forty-eight patients gained bony union, and the time lapsed till union was average 10.6 weeks (range, 8-16 weeks). The evaluation of postoperative radiologic images showed the following reduction statuses by the Fogagnolo classification: 46 cases of "Good", 3 cases of "Acceptable," and 1 case of "Poor." Moreover, the mean TAD was 18.9 mm (range, 9.0-24.9 mm). While 45 cases fit into the zone 5 of the Cleveland index, other 3 were within zone 8 and the other 2 were within zone 6. The mean sliding length of the lag screws were 4.9 mm (range, 0.1-19.4 mm). There were a case of nonunion and a case of periprosthetic infection with nonunion as complications.
CONCLUSION
Using dynamic hip screws with 2-hole side plate for stable 2-part intertrochanteric femur fractures in elderly patients showed satisfactory results with respect to the recovery of ambulatory functions and bony union.
- 466 View
- 0 Download

- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
- Byung Woo Min, Kyung Jae Lee, Gyo Wook Kim, Ki Cheor Bae, Si Wook Lee, Du Han Kim
- J Korean Fract Soc 2014;27(2):120-126. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.120
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study was to analyze the use of a compression hip screw with a trochanter stabilizing plate for treatment of reverse oblique intertrochanteric fractures.
MATERIALS AND METHODS
We reviewed the results of 33 cases of reverse oblique intertrochanteric fracture treated with a compression hip screw with a trochanter stabilizing plate from January 2000 to December 2012 which were followed-up for more than one year. We evaluated postoperative bone union period, change of neck-shaft angle, sliding of hip screw, and other complications.
RESULTS
Of 33 patients, satisfactory reduction was achieved in 28 patients. Five patients had an unsatisfactory reduction, with two cases of excessive screw sliding, one of broken metal, one of varus deformity, and one of internal rotation deformity. We performed corrective osteotomy in varus and internal rotation deformity and partial hip replacement in a case of excessive screw sliding. Bone union was achieved in 29 patients, and the average bone union period was 19.2 weeks.
CONCLUSION
We consider that a compression hip screw with a trochanteric stabilized plate is a good option for treatment of reverse oblique intertrochanteric femoral fractures. However, adequate fracture reduction and ideal implant placement are a basic necessity for successful treatment.
- 785 View
- 6 Download

- A Comparison between Compression Hip Screw and Intramedullary Nail for the Treatment of AO/OTA A2.2 Intertrochanteric Femoral Fracture
- Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Ho Min Lee, Jong Hyun Kim
- J Korean Fract Soc 2013;26(1):44-49. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.44
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the result between the compression hip screw (CHS) and intramedullary (IM) nail for the treatment of AO/OTA A2.2 intertrochanteric fracture.
MATERIALS AND METHODS
We retrospectively reviewed 95 cases of AO/OTA A2.2 intertrochanteric fracture, which were treated with CHS or IM nail by one surgeon from March 1994 to December 2009. One group was treated with CHS (Group I, 28 cases) and the other was treated with IM nail (Group II, 67 cases). We evaluated the mean operation time, the amount of bleeding and transfusion, hospital duration, radiological results and the clinical outcome with the mobility score of Parker and Palmer.
RESULTS
Radiologically, the tip-apex distance, change of neck-shaft angle, and union time were not significantly different between both groups (p>0.05). Clinically, the mean operation time, the amount of bleeding and transfusion, hospital duration and the mobility score were not significantly different (p>0.05). The post-operative complications were lag screw slippage over 25 mm (1 case) and loosening of device (1 case) in group I. In group II, there were perforation of the femoral head (1 case), nail breakage (1 case) and deep infection (1 case).
CONCLUSION
There was no significant differences that are clinical and radiological results in the treatment of AO/OTA A2.2 intertrochanteric fracture, using CHS and IM nail. -
Citations
Citations to this article as recorded by- A Comparison of Clinical Results between Compression Hip Screw and Proximal Femoral Nail as the Treatment of AO/OTA 31-A2.2 Intertrochanteric Femoral Fractures
Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Ho Min Lee, In Hwa Back, Kyeong Soo Eom
Journal of the Korean Orthopaedic Association.2016; 51(6): 493. CrossRef
- A Comparison of Clinical Results between Compression Hip Screw and Proximal Femoral Nail as the Treatment of AO/OTA 31-A2.2 Intertrochanteric Femoral Fractures
- 1,659 View
- 2 Download
- 1 Crossref

- Surgical Treatment of Femoral Unstable Intertrochanteric Fractures in Elderly Patients: Comparative Study between Compressive Hip Screws and Additional Trochanteric Stabilizing Plates
- Kap Jung Kim, Dae Suk Yang, Sang Ki Lee, Won Sik Choy, Kyoung Wan Bae
- J Korean Fract Soc 2011;24(4):295-300. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.295
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the radiologic results between compressive hip screw and compressive hip screw with additional trochanteric stabilizing plate in patients with femoral unstable intertrochanteric fractures in patients with more 65 years old.
MATERIALS AND METHODS
From 2006 to May 2009, 121 cases were included. Group I (compressive hip screw only) was 54 cases and group II (compressive hip screw with trochanteric stabilizing plate) was 67 cases. We checked the lag screw sliding, lateral translation of greater trochanter, changes of neck-shaft angle and complications through periodic follow up of radiographs.
RESULTS
Mean lag screw sliding was 7.6 mm in group I and 3.9 mm in group II (p=0.001). Mean lateral translation of greater trochanter was 3.86 mm in group I and 0.59 mm in group II (p=0.01). Mean changes of neck-shaft angle was nearly the same, 3.57degrees in group I and 3.66degrees in group II. Complications were 15 cases in group I and 10 cases in group II.
CONCLUSION
Compressive hip screw with additional trochanteric stabilizing plate was effective surgical option in patients with femoral unstable intertrochanteric fractures in patients with more than 65 years old. It decreased lag screw sliding, lateral translation of greater trochanter and complication rates. -
Citations
Citations to this article as recorded by- The Role of Beta-Tricalcium Phosphate Graft in the Dynamic Hip Screw Fixation of Unstable Intertrochanter Fracture
Chul-Ho Kim, Ji Wan Kim, Eic Ju Lim, Jae Suk Chang
Journal of the Korean Fracture Society.2016; 29(4): 250. CrossRef
- The Role of Beta-Tricalcium Phosphate Graft in the Dynamic Hip Screw Fixation of Unstable Intertrochanter Fracture
- 715 View
- 1 Download
- 1 Crossref

- Comparison of the Compression Hip Screw (CHS) and the Proximal Femoral Nail Antirotation (PFNA) for Intertrochanteric Femoral Fracture
- Jong Min Lim, Jeung Il Kim, Jong Seok Oh, Kuen Tak Suh, Jae Min Ahn, Dong Joon Kang
- J Korean Fract Soc 2010;23(4):360-366. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.360
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the radiologic, clinical results between who had intertrochanteric fracture, treated with Compression Hip Screw (CHS) and Proximal Femoral Nail Antirotation (PFNA).
MATERIALS AND METHODS
We retrospectively reviewed each 36 and 48 patients of intertrochanteric fracture which were treated with CHS or PFNA by one surgeon from January 2005 to June 2009. We evaluated mean operation time, amount of bleeding, radiologic results, and the clinical outcomes with the mobility score of Parker and Palmer, social function scoring system.
RESULTS
The mean operation time, amount of bleeding were less in the PFNA group, there were 116.7 min, 486.1 ml for the CHS group versus 87.7 min, 289.6 ml for the PFNA group. The radiologic results were not significantly different. Decrease of mobility score of Parker and Palmer, social function score were similar. Proximal migration of leg screw and perforation of femoral head was 2 case and deep infection was 1 cases in CHS group.
CONCLUSION
There were no significant differences that are clinical and radiological results in treatment of intertrochanteric fracture using the CHS and PFNA. But PFNA is less invasive device than CHS, therefore it may be useful device in elderly patients. -
Citations
Citations to this article as recorded by- Chronic kidney disease patients with intertrochanteric fracture have a high mortality rate
Tae Woo Kim, Sang-Min Lee, Nam Hoon Moon, Won Chul Shin
Injury.2021; 52(8): 2350. CrossRef - Comparison between the Results of Internal Fixation Using Proximal Femur Nail Anti-rotation and Bipolar Hemiarthroplasty in Treatment of Unstable Intertrochanteric Fractures of Elderly Patients
Sung-Hwan Kim, Soo-Won Lee, Gyu-Min Kong, Mid-Um JeaGal
Hip & Pelvis.2012; 24(1): 45. CrossRef - Treatment of Intertrochanteric Fractures Using Targon Proximal Femoral Nails
Il Ho Park, Jong Kyoung Won, Kye Young Han
Hip & Pelvis.2012; 24(2): 117. CrossRef - A Comparison of Intramedullary and Extramedullary Fixations for the Treatment of Reverse Oblique or Transverse Intertrochanteric Femoral Fractures
Yerl-Bo Sung, Jung-Yun Choi, Eui-Yub Jung
Hip & Pelvis.2012; 24(2): 109. CrossRef
- Chronic kidney disease patients with intertrochanteric fracture have a high mortality rate
- 2,158 View
- 5 Download
- 4 Crossref

- Analysis of the Causes for Failed Compression Hip Screws in Femoral Intertrochanteric Fracture and Hip Reconstruction Operation
- Ui Seoung Yoon, Jin Soo Kim, Jae Sung Seo, Jong Pil Yoon, Seung Yub Baek
- J Korean Fract Soc 2010;23(3):270-275. Published online July 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.3.270
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the causes of fixation failure of compression hip screw and evaluate outcomes of hip arthroplasty for reconstruction.
MATERIALS AND METHODS
We reviewed 108 femoral intertrochanteric fractures that underwent compression hip screw between January 1997 and December 2007. Failure group (group I) contained 28 cases who had hip arthroplasty for failed compression hip screw and the control group (group II) contained 80 cases who had successive compression hip screw. We analyzed the causes of failure of compression hip screw and evaluated the results of hip arthroplasty for reconstruction.
RESULTS
In group I, 21 cases (75%) were unstable fractures. Group II, 14 cases (17%) were unstable fractures. Tip-apex distance was 26.5 (18~35) mm in group I and 18.6 (8~22) mm in group II. Lateral wall fracture of greater trochanteric area was combined in 24 cases (85.7%) in group I and 9 cases (11.3%) in group II. Harris Hip Score improved from 33.5 (22~43) points to 84.2 (75~93) points after salvage hip arthroplasty.
CONCLUSION
We considered the causes of failed compression hip screw to be fracture instability, increased tip-apex distance and presence of lateral wall fracture of greater trochanter. Hip arthroplasty was found to be a useful method for failed compression hip screw.
- 486 View
- 1 Download

- Proximal Femoral Nail Antirotation versus Compression Hip Screw with Trochanter Stabilizing Plate for Unstable Intertrochanteric Hip Fractures
- Jae Young Rho, Sang Bum Kim, Youn Moo Heo, Seong Jin Cho, Dong Sik Chae, Woo Suk Lee
- J Korean Fract Soc 2010;23(2):161-166. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.161
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze and compare the clinical and radiologic results of treatments in unstable intertrochanteric fractures of the femur with proximal femoral nail antirotation (PFNA) and compression hip screw with trochanter stabilizing plate (CHS with TSP).
MATERIALS AND METHODS
We retrospectively reviewed the results of 66 cases of unstable intertrochanteric fractures of the femur treated with PFNA (Group I) and CHS with TSP (Group II) which could be followed up for minimum a year. We evaluated several comparative factors such as operation time, blood loss, time to bone union, changes in neck-shaft angle, sliding of screw (or blade), complications, postoperative pain, social-function score of Jensen, and mobility score of Parker and Palmer.
RESULTS
Group I showed shorter operation time and less blood loss with significance than group II (p<0.05), but there were no differences between the groups in the mean time to bone union, changes in neck-shaft angle, sliding of screw (or blade), complications, postoperative pain, and social-function score of Jensen (p>0.05). Two cases of cutting out of the blade through the femoral head were found in group I. One case of cutting out of the screw, one case of the breakage of the plate, and loosening of the plate were found in group II as complications.
CONCLUSION
We think that there were no significant differences between PFNA and CHS with TSP in view point of radiologic and clinical outcomes in unstable intertrochanteric fractures of the femur, but PFNA is less invasive device than CHS with TSP, therefore it may be useful device in elderly patients. -
Citations
Citations to this article as recorded by- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
Byung-Woo Min, Kyung-Jae Lee, Gyo-Wook Kim, Ki-Cheor Bae, Si-Wook Lee, Du-Han Kim
Journal of the Korean Fracture Society.2014; 27(2): 120. CrossRef - Effectiveness of the Valgus Reduction Technique in Treatment of Intertrochanteric Fractures Using Proximal Femoral Nail Antirotation
Ji-Kang Park, Hyun-Chul Shon, Yong-Min Kim, Eui-Sung Choi, Dong-Soo Kim, Kyoung-Jin Park, Byung-Ki Cho, Jung-Kwon Cha, Sang-Woo Kang
Journal of the Korean Orthopaedic Association.2013; 48(6): 441. CrossRef - A Comparison of Intramedullary and Extramedullary Fixations for the Treatment of Reverse Oblique or Transverse Intertrochanteric Femoral Fractures
Yerl-Bo Sung, Jung-Yun Choi, Eui-Yub Jung
Hip & Pelvis.2012; 24(2): 109. CrossRef
- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
- 912 View
- 1 Download
- 3 Crossref

- Treatment of Unstable Intertrochanteric Fracture in Elderly Patients : Comparison between the Results of Internal Fixation Using Compression Hip Screw and Cemented Bipolar Hemiarthroplasty
- Myung Sik Park, Woo Chul Jung, Hyuk Park, Byung Yun Hwang, Young Jin Lim, Myung Guk Jung, Hong Man Cho
- J Korean Fract Soc 2009;22(3):138-144. Published online July 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.3.138
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To perform comparative analysis between the results of internal fixation using compression hip screw and cemented bipolar hemiarthroplasty in unstable intertrochanteric fracture in elderly patients.
MATERIALS AND METHODS
From January 2001 to October 2006, we reviewd 73 patients, who were treated surgically for unstable intertrochanteric fractures, with a minimum of 2 years follow up. The patient's age was older than 60 year old. The patients were divided into two groups and evaluated, retrospectively. One group was treated with cemented bipolar hemiarthroplasty (Group A, 34 cases), and the other group was treated with compression hip screw (Group B, 39 cases). We evaluated the amount of intraoperative bleeding, operative time, clinical results and complications between the two groups.
RESULTS
The amount of intraoperative bleeding and operative time were no statistically significant between the two groups. Group A showed a better result than Group B for clinical outcome using Johnson Daily Activity of Life. Complications in the group A were comprised of dislocation (1 case), nonunion of greater trochanter (1 case), infection (1 case) and loosening (1 case), and those in the group B were comprised of loss of fixation (8 cases) and infection (1 case).
CONCLUSION
We found that short-term outcomes of cemented bipolar hemiarthroplasty for unstable intertrochanteric fractures were satisfactory. However, a longer-follow up period is necessary to clarify the efficacy of cemented bipolar hemiarthroplasty. -
Citations
Citations to this article as recorded by- Early Rehabilitation in Elderly after Arthroplasty versus Internal Fixation for Unstable Intertrochanteric Fractures of Femur: Systematic Review and Meta-Analysis
Jun-Il Yoo, Yong-Chan Ha, Jae-young Lim, Hyun Kang, Byung-Ho Yoon, Hyunho Kim
Journal of Korean Medical Science.2017; 32(5): 858. CrossRef - The Comparison of Compression Hip Screw and Bipolar Hemiarthroplasty for the Treatment of AO Type A2 Intertrochanteric Fractures
Yee-Suk Kim, Jae-Seung Hur, Kyu-Tae Hwang, Il-Yong Choi, Young-Ho Kim
Hip & Pelvis.2014; 26(2): 99. CrossRef
- Early Rehabilitation in Elderly after Arthroplasty versus Internal Fixation for Unstable Intertrochanteric Fractures of Femur: Systematic Review and Meta-Analysis
- 737 View
- 1 Download
- 2 Crossref

- The Comparison between ITST(TM) (Intertrochanteric/Subtrochanteric) & DHS (Dynamic Hip Screw) in Unstable Femur Intertrochanteric Fracture
- Ho Seung Jeon, Byung Mun Park, Kyung Sub Song, Hyung Gyu Kim, Jong Ju Yun
- J Korean Fract Soc 2009;22(3):131-137. Published online July 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.3.131
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate between DHS and ITST nail (2nd generation) on the treatment of unstable femur intertrochanteric fracture in patients over 70 years old.
MATERIALS AND METHODS
61 cases of unstable intertrochanteric fracture (grouped 37 patients with DHS and 24 patients with ITST) who were taken the operation from Mar. 2003 to Sep. 2007 were analysed regarding to union time, sliding length of lag screws, operation time, blood loss, postoperative complications and functional recovery score by Skovron.
RESULTS
The mean union time was 14.7 weeks in study group (ITST). The mean union time was 16.2 weeks in control group (DHS). The lag screw slidings were 7.2 mm in study group and 8.7 mm in control group. The operation times were 57.9 min in study group and 76.9 min in control group. The amount of blood loss were 67.7 ml in study group and 227.4 ml in control group. The complications were 4 cases in study group and 4 cases in control group. The Skovron recovery scores were 76.5% in study group and 73.7% in control group.
CONCLUSION
From a practical point of short operation time, less amount of bleeding and less complication, author think that the ITST nail is useful implant for treatment of unstable femur intertrochanteric fracture in patient of old age. -
Citations
Citations to this article as recorded by- Unstable Intertrochanteric Fracture Treated with ITST: A Comparative Study between Groups with and without Comminution of Greater Trochanter
Kyung-Sub Song, Sang-Ho Lee, Seong-Hun Jeong, Su-Keon Lee, Sung-Ha Hong
Journal of the Korean Fracture Society.2014; 27(1): 36. CrossRef - Treatment of the Intertrochanteric Femoral Fracture with Proximal Femoral Nail: Nailing Using the Provisional K-wire Fixation
Gu-Hee Jung
Journal of the Korean Fracture Society.2011; 24(3): 223. CrossRef
- Unstable Intertrochanteric Fracture Treated with ITST: A Comparative Study between Groups with and without Comminution of Greater Trochanter
- 741 View
- 3 Download
- 2 Crossref

- Treatment of Failed Intertrochanteric Fractures to Maintain the Reduction in Elderly Patients
- Soon Yong Kwon, Hyun Woo Park, Sang Uk Lee, Soo Hwan Kang, Jae Young Kwon, Jung Hoon Do, Seung Koo Rhee
- J Korean Fract Soc 2008;21(4):267-273. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.267
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study was to evaluate and report the new method with a cement augmented screw fixation again to treat the failed intertrochanteric fracture in elderly which were treated with ordinary compression hip screw initially.
MATERIALS AND METHODS
From Mar. 1988 to May 2007, 10 patients (mean age 69 years) with the failed intertrochanteric fracture which were treated with initial hip screw, were treated with a cement augmented compression hip screw again. The mean follow-up after surgery was over 18 months. The cause of failure, the period upto the reoperation, the neck-shaft angle after the reoperation, the position of lag screw in the femoral head, and the degree of union at last follow-up were analyzed. The change in the functional hip capacity were evaluated by the classification of Clawson.
RESULTS
Causes of failure were superior cutting-out in 6 cases, cortical anchorage failure in 3, and nonunion in one case. The period upto the reoperation was average 7.8 months. Valgus reduction of average 5.7degrees was achieved, and the positions of lag screw were postero-inferior in 6 cases, center in 3, infero-center in one case. We obtained complete union in 9 cases. The functional outcome showed moderate in 6 cases, good in 3 and poor degree in one case.
CONCLUSION
Cement augmented compression hip screw treatment will possibly reduce cutting-out of screw and bring more stability in fixation for intertrochanteric fractures in old osteoporotic patients, as well, even in failed cases treated with initial compression hip screw, but proper selection of patients is important. -
Citations
Citations to this article as recorded by- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
So Young Kim
Journal of the Korean Fracture Society.2019; 32(2): 89. CrossRef
- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
- 712 View
- 1 Download
- 1 Crossref

- Treatment of Stable Intertrochanteric Fractures Using a Short Side Plate Dynamic Hip Screw
- Chong Kwan Kim, Jin Woo Jin, Sung Won Jung, Wan Sub Kwak, Jae Il Jo, Woo Sik Kim
- J Korean Fract Soc 2006;19(3):309-313. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.309
-
 Abstract
Abstract
- PURPOSE
To evaluate the usefulness of a 2 holes side plate dynamic hip screw for the treatment of stable intertrochanteric fracture of the femur.
MATERIALS AND METHODS
Between January 2000 and September 2004, 46 patients with intertrochanteric fracture of the femur were treated with 2 hole side plate dynamic hip screw (Group 1, 25 cases) or 4 hole side plate dynamic hip screw (Group 2, 21 cases). The mean age of the patient was 70 years, with a mean follow-up duration of 13 months. The time for operation, surgical incision length, blood loss, time for union, the sliding distance, change in the femoral neck-shaft angle and patient's walking ability were evaluated.
RESULTS
The mean operation time and mean incision length were shortened, and mean blood loss was decreased in Group 1 (p<0.01). There was no statistical difference in the union time, the mean change in the femoral neck-shaft angle and the mean sliding distance of the lag screw at the last follow-up. The mean mobility score of the Parker and Palmer was 8.0 points before the fracture and 7.2 points at the last follow-up.
CONCLUSION
Two-hole side plate dynamic hip screw is a useful device, in terms of the operation time, morbidity of operation site, satisfactory union rate and functional recovery of the patient in treatment of elderly patients with stable intertrochanteric fractures of the femur.
- 438 View
- 0 Download

- Treatment of Comminuted Subtrochanteric Fractures of the Femur by High-Energy Trauma
- Taek Soo Jeon, Woo Sik Kim, Sang Bume Kim, Cheol Mog Hwang, Kyu Tae Kim, Sun Hong Kim
- J Korean Fract Soc 2006;19(2):135-140. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.135
-
 Abstract
Abstract
- PURPOSE
The purpose is to evaluate the effectiveness of open reduction and internal fixation in comminuted subtrochanteric fractures caused by high energy trauma at a non-osteoporotic young age.
MATERIALS AND METHODS
Of all cases of subtrochanteric fractures caused by high energy trauma under 60 years old from February 2000 to February 2004, we analyzed 16 patients who had severe comminuted fractures (Seinsheimer classification type IV, V). The mean age is 43.5 (31~54) years old. Mean follow-up period was 22 (14~38) months. We tried to reduce anatomically as much as possible and fixed firmly using a compression hip screw in all cases. Additional procedures such as interfragmentary screw fixation, cerclage wiring or lateral stabilization plating were performed in 13 cases. Bone grafting was performed in 8 cases. We evaluated bony union rate, time to union, status of reduction, varus deformity and rate of implant failure using a simple X-ray. We also analyzed the clinical result using the Harris hip score including range of motion, pain and limping gait, so on.
RESULTS
In all 16 cases, bony union was achieved and the mean time to union was 24 (20~32) weeks. There was no intra-operative complication. Postoperative complications such as loss of reduction, varus deformity, implant failure or infection did not occur. Clinically, the Harris hip score was 98.9 (97~100) points.
CONCLUSION
Optimal open reduction and firm internal fixation with or without additional fixation was thought to be a recommendable method of treatment for comminuted subtrochanteric fractures of the femur caused by high energy trauma at a young age. -
Citations
Citations to this article as recorded by- Treatment of Subtrochanteric Femur Fractures Using Intramedullary Devices
Chung Soo Hwang, Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Chong Suk Park, Sang Ho Lee
Journal of the Korean Fracture Society.2008; 21(1): 13. CrossRef
- Treatment of Subtrochanteric Femur Fractures Using Intramedullary Devices
- 604 View
- 0 Download
- 1 Crossref

- Treatment of Subtrochanteric Fractures with Compression Hip Screw
- Kee Haeng Lee, Hyoung Min Kim, Youn Soo Kim, Chang Hoon Jeong, Il Jung Park, Ill Seok Park, Chan Woong Moon
- J Korean Fract Soc 2006;19(1):1-5. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.1
-
 Abstract
Abstract
- PURPOSE
To evaluate the effectiveness of the compression hip screw, we reviewed the clinical results of cases of femoral subtrochanteric fracture which were treated with compression hip screw.
MATERIALS AND METHODS
From May 1997 to June 2004, 20 cases of femoral subtrochanteric fracture, which were treated with compression hip screw and followed up more than 12 months, were reviewed. By the Seinsheimer's classification, there were 1 case of type IIa, 4 cases of type IIb, 2 cases of type IIIa and IIIb, 4 cases of type IV and 7 cases of V. We analyzed the treatment results by bony union time, range of motion, ambulation status and complications.
RESULTS
All 20 cases were gained bony union without serious complications and secondary operation. The average bony union time was 19.8 weeks. 17 of 20 cases were recovered pre-injury ambulatory status level.
CONCLUSION
The compression hip screw may be effective in treatment of the femoral subtrochanteric fracture with very narrow intramedullary canal, proximal femoral deformity, comminuted fracture with large butterfly fragment, long spiral fracture with medial cortical comminution and combined intertrochanteric fracture. -
Citations
Citations to this article as recorded by- The stabilising effect by a novel cable cerclage configuration in long cephalomedullary nailing of subtrochanteric fractures with a posteromedial wedge
Pavel Mukherjee, Jan Egil Brattgjerd, Sanyalak Niratisairak, Jan Rune Nilssen, Knut Strømsøe, Harald Steen
Clinical Biomechanics.2019; 68: 1. CrossRef - Factors Affecting Time to Bony Union of Femoral Subtrochanteric Fractures Treated with Intramedullary Devices
Jung-Yoon Choi, Yerl-Bo Sung, Jin-Hee Yoo, Sung-Jae Chung
Hip & Pelvis.2014; 26(2): 107. CrossRef
- The stabilising effect by a novel cable cerclage configuration in long cephalomedullary nailing of subtrochanteric fractures with a posteromedial wedge
- 605 View
- 0 Download
- 2 Crossref

- The Treatment of Unstable Intertrochanter Fracutures of Femur: Comparison between Proximal Femoral Nail and Dynamic Hip Screw
- Kyun Chul Kim, Hun Kyu Shin, Kyung Mo Son, Chun Seok Ko
- J Korean Fract Soc 2005;18(4):369-374. Published online October 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.4.369
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the results between PFN (Proximal Femoral Nail) and DHS (Dynamic Hip Screw) on the operative treatment of unstable intertrochanteric fractures retrospectively.
MATERIALS AND METHODS
35 cases of unstable intertrochanteric fractures (grouped 24 patients with DHS and 11 patients with PFN) who were taken the operations from Jan. 2001 to Mar. 2002 were analysed regarding to union state, union time, operation time, sliding length of lag screws, blood loss, postoperative complications and functional recovery scores by Sk?vron with ANOVA and multivariate linear regression.
RESULTS
The means of union time were 17.9 weeks (DHS) and 17.0 weeks (PFN), sliding length of lag screws were 3.9 mm (DHS) and 2.1 mm (PFN), perioperative blood losses were 743 cc (DHS) and 736 cc (PFN), operation time were 93.4 minutes (DHS) and 102 minutes (PFN), and the functional recovery scores by Sk?vron were 71.8% (DHS) and 76.8% (PFN), respectively. The results of our study indicate that there were not statistically significant differences between PFN and DHS groups in treatment of unstable intertrochanteric fractures (p>0.05). But, there was less sliding of lag screws in PFN group in statistical significance (p<0.05).
CONCLUSION
Authors think that PFN is one of the useful implants in treating unstable intertrochanteric fractures of the femur in regarding to sliding. -
Citations
Citations to this article as recorded by- Bipolar Hemiarthroplasty in Unstable Intertrochanteric Fractures with an Effective Wiring Technique
Jae-Hwi Nho, Gi-Won Seo, Tae Wook Kang, Byung-Woong Jang, Jong-Seok Park, You-Sung Suh
Hip & Pelvis.2023; 35(2): 99. CrossRef - Comparison of the Gamma Nail and the Dynamic Hip Screw for Peritrochanteric Fracture
Seok Hyun Kweon
Hip & Pelvis.2011; 23(2): 124. CrossRef - The Efficiency of Additional Fixation of the Alternative Bone Substitute in Unstable Intertrochanteric Fractures of Femur Treated with Gamma Nail
Jong-Oh Kim, Young-One Ko, Mi-Hyun Song
Journal of the Korean Fracture Society.2011; 24(1): 1. CrossRef
- Bipolar Hemiarthroplasty in Unstable Intertrochanteric Fractures with an Effective Wiring Technique
- 681 View
- 3 Download
- 3 Crossref

- The Compression Hip Screw with Trochanter Stabilizing Plate for Internal Fixation of Unstable Intertrochanteric Fractures
- Jin Ho Cho
- J Korean Fract Soc 2005;18(3):221-226. Published online July 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.3.221
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate trochanter stabilizing plate and compression hip screw can prevent excessive impaction and cutting-out in unstable intertrochanteric fractures.
MATERIALS AND METHODS
One hundred twenty-one patients with intertrochanteric fractures were treated between December 1999 and March 2002. Of the patients, twenty-four patients were treated with an additional TSP on the CHS. Nineteen patients were followed for more than six months. The fractures were classified according to the AO classification. Impactions of compression lag screw were measured immediate postoperatively and postoperatively three months later on simple radiographs. Functional results were followed Salvati-Wilson assessment score at postoperative six months later.
RESULTS
The group consisted of seven men and twelve women, and the mean age was 73 years. Two were classified as A2.2, six A2.3, one A3.2, and ten A3.3 fractures. Mean impaction was 5.4 mm (range 1.8 to 11.4 mm). Functional results were excellent in 32% and good in 53%. Eighteen patients had healed after operation. One complication required a bipolar hemiarthroplasty due to cutting-out of lag screw.
CONCLUSION
In three-part and four-part intertrochanteric fractures with lateral cortex breakage or vertical fracture in greater trochanter, the addition of TSP to CHS can prevent abductor muscle weakness due to fracture impaction, limb shortening and additional lateral cortical fracture. It also helps early weight bearing and bone healing.
- 414 View
- 0 Download

Note
- New Wiring Method for Lesser Trochanter Fixation in Unstable Intertrochanteric Fractures: Technical Note
- Joong Myung Lee, Jeong Hee Lee, Churl Woo Lee, Hyun Min Kim
- J Korean Fract Soc 2005;18(2):209-212. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.209
-
 Abstract
Abstract
 PDF
PDF - In unstable femoral trochanteric fracture, we usually used transversing K-wires through the lesser trochanter to achieve an anatomical reduction, and using sliding hip screws. However, in patients with comminuted lesser trochanter or osteoporosis, an intrusion of the wire into the lesser trochanter and/or iatrogenic intertrochanteric fractures were often resulted. Those who were not familiar with a technique of puncturing two holes through the lesser trochanter might have had to face some difficulties. In order to overcome aforementioned drawbacks, the authors had quite satisfactory results by employing the method of passing each of two wires above and below the iliopsoas muscle, and they were twisted posteriorly and then anteriorly; and finally they were pulled together posteriorly. Through this technique, both firm fixation of the lesser trochanter and more stable bony union were obtained.
-
Citations
Citations to this article as recorded by- The lesser trochanter “Sling fixation technique” in proximal intramedullary nailing of unstable intertrochanteric fractures: A polymer-based cerclage wiring
Marco Villano, Matteo Innocenti, Roberto Civinini, Christian Carulli, Alessandro Civinini, Zyad Ayman Taha, Andrea Cozzi Lepri
Journal of Orthopaedics.2022; 34: 94. CrossRef - Unstable Intertrochanteric Fracture: Do We Know Everything? A Review
Balaji Zacharia, Harshitha Hayavadana Udupa
SN Comprehensive Clinical Medicine.2022;[Epub] CrossRef - When to Reduce and Fix Displaced Lesser Trochanter in Treatment of Trochanteric Fracture: A Systematic Review
Ao-Lei Yang, Wei Mao, Jun-Guo Wu, Yi-Qun He, Hao-Fei Ni, Hai-Long Li, You-Hai Dong
Frontiers in Surgery.2022;[Epub] CrossRef - Medial wall fragment involving large posterior cortex in pertrochanteric femur fractures: a notable preoperative risk factor for implant failure
Pengfei Li, Yang Lv, Fang Zhou, Yun Tian, Hongquan Ji, Zhishan Zhang, Yan Guo, Zhongwei Yang, Guojin Hou
Injury.2020; 51(3): 683. CrossRef - In response
David J. Ciufo, John P. Ketz
Journal of Orthopaedic Trauma.2018; 32(9): e382. CrossRef - Three-Dimensional Computed Tomography Reduced Fixation Failure of Intramedullary Nailing for Unstable Type of Intertrochanteric Fracture
Wei-Yu Li, Kai-Cheng Lin
Journal of Orthopaedic Trauma.2018; 32(9): e381. CrossRef - Wiring Techniques for the Fixation of Trochanteric Fragments during Bipolar Hemiarthroplasty for Femoral Intertrochanteric Fracture: Clinical Study and Technical Note
Joong-Myung Lee, Yongsuk Cho, Junhyun Kim, Dong-Won Kim
Hip & Pelvis.2017; 29(1): 44. CrossRef - Wiring technique for lesser trochanter fixation in proximal IM nailing of unstable intertrochanteric fractures: A modified candy-package wiring technique
Gyeong Min Kim, Kwang Woo Nam, Kyu-Bum Seo, Chaemoon Lim, Jiyun Kim, Yong-Geun Park
Injury.2017; 48(2): 406. CrossRef - Bipolar Hemiarthroplasty with Cementless Femoral Stem for Unstable Intertrochanteric Fractures
Joong-Myung Lee, Hee-Tae Nam, Sang-Hun Lee
Journal of the Korean Orthopaedic Association.2012; 47(2): 79. CrossRef
- The lesser trochanter “Sling fixation technique” in proximal intramedullary nailing of unstable intertrochanteric fractures: A polymer-based cerclage wiring
- 699 View
- 15 Download
- 9 Crossref

Original Articles
- Radiologic Result of Treatment of Intertrochanteric Fracture Using Compression Hip Screw: Involvement of Lateral Cortex
- Suk Ha Lee, Sung Tae Lee, Kwang Jun Oh, Yong Bae Kim, Woo Seung Lee, Ji Sung Jun, In Rok Yoo, Jung Sup Keum
- J Korean Fract Soc 2005;18(2):115-119. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.115
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the meaning of the unstable intertrochanteric fracture of femur with involvement of lateral cortex by analysing the radiologic result of the surgical treatment using a compression hip screw.
MATERIALS AND METHODS
Classifing patients (who has taken the surgical treatment for intertrochanteric fracture of femur using compression hip screw from January 1999 to June 2002) in our hospital with 24 patients who had not much difference statistically in the compression screw located within the femur, Tip-Apex distance (TAD) the Singh Numerical Value of osteoporosis. The results were divided into two groups, group A (without fracture extends through lateral cortex of femur: 16 cases) and B (fracture extends through lateral cortex of femur: 8 cases), when analyzing it. And then analyzed the final examination in the evaluation of electrical potential level by radiology, change of the inside and outside of neck-shaft angle, descent level of the screw and the change of the neck-shaft angle.
RESULTS
In the latest follow up, the sliding amount of the screw in group B, the average was 14.9+/-9.3 mm, and 6.7+/-3.6 mm in group A. There was no difference statistically (p value>0.05). In the varus change in group B, the average was 8.00+/-8.12degrees and in group A it ws 2.75+/-2.63degrees There was statistical difference(p value<0.05). In displacement after operation, it was 7.60+/-2.61 mm in group B and 0.5+/-1.80 mm in group A. There was statistical difference (p value<0.05).
CONCLUSION
The intertrochanteric fracture with involvement of lateral cortex of femur have to be considered as unstable fracture having tendency of displacement. -
Citations
Citations to this article as recorded by- Analysis of the Causes for Failed Compression Hip Screws in Femoral Intertrochanteric Fracture and Hip Reconstruction Operation
Ui Seoung Yoon, Jin Soo Kim, Jae Sung Seo, Jong Pil Yoon, Seung Yub Baek
Journal of the Korean Fracture Society.2010; 23(3): 270. CrossRef
- Analysis of the Causes for Failed Compression Hip Screws in Femoral Intertrochanteric Fracture and Hip Reconstruction Operation
- 550 View
- 0 Download
- 1 Crossref

- Sliding after Internal Fixation of Stable Intertrochanteric Fracture of the Femur
- Woo Suk Lee, Whan Young Chung, Woo Sik Kim, Yong Chan Kim, Taek Soo Jeon, Sung Kwun Jo, In Tak Bae, Young Su Lim
- J Korean Fract Soc 2005;18(2):110-114. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.110
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the risk factors of sliding after internal fixation with sliding compression hip screw in stable intertrochanteric fracture of the femur.
MATERIALS AND METHODS
From March 2000 to April 2003, 61 stable intertrochanteric fractures (Kyle-Gustilo type II) were treated operatively with sliding compression hip screws. The patients were 40 females and 21 males with an average age of 74 (range, 54~99). We measured vertical and horizontal shortening in regard to age, sex, bone mineral density, neck-shaft angle, cancellous bone defect, and the existence of lessor trochanter fracture on postoperative 6 months.
RESULTS
The average vertical shortening was 4.1 mm (0~22 mm) and the average horizontal shortening was 7.3 mm (0~30 mm). Age, sex, bone density and neck-shaft angle were not significantly related with vertical and horizontal shortening (p>0.05). Vertical shortening was significantly greater in the group with cancellous bone defect and in the group without lesser trochanter fracture (p<0.05).
CONCLUSION
Proper management for fracture site and fixation was needed to make it stable because the stable intertrochanteric fracture with cancellous bone defect and intact lesser trochanter could be induced into unexpected sliding. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 575 View
- 1 Download
- 1 Crossref

- Fixation Failure of Unstable Intertrochanteric Fracture of the Femur Using Compression Hip Screw
- Sang Won Park, Soon Hyuck Lee, Jong Ryoon Baek, Sung Jun Park, Jong Won Chung
- J Korean Fract Soc 2005;18(1):1-5. Published online January 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the factors which influence on the fixation failure after the compression hip screw fixation for unstable intertrochanteric fractures.
MATERIALS AND METHODS
Eighty-two patients of unstable intertrochanteric fracture of A2 and A3 type who had underwent operation with compression hip screw were evaluated at least 1 year follow-up in regard to the age, degree of osteoporosis, fracture type, diastasis of fragment, sliding of lag screw, position of lag screw and status of reduction.
RESULTS
73 patients out of 82 patients had the union and 9 patients showed fixation failure. The results of fixation failure were 6 cases of migration of lag screw and 3 cases of cut-out of lag screw. There were statistically significant correlations between fixation failure and A2.3 and A3 type. The fixation failure group showed increased medial migration of medial cortex of proximal and distal fragment, which is significantly correlated with fixation failure. There were little statistical significant correlations between age, degree of osteoporosis, status of reduction, position of lag screw, sliding of lag screw and fixation failure.
CONCLUSION
Another alternative fixation method and technique have to be considered for unstable A2-3 or A3 type because compression hip screw fixation only is very insufficient with high failure rate.
- 396 View
- 1 Download

- Correlation between Anterior and Posterior Obliquity of the Sliding Lag Screw and Stability in Unstable Intertrochanteric Fractures
- Kyu Hyun Yang, Je Hyun Yoo, Dong Joo Rhee, Jung Hoon Won, Dae Ya Kim, Dong Sik Sim
- J Korean Fract Soc 2004;17(4):308-313. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.308
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the characteristics of the sliding pattern of the proximal fragment (head and neck) in unstable intertrochanteric fractures, which were fixed with a dynamic hip screw (DHS) with anterior to posterior or posterior to anterior insertion angle in the axial view.
MATERIALS AND METHODS
AO type A2.1 intertrochanteric fracture was reproduced in 10 proximal femur model (Synbone, Malans, Switzerland). Five fractured models were reduced and fixed using DHS with anterior to posterior insertion angle (group 1) and five models were fixed with posterior to anterior angle (group 2). Load of 500 N (30 cycles) was applied to the fracture fragment-plate complex using Instron 6022. Data on the distance of sliding and the angle of rotation of the proximal fragment were collected and analyzed.
RESULTS
No significant difference was noted statistically in the distance of sliding between the two groups (p=0.92). However, the mean angle of rotation was 13.4degrees and 8.0degrees in group 1 and 2, respectively and the difference was statistically significant (p=0.012). Anterior cortical fracture of distal fragment was noted in 3 cases of group 1. There was no fracture of the anterior cortex in group 2.
CONCLUSION
In unstable intertrochanteric fracture, the insertion angle of the lag screw in axial view does seem to play a role in the fate of bone-plate complex. Early eccentric contact of both fragments caused rotation of the proximal fragment in all cases and anterior cortical fracture of the distal fragment in 3 cases of group 1.
- 360 View
- 0 Download

- Comparison of Clinical Results between Bipolar Hemiarthroplasty and Compression Hip Screw on Unstable Intertrochanteric Fractures of the Femur in Elderly Patients
- Eui seoung Yoon, Hak Jin Min, Jae Seong Suh, Yoon Jong Kim, Hee Seon Kim, Yong Jun Lee, Jeong Min Heo
- J Korean Fract Soc 2004;17(3):214-220. Published online July 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.3.214
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate postoperative incidence of complications and functional results between two groups, primary bipolar hemiarthroplasty and internal fixation with compression hip screw on unstable intertrochanteric fractures of the femur with severe osteoporosis in elderly patients.
MATERIALS AND METHODS
78 cases treated under unstable intertrochanteric fractures of the femur with severe osteoporotic elderly patients from March 1997 to August 2001 who have been followed up for more than a year were evaluated retrospectively between the group of bipolar hemiarthroplasty, 38 cases out of 60 cases and group of compression hip screw, 40 cases out of 59 cases. The incidence of complications and functional ability according to Merle d'Aubigne scale and the mortality rate were compared using student t-test.
RESULTS
The means of Merle d'Aubigne scale for the hemiarthroplasty group and the compression hip screw group were at the last follow up, 15.0 and 13.6 respectively. The differences were statistically significant (p=0.04). Bipolar group revealed significant differences in general (18%) and mechanical complications (5%) between two groups (p<0.05). The mortality rates were 28% and 22% respectively and there were no significant differences statistically (p>0.05).
CONCLUSION
We consider that primary bipolar hemiarthroplasty would be better method in the treatment of the unstable femoral intertrochanteric fracture with severe osteoporosis but we need much longer follow up. -
Citations
Citations to this article as recorded by- Outcomes of Cephalomedullary Nailing in Basicervical Fracture
Seok Hyun Kweon, Sung Hyun Lee, Seng Hwan Kook, Young Chae Choi
Hip & Pelvis.2017; 29(4): 270. CrossRef - Bipolar Hemiarthroplasty Using the Greater Trochanter Reattachment Device (GTRD) for Comminuted Intertrochanteric Femur Fracture in Elderly Patients
Jin-Wan Kim, Young-Chul Ko, Chul-Young Jung, Il-Soo Eun, Hyeon-Soo Choi, Ok-Gul Kim, Young-June Kim
Journal of the Korean Fracture Society.2009; 22(4): 232. CrossRef - Bipolar Hemiarthroplasty for Femoral Basicervical Fractures in the Elderly
Duk-Hwan Kho, Ki-Hwan Kim, Hyeung-Jun Kim, Dong-Heon Kim
Journal of the Korean Fracture Society.2009; 22(4): 239. CrossRef - Bipolar Hemiarthroplasty Using Calcar Replacement Stem for Hip Fractures in the Elderly
Duk-Hwan Kho, Ki-Hwan Kim, Hyeung-June Kim, Dong-Heon Kim
Journal of the Korean Fracture Society.2008; 21(3): 232. CrossRef - Trochanteric Management for Unstable Intertrochanteric Femoral Fracture in the Elderly Patients
Duk-Hwan Kho, Ju-Yong Shin, Ki-Hwan Kim, Jun-Hyuck Lee, Dong-Heon Kim
Journal of the Korean Fracture Society.2007; 20(2): 129. CrossRef
- Outcomes of Cephalomedullary Nailing in Basicervical Fracture
- 616 View
- 0 Download
- 5 Crossref

- Fixation Failure of Compression Hip Screw in Unstable Intertrochanteric Fracture of Femur
- Deuk Soo Hwang, Sang Goo Kwak, Young Mo Kim, Dae Chul Nam, Ui Pyo Hong
- J Korean Soc Fract 2003;16(4):600-604. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.600
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the factor of fixation failure in association of the early controlled weight bearing exercise after using a compression hip screw (CHS) for unstable intertrochanteric fracture of femur in old ages.
MATERIALS AND METHODS
Between May 1998 and February 2002, 8 cases of fixation failure of CHS among the 80 patients were evaluated. We compared gender, age, fracture type with a matched group that fixation failure was not noted. During operation, we performed valgus nailing of compress lag screw and compressed fracture gap with a bolt as soon as possible. The patients were encouraged partial weight bearing 4~5 days after operation and compaired immediate postoperative and postoperative 2 weeks x-ray films about degree of slippage or varus angulation of femur.
RESULTS
In 5 cases, cut-out of the lag screw were found. In 3 cases, plate fracture and fixation failure were found. Relation between timing of partial weight bearing and fixation failure was not significant (p=0.146). But in 5 cases of failure, they continued weight bearing in spite of excessive slippage of the lag screw.
CONCLUSION
Early controlled partial weight bearing exercise after operation of intertrochanteric fracture of the femur were reported good for functional recovery in old ages. But, excessive slippage of the lag screw or varus angulation of proximal femur were found on follow up period, patient teaching and control of ambulation is strongly recommended. -
Citations
Citations to this article as recorded by- Treatment of Failed Intertrochanteric Fractures to Maintain the Reduction in Elderly Patients
Soon-Yong Kwon, Hyun-Woo Park, Sang-Uk Lee, Soo-Hwan Kang, Jae-Young Kwon, Jung-Hoon Do, Seung-Koo Rhee
Journal of the Korean Fracture Society.2008; 21(4): 267. CrossRef
- Treatment of Failed Intertrochanteric Fractures to Maintain the Reduction in Elderly Patients
- 557 View
- 0 Download
- 1 Crossref

- The Importance of Position of the Distal Fragment in Intertrochanteric Fracture of the Femur using Compression Hip Screw
- Jong Deuk Rha, Hyun Soo Park, Young Bong Park, Chang Suk Lim, Seung Woo Kim
- J Korean Soc Fract 2003;16(4):447-455. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.447
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We reviewed the amount of impaction and the change of neck shaft angle of intertrochanteric fracture of the femur which were treated with compression hip screw according to the fracture type and the displaced state of the distal fragment.
MATERIALS AND METHODS
There were 50 patients who had at least six months follow up, 13 men, and 37 women who were treated from January 1995 to December 2000. We have analysed the amount of impaction (measurement of the ratio between screw length and screw outside barrel length) and the change of neck shaft angle according to the fracture type and the displaced state of the distal fragment. The results were assessed statistically.
RESULTS
The fracture healing was achieved in about 13 weeks. There were 36 stable fracture types and 14 unstable fracture types by Evans classification. The most common osteoporotic singh index was grade II. The mean impaction amount of the fracture site was 5.4 mm and the mean neck shaft angle change was 1.5degrees of varus angulation. The mean tip apex distance was 32 mm. There was no case of lag screw penetration into the joint. There was significant difference in result according to the displaced state of the distal fragment. The amount of impaction was less in cases that anatomically reduced or got the posterolateralization of the distal fragment.
CONCLUSION
The results of our study indicate that the anatomical reduction and posterolateralization of the distal fragment could reduce the amount of impaction and the change of neck shaft angle. We advise that the position of the distal fragment in intertrochanteric fracture of the femur is very important to reduce the failure. -
Citations
Citations to this article as recorded by- Comparison of Bone Mineral Density in Elderly Patients according to Presence of Intertrochanteric Fracture
Sang Ho Moon, Byoung Ho Suh, Dong Joon Kim, Gyu Min Kong, Hyeon Guk Cho
Journal of the Korean Fracture Society.2007; 20(3): 222. CrossRef
- Comparison of Bone Mineral Density in Elderly Patients according to Presence of Intertrochanteric Fracture
- 579 View
- 0 Download
- 1 Crossref

- Loss of Fixation after Internal Fixation of Intertrochanteric Femoral Fracture with Compression Hip Screw
- Jong Oh Kim, Sang Yeol Chang, Joon Gue Moon, Hoon Jeong, Woo Chul Jeong
- J Korean Soc Fract 2003;16(3):334-339. Published online July 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.3.334
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the factors which might affect the loss of fixation after surgical treatment of intertrochanteric fracture with compression hip screw.
MATERIALS AND METHODS
From February 1996 to February 2001, seventy nine cases of intertrochanteric fracture which we operated with compression hip screw was reviewed with minimal follow up for 6 months. There were twelve cases of loss of fixation. The cases were analyzed according to each factors which we thought to affect the loss of fixation. The factors are fracture type by modified Evans classification, Singh index, placement of screw in femoral head, quality of reduction. Then we analyzed these factors with chi square test.
RESULTS
Difference between age group and sex were not thought to be statistically meaningful factors (p>0.05). There were difference of prevalence between two group divided by fracture stability (p<0.05). In cases of superior placement in femoral head, there were more loss of fixation. Displacement of cortex of proximal femur on radiologic AP view other than lateral view showed meaningful difference (p<0.05).
CONCLUSION
Age, sex, Singh index did not affect the loss of fixation. But, next factors as follows affected the loss of fixation; Superior placement of hip screw, unstable fracture pattern, displacement of fracture site more than 5 mm after surgical reduction on radiologic AP view.
- 413 View
- 1 Download

- Stability and Usefulness of Compression Hip Screw in the Treatment of Femur Intertrochanter Fracture in the Elderly
- Jong Oh Kim, Kwon Jae Roh, Yeo Heon Yun, Young Do Koh, Jae Doo Yoo, Jun Mo Jung, Han Cheon Bang, Jae Hak Jung
- J Korean Soc Fract 2003;16(2):128-135. Published online April 30, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.2.128
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the relationship between fracture stability and functional results, and analyze the correlation between stability factors and the outcome in intertrochanteric fractures of the elderly.
MATERIALS AND METHODS
Of the 231 patients, 84 patients with age above 60 were able to follow up for minimum 6 months. We measured the sliding length of the lag screw, varus degree, position of lag screw, reduction status and medialization of distal fragment radiologically. The functional outcome of the treatment was evaluated with the Clawson's result classification and we evaluated the correlation between the radiological results of measurement and the functional recovery depending on the Evans fracture classification.
RESULTS
There were good results in 40 cases out of 51 stable fractures, and in 10 cases out of 33 unstable fractures (p<0.001). In case of sliding of lag screw more than 10 mm, good results were obtained in 4 cases, and poor in 21. And in case of sliding less than 10 mm, good results were obtained in 46, and poor in 13 (p<0.001). But there was no relationship between other radiologic factors and clinical results. In unstable type, there were 12 cases with lag screw sliding more than 10 mm and 10 cases with less than 10 mm. In comminuted type, there were 11 cases with lag screw sliding more than 10 mm and 2 cases with less than 10 mm (p<0.001).
CONCLUSION
The sliding of lag screw more than 10 mm may result in poor outcome. As in comminuted unstable pattern, sliding of lag screw might be excessive, the use of compression hip screw alone is not a good treatment option.
- 392 View
- 1 Download

- Treatment of Trochanteric Fractures of the Femur with Compression Hip Screw-Analysis of Factors associated with Failure of Fixation-
- Chan Hoon Yoo, Hong Tae Kim, Young Soo Byun, Jun Mo Nam, Young Ho Cho, Seong Gun Moon
- J Korean Soc Fract 2002;15(3):312-319. Published online July 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.3.312
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study was performed to analyze the significant factors that may affect failure of fixation in trochanteric fractures of the femur treated with the compression hip screw.
MATERIALS AND METHODS
From May 1995 to July 2000, the authors analyzed 97 cases of trochanteric fracture of the femur treated with the compression hip screw and followed more than one year. We classified the fracture type by Jensen 's method. We used Singh index for the degree of osteoporosis. In the post-operative radiograph, we checked neck-shaft angle, state of reduction, position of the lag screw within the femoral head, tip-apex distance, and sliding distance of the lag screw. The relationship between these factors and failure of fixation was statistically analyzed.
RESULTS
There were 17 cases (17.5%) of failure of fixation ; 15 cases (15.4%) of excessive sliding of the lag screw, 1 case (1%) of cutting out of the lag screw, and 1 case (1%) of valgus malunion. There were significant relationships between failure of fixation and old age over 80, unstable fracture, telescoping reduction, anterior or medial displacement of the distal fragment, and anterior placement of the lag screw within the femoral head.
CONCLUSION
Accurate reduction and avoidance of the placement of the lag screw in the anterior part of the femoral head were important factors to prevent failure of fixation in trochanteric fractures of the femur treated with the compression hip screw.
- 355 View
- 0 Download

- Treatment of Comminuted Trochanteric Fracture with Dynamic Hip Screw and Trochanteric Stabilizing Plate
- Seungki Baek, Youngjoon Choi, Chunghwan Kim, Yoojin Kim, Jaekwang Hwang, Hyungsun Ahn, Hyuntae Ahn, Kyungjun Park, Jaiwoo Cho
- J Korean Soc Fract 2002;15(2):278-285. Published online April 30, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.2.278
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the results of treatment of comminuted femoral trochanteric fracture using dynamic hip screw(DHS) with trochanteric stabilizing plate(TSP) and DHS only.
MATERIALS AND METHODS
we analysed retrospectively 32 cases that has fracture extends over two or more levels of medial cortex(A2 of AO classification) and fracture extends through lateral cortex of femur(A3 of AO classicification) of femoral trochanteric fractures between 1997 and 2000. On simple AP radiograph of the DHS with TSP(n=16) and DHS only group(n=16), we reviewed bony union, slippage of lag screw, lateral displacement of greater trochanter.
RESULT
Bony union was observed in all cases. When bony union is done in follow up radiograph, Mean slippage of lag screw is 14.5mm in DHS only group, 12.6mm in DHS with TSP group and mean lateral displacement of greater trochanter is 9.8mm in DHS only group, 1.2mm in DHS with TSP group.
CONCLUSION
Use of DHS with TSP in comminuted femoral trochanteric fracture is lesser slippage of lag screw and lateral displacement of greater trochanter than DHS only used, and that is better method to maintain fracture reduction and internal fixation in treatment of comminuted femoral trochanteric fractures than DHS only. -
Citations
Citations to this article as recorded by- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
Byung-Woo Min, Kyung-Jae Lee, Gyo-Wook Kim, Ki-Cheor Bae, Si-Wook Lee, Du-Han Kim
Journal of the Korean Fracture Society.2014; 27(2): 120. CrossRef - A Comparison of Intramedullary and Extramedullary Fixations for the Treatment of Reverse Oblique or Transverse Intertrochanteric Femoral Fractures
Yerl-Bo Sung, Jung-Yun Choi, Eui-Yub Jung
Hip & Pelvis.2012; 24(2): 109. CrossRef
- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
- 647 View
- 2 Download
- 2 Crossref

- The Angulation as to the Location of the Lag Screw of Compression Hip Screw in the Intertrochanteric Fracture of the Hip
- Sang Won Park, Kwang Jun Oh, Seung Yong Wang
- J Korean Soc Fract 2002;15(1):15-20. Published online January 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.1.15
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the change of the angulation deformity according to apposition of medial cortex and sliding mechanism as to the location of the lag screw in the intertrochanteric fracture of the Korean femur which neck-shaft angle is relatively small .
MATERIALS AND METHODS
We selected the patients those angulation of femur neck-shaft was within 5 degree in comparison with normal side, and displacement of fracture fragment was within 4mm on the immediate post-operative radiograph. According to Evans classification, all patients were type I fracture. We classified the patients in two groups -stable medial cortex apposition(Group I) was 13 cases, and unstable no apposition(Group II) was 16 cases.
RESULTS
In the Group I, the varus-valgus angulation was average 3.3 degrees when lag screw was positioned at the middle of the femur neck, average 3.6 degrees when lag screw was positioned at the inferior to the femur neck. In the Group II, the varus-valgus angulation was average 6.1 degrees when lag screw was middle of the femur neck, average 1.5 degrees when lag screw was inferior to the femur neck.
CONCLUSION
There is no difference in angulation deformity when the lag screw is inferior or middle of femur neck if medial cortex is contacted, but the angulation deformity is less when the lag screw is inferior to femur neck if medial cortex is not contacted, in intertrochanteric fracture.
- 380 View
- 2 Download

- Treatment of unstable pertrochanteric fracture of the femur using compression hip screw and plate with 6 or more holes
- Jeong Woung Lee, Chi Weon Lee, Doo Hoon Sun, Myung Sang Moon
- J Korean Soc Fract 2001;14(4):592-600. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.592
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The objectives of this study are to observe and report the clinical results of the treatment of unstable pertrochanteric femur fracture extending into subtrochanter or shaft of the femur using compression hip screw and plate with 6 or more holes.
MATERIALS AND METHODS
Between February 1993 and December 1997, 39 patients were treated surgically for unstable pertrochanteric femur fracture. 26 patients who have been followed up over twelve months were included in this study. Surgery was performed within 2 weeks after injury, except one patient who had combined head injury. The fracture was fixed internally with compression hip screw and plate with 6 or more holes, and additional fixations were also performed with Cable wire, interfragmentary screw and Knowles pin. The result was analyzed radiographically and clinically for blood loss, surgery time, bony union period and complication. Average estimated blood loss was 910 cc. Average surgery time was one hundred ten minutes. The complications occurred in 7 cases (27%) ; 1 nonunion, 2 screw loosening and 4 cases of superficial wound infection. There was no case of lag screw penetration to the femoral head or metal failure. The bony union was obtained at average 22 weeks.
CONCLUSION
With use of the compression hip screw and long plate with 6 or more holes for stable internal fixation, we obtained satisfactory results for unstable pertrochanteric femur fracture extending into subtrochanter or shaft of the femur.
- 366 View
- 1 Download

- Comparison Study between Internal Fixation with Compression Hip Screw and Bipolar Hemiarffiroplasty in Unstable Intertrochanteric Fracture
- You Sung Suh, Sai Won Kwon, Ho Won Jung, Jong Seok Park, Byung Ill Lee
- J Korean Soc Fract 2001;14(4):584-591. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.584
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To define the appropriate treatment of unstable intertrochanteric fracture for aged patients by conducting a clinical and roentgenographical comparative analysis of internal fixation with compression hip screw and primary bipolar hemiarthroplasty.
MATERIALS AND METHODS
38 patients aged 65 or above with intertrochanteric fracture of Singh index below grade III or bone mineral density(BMD) -3.0 who had both severe osteoporosis and unstable fracture, from the period of January 1995 to January 2000. The 38 patients had either internal fixation with compression hip screw(18 cases, Group I) or primary bipolar hemiarthroplasty(20 cases, Group II), and were followed-up for at least one year afterwards. To prevent postoperative complication, early ambulation was permitted as early as possible to both groups.
RESULTS
The average age was 76(range 65-87) for Group I and 79.8(range 78-92) for Group II, respectively. 19 patients were diagnosed to have I-c fracture, following Evans Classification. 35 cases(92.1%) were given grade III or below according to the preoperative Singh index, while all cases showed severe osteoporosis with average bone density of -4.26(-6.95 ~ -2.54). 60% of Group II were given very good or above diagnosis following Merle d'Aubignè's postoperative functional outcome, compared with 16.7% of Group I, thus showed statistic difference of p=0.006. The average for postoperative Harris hip score was also higher with 77 points(range 43-95) for Group I than with 86 points(range 57-94) for Group II, thus showed statistic difference of p=0.0216.
CONCLUSION
For aged patients with unstable intertrochanteric fracture, primary bipolar hemiarthroplasty is considered to have better clinical and roentgenographical results, and able to decrease local and general complications, compared with internal fixation with compression hip screw.
- 317 View
- 0 Download

- Treatment of Intertrochanteric Fractures of Femur Using Intramedullary Hip-Screw
- Phil Hyun Chung, Chung Soo Hwang, Suk Gang, Dong Ju Chae, Jong Pil Kim, Joon Han Kim
- J Korean Soc Fract 2001;14(4):575-583. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.575
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We analyze the results of the treatment of intertrochanteric fractures by using intramedullary hip screw.
MATERIALS AND METHODS
We reviewed 34 patients of intertrochanteric fracture who were treated by using of intramedullary hip screw from March 1998 to February 2000, and we classified the fractures by Evans system. 26 cases were treated by closed reduction and internal fixation; 8 cases were by open reduction and internal fixation. We analyzed fracture figure and stability, amount of sliding of lag screw, the change of femur neck-shaft angle, postoperative activity and postoperative complication RESULTS: Bony union was obtained in average 14.3 weeks. Gap of fracture site was formed in 2 cases and crack on entry area of nail was formed in 1 case. Postoperative wound infection occurred in laces and delayed union occurred in 1 case. The change of femur neck-shaft angle showed an average decrease 1.7 degree in stable fractures, 3.5 degree in unstable fractures. Lag screw was sided an average 1.0 mm in stable fractures, 2.6 mm in unstable fractures. Postoperative mobility were analyzed by score of Parker and Palmer, and showing from 7.6 score pretrauma to 3.37 score postoperation in 1 month, 5.0 score postoperation in 3 months, 7.48 score postoperation in 6 months and 7.5 score postoperation in one year.
CONCLUSION
Intramedullary hip screw in intertrochanteric fractures reduced the collapse by processing union of fracture site due to the less decreases of femur neck shaft angle and the shortening by sliding of lag screw
- 392 View
- 1 Download

- Treatment of subtrochanteric fracture - Comparison of treatment efficacy according to internal fixation device -
- Taek Rim Yoon, Sung Man Rowe, Eun Kyoo Song, Jong Yoon Seol, Sang Gyoo Shin
- J Korean Soc Fract 2001;14(2):189-199. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.189
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to compare the clinical results of subtrochanteric fractures which were treated with compression hip screw, intramedullary nailing and Rowe plate.
MATERIALS AND METHODS
From 1991 to 1999, 84 cases of subtrochanteric fractures were treated in Chonnam national university hospital. Among them, 25 cases were treated with compression hip screw, 18 cases with interlocking IM nailing and 32 cases with Rowe plate. Excluding pathologic fracture, there were 24 cases(group A), 16 cases(group B) and 30 cases(group C) of subtrochanteric fractures which were followed over 1 year. Mean follow up period was 18, 21, 24 months each. We compared the fracture pattern, operation time, operation method, additional fixation, bone union and complications among the groups.
RESULTS
We devided subtrochanteric fracture into below class II and above class III based on Seinsheimer classification. The overall clinical results were 1 case below class II, 22 above III in group A, 12 below II, 6 above II in group B, and 4 below II, 26 above III in group C. The average operation time was 153 minutes in group A, 166 in group B, and 150 in group C. Additional wiring was performed in 15 cases in group A, 1 in group B and 6 in group C. Interfragmentary screw fixation was performed only in group A(12 cases). Bone graft was performed in 6 cases in group A, 6 cases in group B and 11 cases in group C. The complications were as follows; delayed union 1 case in group A, 2 cases in group B and 6 cases in group C.; Nonunion only 1 case in group B; varus deformity 4 cases in group B and 2 cases in group C; metal failure 1 case in group B and 1 case in group C.
CONCLUSIONS
In treatment of subtrochanteric fractures, compression hip screw was applied to more communited fractures than intramedullary nail, but with additional fixation safe union and excellent clinical outcomes obtained. For intramedullary nailing, great care should be taken not to produce varus malalignment. In plate fixation, we should keep in mind the possibility of metal failure and varus malalignment. Weight bearing should be delayed. -
Citations
Citations to this article as recorded by- Extra-capsular proximal femoral fractures: a cohort comparison of union and complication rates after ballistic versus blunt trauma
Jordan Cook Serotte, Kevin Chen, Julia Nascimben, Jason Strelzow
European Journal of Orthopaedic Surgery & Traumatology.2025;[Epub] CrossRef - Factors Affecting Time to Bony Union of Femoral Subtrochanteric Fractures Treated with Intramedullary Devices
Jung-Yoon Choi, Yerl-Bo Sung, Jin-Hee Yoo, Sung-Jae Chung
Hip & Pelvis.2014; 26(2): 107. CrossRef - Efficacy of Percutaneous Cerclage Wiring in Intramedullary Nailing of Subtrochanteric Femur Fracture - Technical Note -
Ki-Chul Park, Hee-Soo Kim
Journal of the Korean Fracture Society.2013; 26(3): 212. CrossRef - The Treatment of Subtrochanteric Fracture with Cephallomedually Nail -Minimal Incision and Lowman Clamp Assisted Reduction-
Jang Seok Choi, Do Hyun Moon, Young Tae Noh
Journal of the Korean Fracture Society.2011; 24(4): 301. CrossRef
- Extra-capsular proximal femoral fractures: a cohort comparison of union and complication rates after ballistic versus blunt trauma
- 619 View
- 3 Download
- 4 Crossref

- Treatment of Comminuted Subtrochanteric Fractures of the Femur with Compression Hip Screw
- You Sung Suh, Suk Bum Lim, Hyung Suk Choi, Yon Il Kim, Soo Kyoon Rah, Byung Ill Lee
- J Korean Soc Fract 2001;14(2):181-188. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.181
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study was performed to analyze the weight-bearing ambulation time, bony union time and complications after fixation of comminuted subtrochanteric fractures of the femur with compression hip screw and evaluate its effectiveness. MATERIAL & METHODS: From January 1993 to January 2000, 21 cases of S e i n s h e i m e r's Type IV and Type V comminuted subtrochanteric fractures of femur which were treated by compression hip screw and followed for more than 1 year were analyzed by weight-bearing ambulation time, bony union time and complications.
RESULTS
We recommended partial weight bearing ambulation from 6 weeks after operation and full weight bearing ambulation from 12 weeks after operation. All of 21 cases, primary bony union was achieved and mean time was 16 weeks(range 13 to 25 weeks). 2 cases of mechanical complications were occurred. Also 4 cases of malunion of lesser trochanter and 2 cases of nonunion of lesser trochanter were occurred, but none of them result in limitation of motion, limping nor pain.
CONCLUSIONS
We thought compression hip screw is a good implant for rigid fixation of comminuted subtrochanteric fractures, especially involve intertrochanteric region like Seinsheimer's Type IV and Type V.
- 401 View
- 1 Download

- Operative Treatment of the Femur Intertrochanteric Fracture Using the Gamma nail and the Compression Hip Screw
- Ju O Kim, Jae Il Oh, Sang Moon Yoo, Han Ki Lim
- J Korean Soc Fract 2001;14(2):166-173. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.166
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare and analyze the operative results of compression hip screw with those of gamma nail in the treatment of intertrochanteric fracture of femur.
MATERIALS AND METHODS
We performed retrospective analysis of intertrochanteric fracture of femur using the compression hip screws on 16 cases(stable 8 cases, unstable 8 cases) and compared the results with those of 21 cases(stable 5 cases, unstable 16 cases) of Gamma nail fixation. All the 37 cases were operated between April 1992 and May 1997 and followed for minimal 12 months. We permitted earlier weight bearing for the Gamma nail inserted group(1 week vs 3 weeks). We evaluated the operation time, bleeding amount, intraoperative and postoperative complications, bone union time, neck-shaft angle, and functional assessment by follow up radiographs and clinical results.
RESULTS
The average operation time was shorter in the Gamma nail group than in the compression hip screw group (97+/-23.3 compared with 117+/-35.9 minutes; p<0.05). The average amount of bleeding was lesser in the Gamma nail group than in the compression hip screw group (592 compared with 712 ml: p<0.05). The fracture union time and clinical function of two groups showed no statistically significant difference(p>0.05). During Gamma nail insertion, crack was developed in one femoral shaft which was united after bed rest and delayed weight bearing. Postoperative complications were coxa vara in 3 cases(1 case on Gamma nail, 2 cases on CHS) and cutting out of lag screw in 3 cases(1 case on Gamma nail, 2 cases on CHS), but showed no statistically significant difference between two groups(p=0.781).
CONCLUSION
Early weight bearing can be encouraged for the Gamma nail group and this seemed to be beneficial for the old patients. The Gamma nail fixation is considered as a useful method for the patients with intertrochanteric fracture if it is managed with proper technique. -
Citations
Citations to this article as recorded by- Treatment of Intertrochanteric Fractures Using Targon Proximal Femoral Nails
Il Ho Park, Jong Kyoung Won, Kye Young Han
Hip & Pelvis.2012; 24(2): 117. CrossRef
- Treatment of Intertrochanteric Fractures Using Targon Proximal Femoral Nails
- 746 View
- 0 Download
- 1 Crossref

- Treatment of trochanteric fractures of the femur in osteoporotic patients
- Joo Tae Park, Chang Sung So, Jae Yong Byun, Kyung Ho You, Ho Yeun Hwang
- J Korean Soc Fract 2001;14(1):16-22. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.16
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To determine more useful method by comparing the functional recovery and postoperative complications according to operative methods in treatment of unstable trochanteric fracture of the femur with osteoporotic bone.
MATERIALS AND METHODS
Of 45 cases with unstable femoral trochanteric fracture with osteoporosis who had been able to ambulate before injury, we compared postoperative functional recovery and complications between 25 cases treated by cemented bipolar hemiarthroplasty and 20 cases treated by dynamic compression hip screw.
RESULTS
Of 45 cases who had been treated by cemented bipolar hemiarthroplasty and dynamic compression hip screw, the functional results, according to the rating scale of Merle d Aubigne were rated as above good in 23 cases and 14 cases, respectively and postoperative mechanical complications were found in 2 cases and 7 cases, respectively. There was statistically significant difference(P<0.05).
CONCLUSION
Unstable trochanteric fracture of the femur with osteoporotic bone treated by cemented bipolar hemiarthroplasty showed good functional results and few mechanical complications for short term follow-up.
- 416 View
- 2 Download

- Surgical Treatment of Subtrochanteric Fracture with Compression Hip Screw
- Taek Rim Yoon, Sung Man Rowe, Keun Bae Lee, Jae Il Oh
- J Korean Soc Fract 2001;14(1):1-7. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to review the clinical results of 23 cases of subtrochanteric fractures which were treated with compression hip screw fixation and evaluation of the advantage of lateral position.
MATERIALS AND METHODS
From December 1993 to October 1999, 23 cases(l4 male, 9 female) of subtrochanteric fractures were treated with open reduction and internal fixation using compression hip screw. The mean age was 51.3 years(range, 18-89 years). All operations were done on the standard surgical table in lateral position, and additional fixation was done by supplementary screw fixation or cerclage wiring in 19 cases.
RESULTS
All patients (100%) went on to union on the average of 15 weeks (range l2-28 weeks). There were no complications, such as nonunion, malunion, or fixation loss. There was one delayed union which revealed radiographical bony union at postoperative 7 months.
CONCLUSION
Fixation with compression hip screw with or without additional fixation was thought to be a recommendable method of treatment for subtrochanteric fracture. The surgical procedure with the patient on lateral position enabled the surgeon to do interfragmentory fixation more safely and effectively with less disturbance of soft tissues attached to the fractured fragment.
- 319 View
- 0 Download

- The Result Of Surgical Treatment Of The Femur Unstable Intertrochanteric Fracture Using Compression Hip Screw: Analysis Of Effect Of Degree Of Force On Trauma And Degree Of Osteoporosis
- Ki Do Hong, Sung Sik Ha, Sang Weon Park
- J Korean Soc Fract 2000;13(4):795-803. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.795
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyise the effect of degree of force on trauma and degree of osteoporosis in femoral unstable intertrochanteric fracture's result of treatment using compression hip screw.
MATERIALS AND METHODS
From January 1993 to December 1997, 55 patients who were operated with compression hip screw and followed up for more than 1 year were devided into high and low energy injured group by the mechanism of the trauma and also devided low(gradeIV,V,VI) and high grade osteoporosis group(gradeI,II,III) by Singh's index. We analize and compare the result of treatment in each groups.
RESULTS
The averrage rate of mechanincal complication was 24%. The mechanical complication rate of the high grade osteoporosis group(34%) was higher than low grade osteoporosis group(9%)(p<0.05). The average subsidence of compression screw was 9.9mm and it shows significant difference between low(7.8mm ) and high grade osteoporosis group(11.5mm )(p<0.05). The average increased varus deformity of neckshaft angel during follow up was 3.8degrees and it shows singnificant defference between high energy injuried group(4.6degrees ) and low energy injuried group(2.7degrees)(p<0.05). No difference was seen in each groups for time of bone union(p>0.05). In view of functional recovery by Clawson's method, no difference between pre-injury and postoperative state was seen in 7 cases(22%) in high grade osteoporosis group and 13 cases(57%) in low grade osteoporosis group, thus worse functional recovery was seen in high grade osteoporosis group.
CONCLUSIONS
We observed higher mechanical complication rate, more compression screw subsidence and worse functional recovery in high grade osteoporosis group and more varus deformity in high energy injured group. Thus we need more attension to treatment and follow up in high energy injured, severe osteoporotic unstable intertrochanteric fracture.
- 417 View
- 1 Download

- Effect of Trochanter Stabilizing Plate in Unstable Intertrochanteric Fracture
- Youn Soo Park, Kye Young Han, Hyung Gun Kim
- J Korean Soc Fract 2000;13(4):779-787. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.779
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to investigate the effectiveness of trochanter stabilizing plate (TSP) with compression hip screw(CHS) on the reduction stability, fracture union and sliding of lag screw in unstable intertrochanteric fracture. MATERIAL AND METHOD: From October 1997 to March 1999, 32 cases(group 1) and 20 cases(group 2) who could be followed for more than 1 year were treated with TSP (group 2) and CHS only (group 1) due to unstable intertrochanteric fractures. And two groups were compared clinically and radiologically.
RESULTS
Operation time was longer in group 2 and hospital stay was longer in group 1. Preoperative functions were better in group 1(7.00 points) than in group 2(6.47 points). When postop. function was compared with preop. function, group 1 showed differences on the three months follow-up and six months follow-up. Whereas group 2 only showed difference on the three months follow-up but not on the six months follow-up. There was no difference in the incidence of lag screw sliding. However, there were differences in the extent of sliding between group 1(ave.4.88mm) and group 2(ave.2.88mm) with three months follow-up and six months follow-up (group 1: ave 5.42mm and group 2: ave. 3.03mm). There was a significant difference between group 1(12cases) and group 2(0 case) in greater trochanter lateralization, but shaft medialization between group 1(17cases) and group 2(10cases) showed no difference. Loss of neck-shaft angles between group 1(9cases) and group 2(3cases) were not significantly different. Due to loss of reduction, one case in group 1 was reoperated.
CONCLUSION
Application of TSP is not a difficult procedure and reduce excessive sliding of lag screw. And early fuctional recovery without adverse effect of bone healing is possible. So in unstable intertrochanteric fracture, additional use of TSP is effective. -
Citations
Citations to this article as recorded by- Surgical Treatment of Femoral Unstable Intertrochanteric Fractures in Elderly Patients -Comparative Study between Compressive Hip Screws and Additional Trochanteric Stabilizing Plates-
Kap Jung Kim, Dae Suk Yang, Sang Ki Lee, Won Sik Choy, Kyoung Wan Bae
Journal of the Korean Fracture Society.2011; 24(4): 295. CrossRef - Proximal Femoral Nail Antirotation versus Compression Hip Screw with Trochanter Stabilizing Plate for Unstable Intertrochanteric Hip Fractures
Jae-Young Rho, Sang-Bum Kim, Youn-Moo Heo, Seong-Jin Cho, Dong-Sik Chae, Woo-Suk Lee
Journal of the Korean Fracture Society.2010; 23(2): 161. CrossRef
- Surgical Treatment of Femoral Unstable Intertrochanteric Fractures in Elderly Patients -Comparative Study between Compressive Hip Screws and Additional Trochanteric Stabilizing Plates-
- 520 View
- 2 Download
- 2 Crossref

- Comparison of Bipolar Hemiarthroplasty and Compression Hip screw on Treatment of Elderly Unstable Intertrochanteric Fractrues
- Ik Su Choi, Su In Roh, Dae Yeon Kim, Keun Il Lee, Seung Chan Ko
- J Korean Soc Fract 2000;13(1):56-63. Published online January 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.1.56
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate and compare the clinical outcomes of bipolar hemiarthroplasty and compression hip screw on elderly with unstable intertrochanteric fractures We evaluated the clinical results of 65-year or older elderly patients with unstable intertrochanteric fractures between Jan. 1993 to Dec. 1997. 23 patients underwent compression hip screw treatment and 19 patients were treated with bipolar hemiarthroplasty. Functional evaluation was conducted at 3, 6 and 12 month after the operation by hip rating scale of Merle d'Aubigne. Complications, time to weight bearing and hospitalization period were also investigated.
RESULTS
For the bipolar hemiarthroplasty group, functional scale of good or above were seen in 74%, 72% and 67% of the group at 3 months, 6 months and 12 months. However in the compression hip screw group, the good or above results were shown in 57%, 52% and 43% of the group, thus showing a functional deterioration as time progresses. Comparing the overall clinical outcome, the bipolar hemiarthroplasty group showed better results, complication occurred in 26 cases of compression hip screw group and 8 cases of bipolar hemiarthroplasty group, showing better outcomes in the bipolar hemiarthroplasty group.
CONCLUSION
Comparing the length of hospital stay, time to weight bearing, complication and functional superiority of the treatment for elderly unstable intertrochanteric fractures, the bipolar hemiarthroplasty showed superior clinical outcomes than the compression hip screw. Moreover, patients with more unstable fractures and more severe osteoporosis showed better clinical results with bipolar hemiarthroplasty.
- 363 View
- 0 Download

- Analysis of cause of collapse and Non-union After Internal Fixation of Intertrochanteric Fracture
- Seung Woo Suh, Chang Ryong Hur, Jung Ho Park, Jun Seok Hong, Woo Nam Moon
- J Korean Soc Fract 1999;12(4):812-817. Published online October 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.4.812
-
 Abstract
Abstract
 PDF
PDF - Sixty-five Intertrochanteric hip fractures were analyzed radiologically to study the factors affecting postoperati ye stability. Fractures were evaluated by measuring shortening and angulation, collapse of telescoping device when utilized, and migration of the fixation device within the femoral head. Fractures were classified according to their stability preoperatively and the reduction of lessor trochanteric fracture fragment postoperatively. The failure rate and postoperative stability were then compared on terms of severity of osteoporosis, type of fracture, existence of reduction of lestor trochanter fragment.
Results
indicated that the severity of osteoporosis was not related to the group of fracture, which determines stability of fracture. Regarding the rate of bone union, anatomically reduced groups showed similar rates of bone union(73.8% in average) and degree of sliding of lag screw (4.13mm in average) regardless of fixation of lesser trochanter fragment. On the other hand, malreduced group which failed to obtain anatomical reduction had 26.1% of bone union rates and 10.95mm of sliding of lag screw representing importance of anatomical reduction rather than fixation of lesser trochanteric fracture. In conclusion, there was no correlationthip between severity of oLteoporosis and type of fracture. And it is suggested that unstabae intertrochanteric fractures accompanied by large lesser trochanteric fracture fragment can be provided stability avoiding major complications such as loosening of implant or collapse of fracture fragment if it is fixed with anatomical reduction of fracture even without the fixation of lesser trochanteric fragment.
- 348 View
- 0 Download

- The Results of Surgical Treatment of Intertrochanteric Fractures in the Elderly Patients Aged over 65 years : Comparative Study between Compression Hip Screw and Ender Nail Fixationt
- Byeong Yeon Seong, Chang Min Lee, Dong Sung Park
- J Korean Soc Fract 1999;12(4):802-811. Published online October 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.4.802
-
 Abstract
Abstract
 PDF
PDF - OBJECTIVES
: To analyse the comparative results of surgical treatment with compressive hip screw or Ender nail for intertrochanteric fracture in aged over 65 years. MATERIALS & METHODS : From June 1990 to December 1997, 39 of 55 patients who were operated with compression hip screw or Ender nailing and followed up for more than 1 year. A retrospective survey was completed for 39 intertrochanteric fractures which were operated with compressive hip screw(22 patients, Group 1) or Ender nail(17 patients, Group 2). There was an average follow up of 48 months, with a range of 12 to 84 months. Radiographic measurements were performed in aspects of osteoporosis and fracture classification. Clinical evaluation of follow up was measured as Clawsons evaluation according to the fracture claffification and types of fixation. 23 of 39 cases(59%) were unstable and 26 of 39 cases(66.6%) showed below grade III in osteoporosis. Age, cause of fracture, fracture classification, accompanying diseases and Singhs index were identical to both group.
RESULTS
The mean radiologic bone union period was 16.4 weeks. The rate of complication was 7 cases(31.8%) in group I and 8 cases(47.0%) in group II. The rate of mortality was 3 cases(13.6%) in group I and 3 cases(17.6%) in group II. Satisfactory rate was 20 of 22cases(90.9%) in group I and 14 of 17 cases(82.3%) in group II.
CONCLUSION
: We suppose that compressive hip screw fixation for the elderly over 65 years who had intertrochanteric fracture and medical problem, produced good results as comparing to Ender nail fixation. The clinical satisfactory rate were superior in the compressive hip screw group comparing to Ender nail group. Cement fixation for eldly could help to fixate more in compression hip screw.
- 435 View
- 0 Download

- Problems of compression Hip Screw for the Treatment of Intertrochanteric Fracture in Elderly Patients
- Kwon Jae Roh, Jong Oh Kim, Hyung Ho Kim
- J Korean Soc Fract 1999;12(3):502-508. Published online July 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.3.502
-
 Abstract
Abstract
 PDF
PDF - The principle in the treatment of an elderly patient with an intertrochanteric fracture has swung from traction to internal fixation due to complication such as pneumonia, skin ulcer, and thromboernbolic disease, etc. Many surgeons have used sliding compression screw for trochanteric fracture fixation which was regarded as a most effective device to manage the fracture. but, they have reported several risk factors to cause fixation failure such as screw impaction or loosening, because of osteoporosis, large defect on posteromedial aspect of neck, eccentric fixation of lag screw. The aim of the present investigation was to study the relationships between the type of fracture, the trabecular bone grading of proximal femur, reduction status, the implant position and the extent of impaction or loosening of the comression screw. We studied 47 elderly patients(age>60) who were managed using of compression hip screw as operative management and followed more than 6 months after operative treatment at Department of orthopaedic surgery, Ewha womens university Mokdong hospital from 1994 to 1998. The results were as follows 1. Screw impaction or loosening was developed in 7 cases of 47 cases after internal fixation. 2. Of 7 cases, 2 cases were stable fracture(modified Evans type I, II) and 5 cases unstable (modified Evans type III, IV, V). 3. Of 7 cases, 3 cases were high trabecula grade(grade VI, V, IV), 4 cases were low trabecula grade(grade I, II, III). 4. No siginificant diffierence of impaction or loosening development was in screw position. 5. Of 7 cases, 2 cases were anatomical reduction and 5 cases medial reduction.
-
Citations
Citations to this article as recorded by- Treatment of Senile Osteoporotic Intertrochanteric Fracture using Proximal Femoral Nail
Dong-Hui Kim, Sang-Hong Lee, Young-Lae Moon, Jun-Young Lee, Kun-Sang Song
Journal of the Korean Fracture Society.2007; 20(3): 215. CrossRef
- Treatment of Senile Osteoporotic Intertrochanteric Fracture using Proximal Femoral Nail
- 585 View
- 1 Download
- 1 Crossref

- Treatment of Unstable Intertrochanteric Fractures of the Femur - Comparative analysis of the postero-medial fixation with or without additional screw -
- Jin Hong Ko, Bum Gu Lee, Do Hyun Moon, Young Sung Kim
- J Korean Soc Fract 1998;11(3):487-494. Published online July 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.3.487
-
 Abstract
Abstract
 PDF
PDF - An unstable intertrochanteric fracture lacks continuity of the bone cortex on the opposing surfaces of the proximal and distal fragments. This cortical deficit is due to either comminuti- On on the medial aspect of the neck(calcar-region) or a large and separate posterior trochan-teric fragment. Treatment of unstable intertochanteric fracture have taken method to restore bony contact medially and posteriorly by anatomical reduction or displacement osteotomy. The authors analyzed the 60 unstable intertrochanteric fractures treated by anatomic reduction and internal fixation with a compression hip screw from January 1990 to December 1995. We made a comparative analysis of the postero-medial fixation with additional screw(Group I) and no fixation group(Group II). We tried to find the difference of operation time, blood loss, union time, weight bearing time, neck-shaft angle, sliding length of lag screw and complication rate in two groups. The results were obtained as follows: 1. The mean union time was 11.5 weeks in the Group I and 12.7 weeks in the Group II (p>0.05). 2. The mean weight bearing time was 6.1 weeks in the Group I and 8.3 weeks in the Group II (p<0.05). 3. The decrease of neck-shaft angle was 2.3 degree in the Group I and 5.2 degree in the Group II(p<0.05). 4. The sliding length of lag screw was 5.8mm in the group I and 11.2mm in the group II(p< 0.05). 5. The lower complication rate was obtained in the group I than in the Group II, but two groups showed no significance by statistical analysis. In conclusion, the postero-medial fixation with additional screw in the treatment of unstable intertrochanteric fracture of the femur are suggested that medial cortical stability can be gained and early weight-bearing can be allowed.
- 453 View
- 1 Download

- Treatment of Intertrochanteric Fractures of the Femur using Compression Hip Screw in the Senile Osteoporosis
- Eui Hwan Ahn, In Whan Chung, Jeong Hwan Oh, Hyuck Jun Lee
- J Korean Soc Fract 1998;11(1):168-174. Published online January 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.1.168
-
 Abstract
Abstract
 PDF
PDF - The intertrochanteric fracture of the femur are seen in elderly patients who are highly vulnerable to generalized osteoporosis and various senile disease. Firm internal fixation and early ambulation is a goal of treatment. The morbidity and mortality after fracture remain high despite of the development of various devices. For this purpose, compression hip screw becomes popular recently. The purpose of this report is to assess the availability of compression hip screw in the intertrochanteric fracture in the senile osteoporosis by the review of 107 cases from Jan. 1990 to Jan. 1996. The result were as follows : 1. Eighty-three cases(77.6%) were unstable fractures. 2. The lag screw position in the femoral head of 76 cases(71%) were centerd 3. The average length of sliding of the lag screw was 9.9mm. 4. Satisfactory results were obtained in 91% of patients by the functional class of Clawson.
- 457 View
- 0 Download

- Comparison of Hemiarthroplasty and Compression Hip Screw on Elderly Unstable Intertrochanteric Fractures
- Chung Nam Kang, Jong Oh Kim, Dong Wook Kim, Young Do Koh, Sang Hoon Ko, Ki Woong Lee
- J Korean Soc Fract 1997;10(4):738-745. Published online October 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.4.738
-
 Abstract
Abstract
 PDF
PDF - Intertrochanteric fractures of the femur usually occur in the elderly and osteoporotic patients. These appear to be increasing in frefuence and are usually unstable. Sixthy two cases were treated ai our hospital from September 1993 through October 1995. 29 elderly patients underwent bipolar hemiarthroplasty and 33 patients underwent internal fixation with compression hip screw(C.H.S). The results were as follows ; 1. Functional results according to hip rating scale of Merle D,Aubiigne was superior in bipolar group. 2. The incidence of postoperative complications was much fewer in bipolar group than in compression hip screw group. 3. In casees of definite osteoporosis with Singhs index below 3 and Evans unstable type frartures, the incidence of mechanical complications was increased, especially in compression hip screw group. 4. There was no siginificant difference between 2 groups in operative time and blood loss.
-
Citations
Citations to this article as recorded by- Fixation of Greater Trochanter Using an AO Trochanteric Reattachment Device (AO TRD) in Arthroplasty for Intertrochanteric Femur Fracture of Elderly Patients
Weon-Yoo Kim, Young-Yul Kim, Jae-Jung Jeong, Do-Joon Kang
Hip & Pelvis.2013; 25(4): 274. CrossRef - Hemiarthroplasty for Hip Fractures in Elderly Patients over 80 Years Old - Comparative Analysis between Femoral Neck Fracture and Intertrochanteric Fracture -
Chae-Hyun Lim, Young-Yool Chung, Jeong-Seok Kim, Chung-Young Kim
Hip & Pelvis.2013; 25(1): 44. CrossRef - Hip Arthroplasty Using Collarless Polished Tapered Stem -Minimum 2 Years Follow-up Results-
Yerl-Bo Sung, Jung-Yun Choi, Su-Chan Oh
Hip & Pelvis.2012; 24(1): 18. CrossRef - Comparison between the Results of Internal Fixation Using Proximal Femur Nail Anti-rotation and Bipolar Hemiarthroplasty in Treatment of Unstable Intertrochanteric Fractures of Elderly Patients
Sung-Hwan Kim, Soo-Won Lee, Gyu-Min Kong, Mid-Um JeaGal
Hip & Pelvis.2012; 24(1): 45. CrossRef - Cemented Bipolar Hemiarthroplasty for Intertrochanter Fracture in Elderly Patients - Minimum 2-Years Follow-up Results -
Sung Kwan Hwang, Dong Hyun Kang, Tae Yeon Cho, Chang Ho Yi
Hip & Pelvis.2010; 22(3): 209. CrossRef
- Fixation of Greater Trochanter Using an AO Trochanteric Reattachment Device (AO TRD) in Arthroplasty for Intertrochanteric Femur Fracture of Elderly Patients
- 525 View
- 0 Download
- 5 Crossref

- Effect of Unreduced Lesser Trochanteric Fracture on Stability in Intertrochanteric Fracture of Femur
- Seung Woo Suh, Jeong Ho Park, Jong Kun Oh, Kyung Wook Nah, Tae Hyeon Kim, Woo Nam Moon
- J Korean Soc Fract 1997;10(3):529-533. Published online July 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.3.529
-
 Abstract
Abstract
 PDF
PDF - Unstable intertrochanteric hip fractures are characterized by comminution of the posteromedial cortex, resulting in a fragment of variable size containing the lesser trochanter. Stability can be provided by transfixion of the lesser trochanteric fracture fragment with a screw. However, fixation of lesser trochanteric fragment is difficult, time-consuming, and often unsuccessful. Controversy exists as to whether it is necessary to perform reduction and fixation of this fragment. A radiological review of 61 intertrochanteric fractures treated with compression screw was made to study the effect of unreduced lesser trochanteric fracture on fracture healing and stability in unstable intertrochanteric fractures accompanied by lessor trochanteric fracture. Analysis were made on terms of rate of bone union, maintenance of reduction by comparing between anatomically reduced group with/without lesser trochanteric fracture and malreduced group with lesser trochanteric fracture. Anatomically reduced groups with/without lessel trochanteric fracture showed similar rates of bone union(88.3% in average) and degree of sliding of lag screw(3.74mm in average) regardless of fixation of lesser trochanter. On the other hand, unreduced group had 33.3% of bone union rates and 9.80mm of sliding of lag screw representing importance of anatomical reduction rather than fixation of lesser trochanteric fracture. In conclusion, it is suggested that unstable intertrochanteric fractures accompanied by large lesser trochanteric fracture fragment can be treated without fixation of lesser trochanteric fragment avoiding major complicatioins such as loosening of implant or collapse of fracture fragment.
- 436 View
- 1 Download

- Comparison of Compression Hip Screw, Captured Hip Screw and Gamma-Locking Nail in Intertrochanteric Fracture of Femur
- Eu Seup Chung, Kyung Seo Choi, Min Ki Kim, Jong Bong Lee
- J Korean Soc Fract 1996;9(4):876-883. Published online October 31, 1996
- DOI: https://doi.org/10.12671/jksf.1996.9.4.876
-
 Abstract
Abstract
 PDF
PDF - It is well known that most of the intertrochanteric fractures of femur occur in elderly patients with osteoporosis and poor general conditions. So, there are many problems in the treatment of intertrochanteric fractures of femur due to osteoporosis and unstable patterns of fracture and poor general conditions in clderly patients. Various devices have been developed and the results of treatment have been improved, but the morbidity and the mortality still remain high. The authors analysed 33 cases of compression hip screw(group 1), 19 cases of captured hip screw(group 2), and 13 cases of Camma-locking nail(group 3) amomg 65 cases of intectrochanteric fracture of femul operated at Presbyterian Medical Center from Jan.1990 to Aug.1994. We compared the intraoperative and postoperative complications amomg the three devices, and obtained the following results; 1. The incidences of fixation failure were not sigmificant among the three groups. 2. The lag screw penetration of femoral head and angulation were higher in Gamma-locking nail group(23%) among the three groups. 3. Most of anterior displacement of distal fragment and severe impaction of fracture site were occured in unstable fracture and higher in captured hip screw group(16%), and none in Camma locking nail group. 4. In Gamma-locking nail group, severe impaction at fractuie site was not found but the lag screw penetration of femoral head and angulation were higher. In the other two groups, the results were reverse.
- 332 View
- 0 Download

- Primary Bipolar Hemiarthroplasty Compared with Compression Hip Screw on Treatment of Elderly Unstable Intertrochanteric Fractures
- Jae Ick Lee, Myung Hwan Son, Seong Geun Heo, Young Ho Gwun, Jae Hong Park
- J Korean Soc Fract 1996;9(2):401-408. Published online April 30, 1996
- DOI: https://doi.org/10.12671/jksf.1996.9.2.401
-
 Abstract
Abstract
 PDF
PDF - The incidence of intertrochanteric fracture of the femur appears to be increasing, Particularly the more unstable comminuted fracture types are increasing, paralleling increased longevity in the population. Fourteen cases were treated with primary bipolar hemiarthroplasty and eighteen cases were treated with compression hip screw at the Department of Orthopaedic Surgery of Pusan City Medical Center from June 1991. to June 1993. The results obtained were as follows; 1. In the bipolar hemiarthroplasty group, rehabilitation was easier and faster, and the incidences of pressure sore, pulmonary infection & atelectasis were significantly lower. 2. The early walking with full weight bearing that the bipolar hemiarthroplasty made possible is considered to be a major contributing factor to those results.
-
Citations
Citations to this article as recorded by- Comparison between the Results of Internal Fixation Using Proximal Femur Nail Anti-rotation and Bipolar Hemiarthroplasty in Treatment of Unstable Intertrochanteric Fractures of Elderly Patients
Sung-Hwan Kim, Soo-Won Lee, Gyu-Min Kong, Mid-Um JeaGal
Hip & Pelvis.2012; 24(1): 45. CrossRef
- Comparison between the Results of Internal Fixation Using Proximal Femur Nail Anti-rotation and Bipolar Hemiarthroplasty in Treatment of Unstable Intertrochanteric Fractures of Elderly Patients
- 554 View
- 0 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


