-
Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
-
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
-
J Musculoskelet Trauma 2024;37(4):175-183. Published online October 25, 2024
-
DOI: https://doi.org/10.12671/jmt.2024.37.4.175
-
Correction in: J Musculoskelet Trauma 2025;38(1):40
-
 Abstract Abstract
 PDF PDF
- Purpose
The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
Materials and Methods
The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
Results
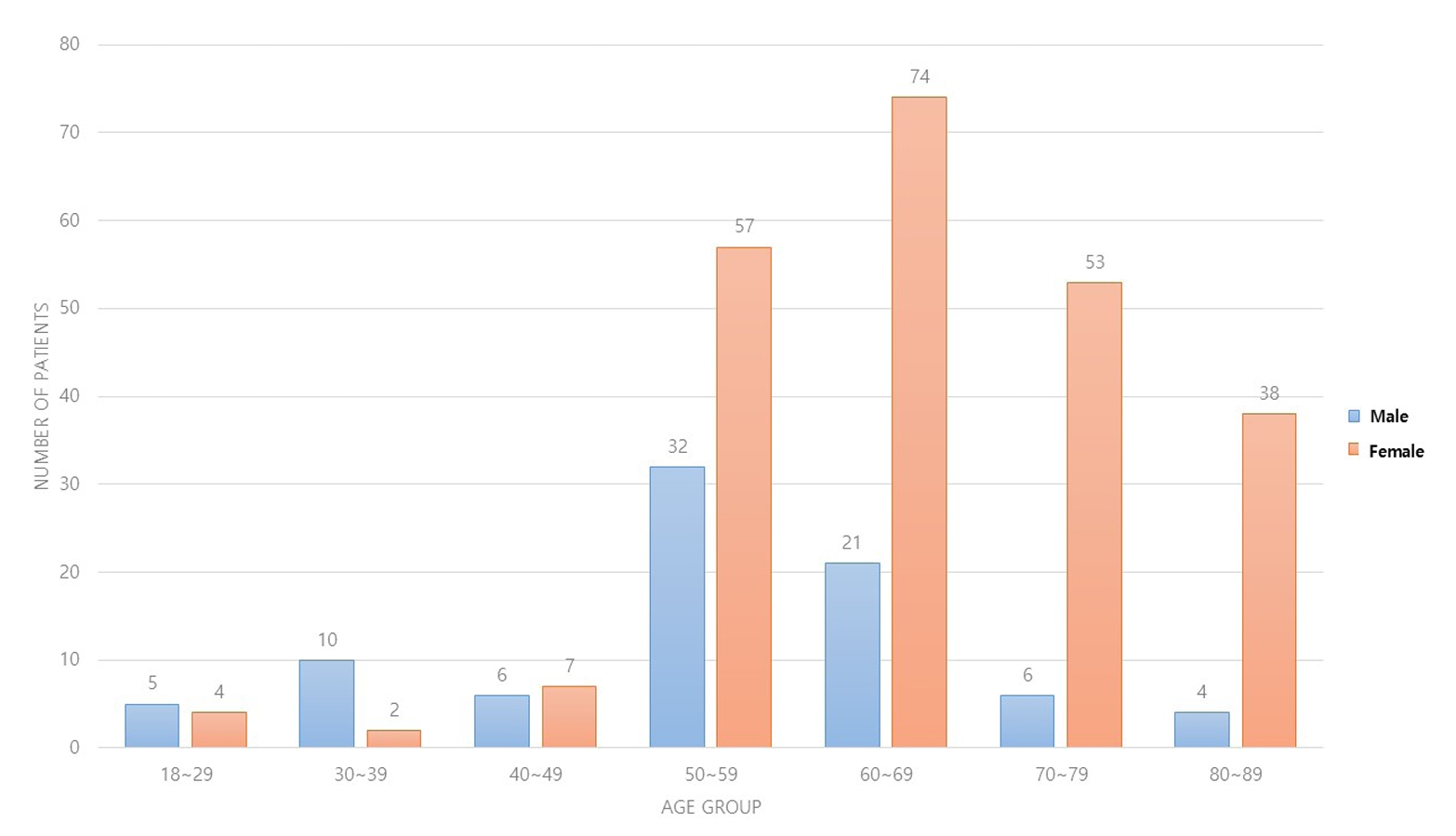
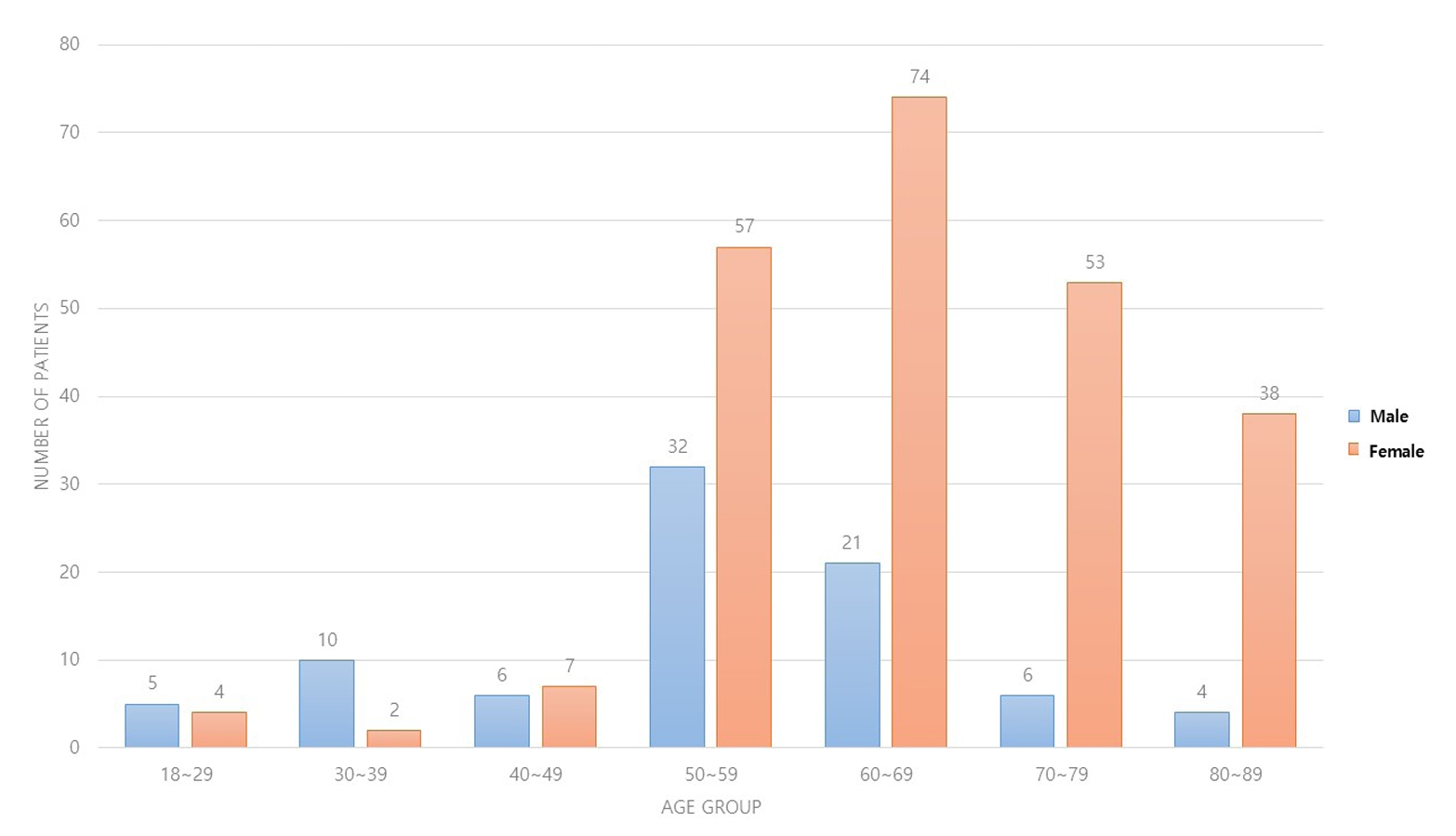
Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
Conclusion
In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates.
-
Citations
Citations to this article as recorded by  - Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef
-
431
View
-
40
Download
-
1
Crossref
-
Current Concepts in Management of Phalangeal Fractures
-
Yohan Lee, Sunghun Park, Jun-Ku Lee
-
J Korean Fract Soc 2022;35(4):169-181. Published online October 31, 2022
-
DOI: https://doi.org/10.12671/jkfs.2022.35.4.169
-
-
 Abstract Abstract
 PDF PDF
- This review focused on the research published to date on the treatment of phalangeal fractures according to the anatomical location of the finger bones, excluding the thumb. In many finger fracture cases, conservative treatment should be prioritized over surgical treatment. The three determinants of surgical treatment are the presence of an intra-articular fracture, the stability of the fracture itself, and the degree of damage to the surrounding soft tissues. Surgical treatment is recommended when bone fragments of 3 mm or more and distal phalanx subluxation are present in the bony mallet finger, and the main surgical treatment is closed reduction and extension block pin fixation. It is essential to pay attention to rotational deformation asf ractures occur proximally. Since intra-articular fractures can cause stiffness and arthritis in the future, a computed tomography scan is recommended to confirm the fracture pattern. These fractures require anatomical reduction of the bone fragments within the joint, and the instability of the joint itself must be corrected. There are no superior surgical treatment methods. It is therefore advantageous for the surgeon to select a surgical method that he is familiar with and confident of performing, considering the fracture itself and various patient-related clinical factors. Nonunion is rare as a complication of a finger fracture, and finger stiffness is the most common complication. Ensuring rapid joint movement as soon as possible can reduce finger stiffness.
-
Primary Open Reduction and Plate Fixation in Open Comminuted Intra-Articular Distal Radius Fracture
-
Jun-Ku Lee, Soonchul Lee, Weon Min Cho, Minkyu Kil, Soo-Hong Han
-
J Korean Fract Soc 2021;34(1):16-22. Published online January 31, 2021
-
DOI: https://doi.org/10.12671/jkfs.2021.34.1.16
-
-
 Abstract Abstract
 PDF PDF
- Purpose
There are no standard surgical treatments for open distal radius fractures (DRFs), and the fracture fixator is chosen by the surgeon’s own experience. This study compared the outcomes of open reduction and volar locking plating (OR VLP) between closed and open AO-OTA type C3 DRFs.
Materials and Methods: Patient data were retrospectively collected between January 2010 and December 2018. Only patients aged >18 years with AO-OTA C3 DRFs were included. After further exclusion, the patients with DRFs were divided into two groups: 13 patients with open DRFs in Group 1 and 203 patients with closed DRFs in Group 2. Data on the patient characteristics and treatment-related factors were further investigated. For the radiological evaluation, the radial height, volar height, and volar titling were measured based on the final plain radiography, and the union time was measured. The wrist range of motion (ROM), pain visual analogue scale score, and modified Mayo wrist score for function were measured at the final outpatient follow-up. Finally, the complications associated with OR VLP fixa-tion were investigated.
Results: In the demographic comparison, the patients with open fractures were older (mean age, 62years) than those with closed fractures (mean age, 57 years), without a statistically significant differ-ence. The patients with open DRFs had longer antibiotic therapy and hospital stay durations. Although they presented a higher radial inclination, with statistical significance, the clinical implication was low with a mean difference of 3°. No significant differences were observed for the remaining radiological parameters, wrist ROM, and functional scores. An open DRF did not increase the complication rates,including deep infection.
Conclusion: Depending on the expertise of the operating surgeon, the primary OR VLP fixation in open intra-articular comminuted DRF did not increase the incidence of deep infections and yielded similar outcomes to a closed intra-articular comminuted DRF.
-
Axillary Artery Rupture after Shoulder Dislocation That Was Treated with a Self-Expanding Stent - A Case Report -
-
HaengJin OHE, Daehyun Hwang, Inkeun Park, Minki Lee, Jun-Ku Lee
-
J Korean Fract Soc 2020;33(4):217-221. Published online October 31, 2020
-
DOI: https://doi.org/10.12671/jkfs.2020.33.4.217
-
-
 Abstract Abstract
 PDF PDF
- raumatic shoulder dislocations are one of the most common major dislocations in the general population. Injury to major vessels is rarely reported as a complication of shoulder dislocations. This case report presents the traumatic dissection of the axillary artery after a simple shoulder dislocation that was managed successfully with the placement of a self-expanding stent. With the clinical manifestations of a brachial plexus injury and progressive vascular compromise in the affected arm, a major vascular injury was detected on an angiogram, and a self-expanding stent was deployed. Through immediate diagnosis and prompt intervention, serious complications, such as hypovolemic shock and even death, were averted, ultimately achieving a favorable patient outcome.
-
Tendon Healing: A Review of Basic Science and Current Progress
-
Young Woo Kwon, Pei Wei Wang, Jun-Ku Lee
-
J Korean Fract Soc 2020;33(4):227-237. Published online October 31, 2020
-
DOI: https://doi.org/10.12671/jkfs.2020.33.4.227
-
-
 Abstract Abstract
 PDF PDF
- The tendon connects the muscles to the bones and transmits the loads generated by the muscles to the bones to move the joints, support the joints, and provide stability to the joints. Approximately 30% of patients complaining of musculoskeletal pain are associated with tendon disease, and approximately 50% of musculoskeletal injuries are caused by a tendon injury. Despite this frequent treatment of tendon damage, studies on the basic biology that provide scientific evidence for treatment, such as development, tendon injury, and healing, are still very limited. This review first summarizes the classification and composition of the tendon identified so far, the surrounding tissue, and the blood supply to the tendon. The limitations of the tendon recovery process after a tendon injury are also discussed.
Finally, this review examines ways to improve tendon recovery and the biological approaches and tissue engineering that have been currently studied. In conclusion, innovative progress in promoting tendon healing has not been achieved despite the many advances in the basic structure of the tendon, and the cell and regulatory molecular factors involved in tendon recovery. Biological approaches and tissue engineering, which have become a recent issue, have shown many possibilities for the recovery of damaged cases, but further research will be needed until clinical application.
|