Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Osteoporotic Sacral Fracture
Article information
Abstract
Abstract
Purpose
The prevalence of osteoporotic sacral fractures is increasing. Traditionally, conservative treatment is the 1st option, but it can increase the risk of comorbidity in the elderly. To reduce the complications and allow early mobility, iliosacral screw fixation with cement augmentation will be one of the treatment options for patients with osteoporotic sacral fractures.
Materials and Methods
This study reviewed 25 patients (30 cases) who had undergone percutaneous iliosacral screw fixation with cement augmentation for osteoporotic sacral fractures from July 2012 to December 2018 with a minimum follow up of six months. The clinical outcomes were assessed using the measures of pain (visual analogue scale [VAS] score), hospital stay and the date when weightbearing started. All patients were evaluated radiologically for pull-out of screw, bone-union, and cement-leakage.
Results
Bone union was achieved in 30 cases (100%). The mean duration of the hospital stay was 24 days (4–66 days); weightbearing was performed on an average nine days after surgery. The VAS scores immediately (3.16) and three months after surgery (2.63) were lower than that of the preoperative VAS score (8.3) (p<0.05). No cases of cement-leakage or neurologic symptoms were encountered. Two patients (6.7%) experienced a pulling-out of the screw, but bone-union was accomplished without any additional procedures.
Conclusion
Percutaneous iliosacral fixation with cement augmentation will be an appropriate and safe surgical option for osteoporotic sacral fractures in the elderly in terms of early weightbearing, pain reduction, and bone-union.
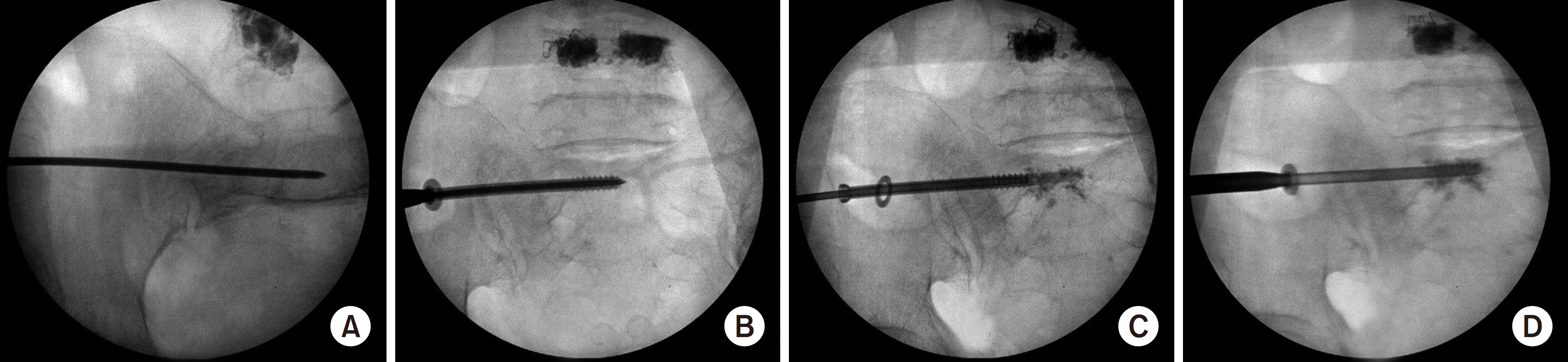
A) Guide-wire was inserted through the fracture sited guided C-arm. (B) A cannulated screw was then inserted. (C) The cannulated screw was pulled out as long as the thread of the screw. Contrast media injected. (D) Cement (2–3 ml) was injected into the sacrum in the region of screw thread. The cannulated screw was then inserted.
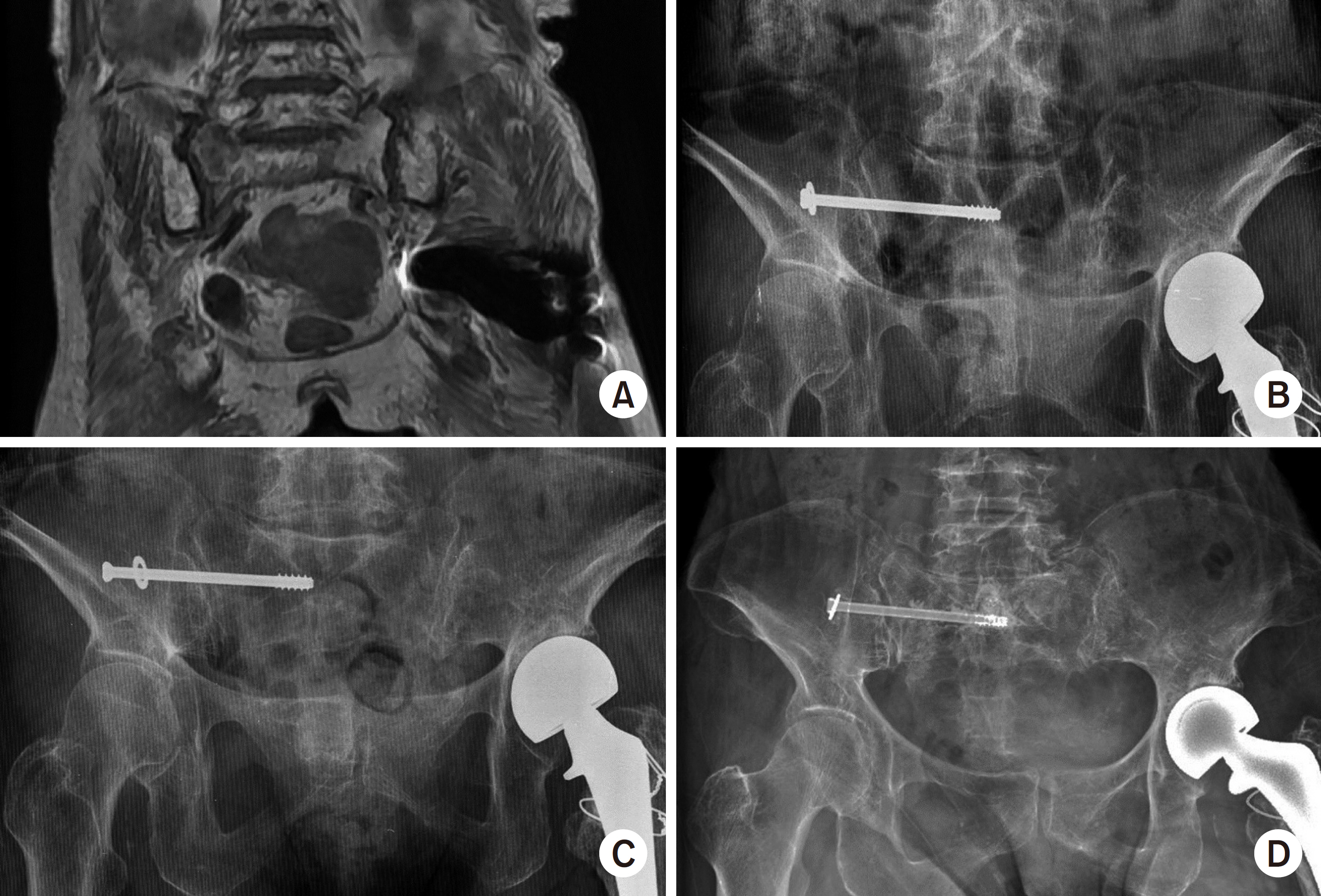
A 78-year-old female patient had a sacral fracture without trauma. Her bone mineral density was −3.9. (A) Right sacral fracture was diagnosed by magnetic resonance imaging. (B) Percutaneous screw fixation was performed. (C) There is a pull-out screw within four days after surgery. (D) Re-operation was performed with cement augmentation. Bone union was achieved within six months of surgery.
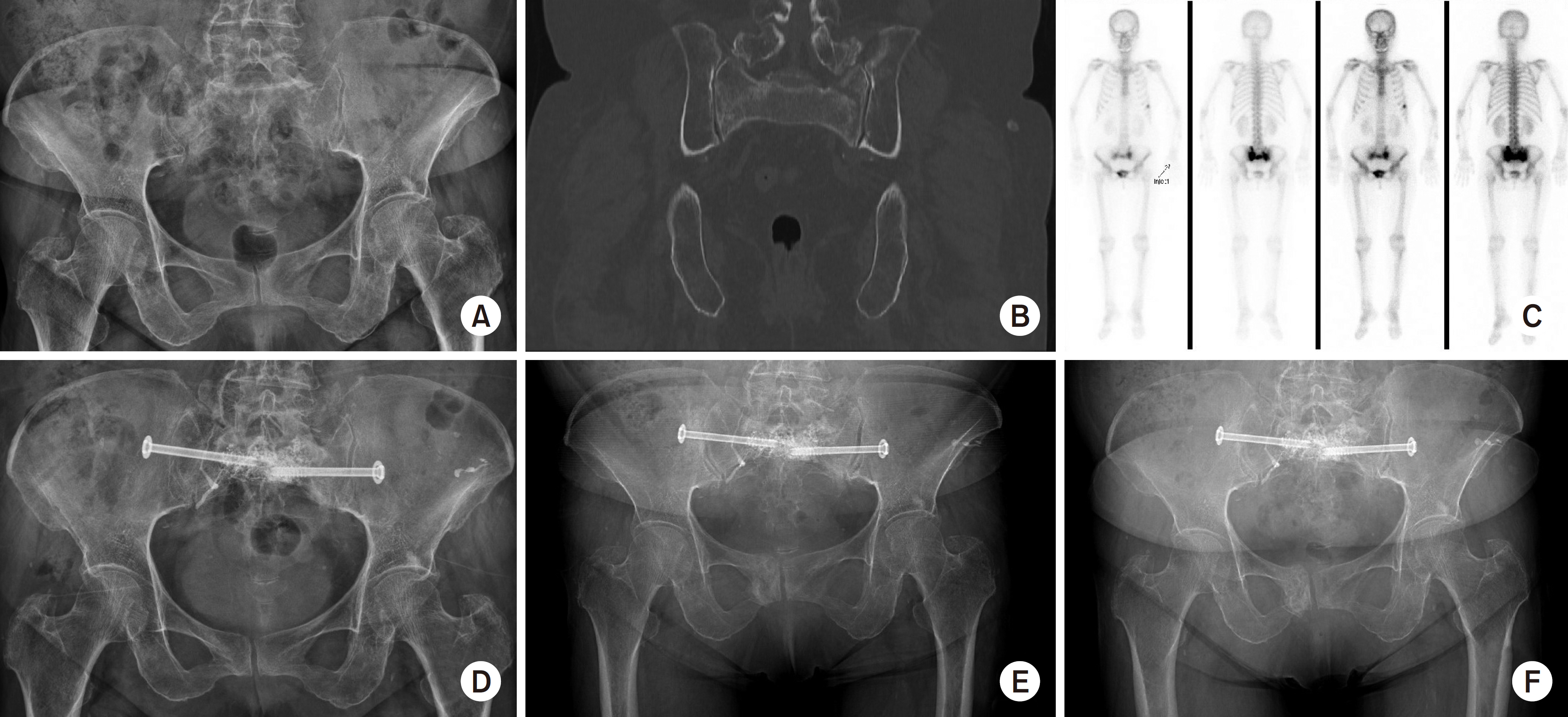
(A-C) A 70-year-old female patient was diagnosed with osteoporotic sacral fracture by simple radiography, computed tomography, and bone scan. (D) There is no cement-leakage on postoperative radiography. (E, F) Bone-union was achieved within six months of surgery. There was no screw-exchange six months and one year after surgery.
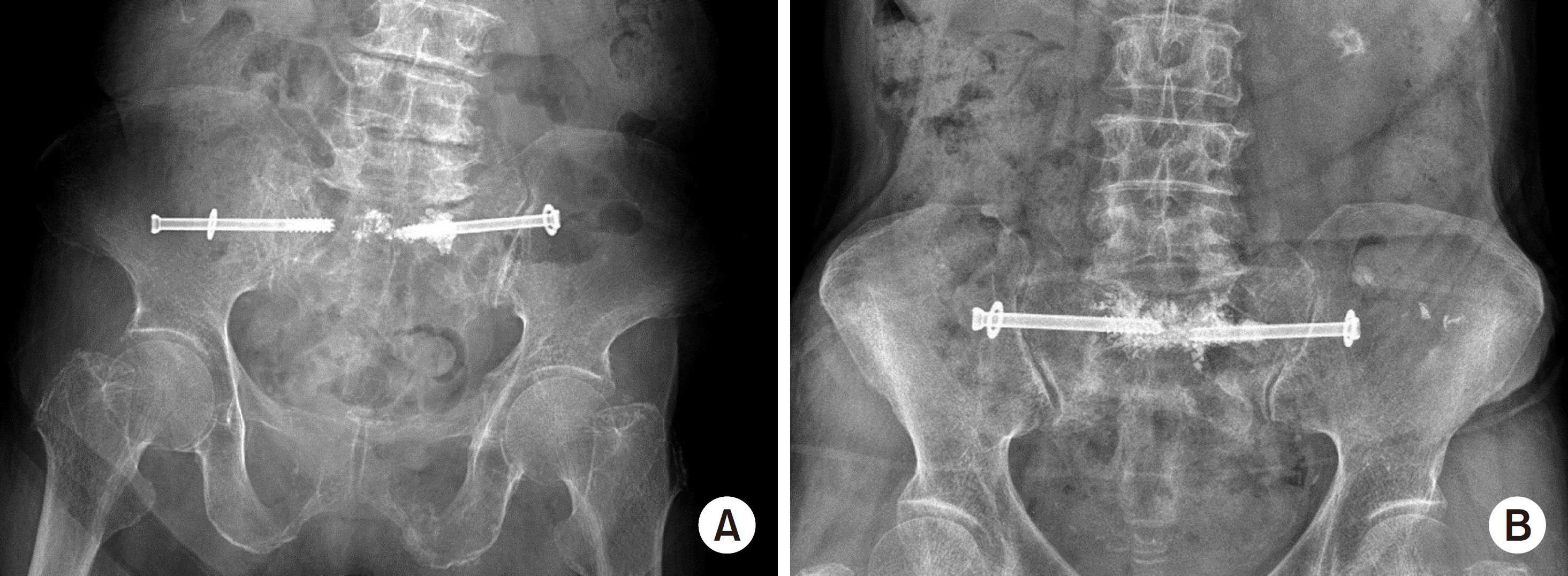
(A) Percutaneous screw fixation with cement augmentation was conducted on an 81-year-old female patient. There is a pull-out screw one month after surgery. (B) Percutaneous screw fixation with cement augmentation was conducted on a 78-year-old female patient. There is a pull-out screw after 12 days of surgery.
