Search
- Page Path
- HOME > Search
Review Articles
- Current concepts and applications of bone graft substitutes in orthopedic surgery
- Jae Ho Cho, Hyung Keun Song
- J Musculoskelet Trauma 2025;38(4):169-177. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00248
-
 Abstract
Abstract
 PDF
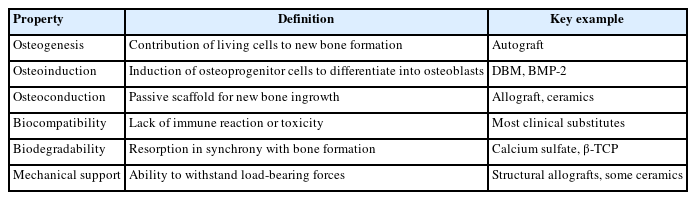
PDF - Bone defects, which often arise from high-energy injuries, infections, tumor resections, or nonunions, represent a persistent challenge in orthopedic trauma surgery. Autologous bone grafting remains the gold standard due to its unique combination of osteogenic, osteoinductive, and osteoconductive properties. However, issues such as donor site morbidity, limited graft volume, and increased surgical time have driven the development of bone graft substitutes. These substitutes vary widely in origin, composition, biological activity, and mechanical characteristics, encompassing allografts, xenografts, synthetic materials, and biologically enhanced constructs. This review outlines the fundamental biological principles underlying bone regeneration—including osteogenesis, osteoinduction, and osteoconduction—and addresses additional key factors such as biocompatibility, biodegradability, and mechanical strength. Current bone graft materials are classified by biological origin and functional characteristics, with an emphasis on their use in trauma surgery. Particular attention is given to the clinical applications, indications, and limitations of allograft-based solutions (such as structural allografts and demineralized bone matrix), synthetic ceramics (including calcium phosphate and bioactive glass), and biologically enhanced options, such as recombinant growth factors and stem cell therapies. In trauma settings, graft selection must be tailored to the characteristics of the defect, mechanical demands, the biological environment, and patient-specific factors. Integration with surgical technique and fixation is crucial for optimizing outcomes. Although modern substitutes show promise, none fully replicate the complex biology of autografts. Looking ahead, emerging technologies such as 3D printing, nanotechnology, and smart biomaterials offer exciting possibilities but face translational challenges. This review aims to provide practicing orthopedic surgeons with a concise, evidence-based overview of bone substitute options and their roles in trauma care. By applying core biological principles and clinical judgment, surgeons can better navigate the expanding array of graft materials to improve outcomes for patients with complex skeletal defects.
-
Citations
Citations to this article as recorded by- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
Seungyeob Sakong, Seokjun Hong, Wonseok Choi, Seonghyun Kang, Jae-Woo Cho, Whee Sung Son, Jeong-Seok Choi, Chang-Jin Yon, Won-Tae Cho, Jong-Keon Oh
Journal of Clinical Medicine.2026; 15(3): 1176. CrossRef
- Safety and Efficacy of rhBMP-2 for Treating Acute Traumatic Fractures of the Upper and Lower Extremities: A Multicenter Prospective Study
- 4,319 View
- 100 Download
- 1 Crossref

- Bone Substitutes: From Basic to Current Update
- Jong Seong Han, Hyung Keun Song
- J Korean Fract Soc 2020;33(4):238-244. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.238
-
 Abstract
Abstract
 PDF
PDF - Bone substitutes are being used increasingly in bony surgery as more than two million bone grafts are performed worldwide per year. Autobone grafts represent the gold standard for bone grafting, but morbidity and limited availability are the main problems. Allobone grafts are osteoconductive, but there are still concerns regarding the infection risks, costs, and donor availability issues. As an alternative, widely used ceramic-based synthetic bone substitutes are based alternatively on calcium (hydroxyapatite, tricalcium phosphate, calcium sulfate, calcium phosphate). Ceramic-based bone substitutes are osteoconductive, but they are weaker than cortical bone and are not osteoinductive. Bone morphogenic protein, demineralized bone matrix, and platelet-rich plasma are used to obtain an osteoinductive function. Recently, cell-based and gen-based bone substitutes were developed and studied. This paper reviews the basic information and the latest concepts on bone grafts and bone substitutes.
-
Citations
Citations to this article as recorded by- Tannic acid-modified magnesium oxychloride bone cement with high water resistance and osteogenic properties
Junying Chen, Yijia Guan, Yue Yang, Tingting Ma, Jinlun Feng, Wenjie Guo, Qifang Wang, Yanru Zhang, Jianguo Liao
Ceramics International.2024; 50(24): 53407. CrossRef - Surface modification of magnesium with a novel composite coating for application in bone tissue engineering
Jorgimara de O. Braga, Diogo M.M. dos Santos, Fernando Cotting, Vanessa F.C. Lins, Nádia M. Leão, Daniel C.F. Soares, Eric M. Mazzer, Manuel Houmard, Roberto B. Figueiredo, Eduardo H.M. Nunes
Surface and Coatings Technology.2022; 433: 128078. CrossRef
- Tannic acid-modified magnesium oxychloride bone cement with high water resistance and osteogenic properties
- 1,145 View
- 12 Download
- 2 Crossref

- Bone Substitutes and the Advancement for Enhancing Bone Healing
- Dong Hyun Lee, Ji Wan Kim
- J Korean Fract Soc 2017;30(2):102-109. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.102
-
 Abstract
Abstract
 PDF
PDF - With an aging population and the development of surgical techniques, there is a growing demand for bone reconstruction in areas of trauma, arthroplasty, and spinal fusion Although autogenous bone grafting may be the best method for stimulating bone repair and regeneration, there are still problems and complications, including morbidity related to bone harvesting and limitation of harvest amount. Allogeneic bone grafts have a limited supply and risk of transmission of infectious diseases. Over the past several decades, the use of bone substitutes, such as calcium phosphate, has increased; however, they have limited indications. Biomedical research has suggested a possibility of stimulating the self-healing mechanism by locally transmitting the external growth factors or stimulating local production through a gene transfer. In this review, we evaluate recent advances, including bone graft, bone substitutes, and tissue engineering.
-
Citations
Citations to this article as recorded by- Calcium phosphate injection technique for treatment of distal radius fracture
Dae-Geun Kim, Byung Hoon Kwack
Medicine: Case Reports and Study Protocols.2021; 2(9): e0117. CrossRef - Experimental Study ofDohongsamul-tang(Taohongsiwu-tang) on Fracture Healing
Hyun Ju Ha, Min-Seok Oh
Journal of Korean Medicine Rehabilitation.2020; 30(2): 47. CrossRef
- Calcium phosphate injection technique for treatment of distal radius fracture
- 665 View
- 0 Download
- 2 Crossref

Original Article
- The Efficiency of Additional Fixation of the Alternative Bone Substitute in Unstable Intertrochanteric Fractures of Femur Treated with Gamma Nail
- Jong Oh Kim, Young One Ko, Mi Hyun Song
- J Korean Fract Soc 2011;24(1):1-6. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the efficiency of additional fixation of the alternative bone substitute in unstable intertrochanteric fractures treated with gamma nail and alternative bone substitute and only with gamma nail.
MATERIALS AND METHODS
Radiologic comparison was done between forty-four patients of unstable intertrochanteric fracture (AO type A2.2, A2.3) during six months. The patients were divided into two groups, a group treated with gamma nail and alternative bone substitute (22 patients, group 1) and another group treated only with gamma nail (22 patients, group 2). Postoperative reduction status, Cleveland index, Tip-apex distance and complications during the follow-up period was compared. Lag screw slippage and femoral neck-shaft angle change were measured between two groups.
RESULTS
No significant difference of reduction status, Cleveland index and Tip-apex distance was found. In group II, there was a 1 more case of cutting-out of the lag screw, but also there was a significant difference. Lesser change in lag screw slippage and neck-shaft angle change was investigated.
CONCLUSION
As there are lesser lag screw slippage and neck-shaft angle change, alternative bone substitutes applied in unstable intertrochanteric fractures seems to be useful in maintaining reduction and preventing failure of internal fixation when proper reduction and screw insertion is performed.
- 555 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


