References
1. Järvholm U, Körner L, Thorén O, Wiklund LM. Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand 55:652–656.
1984;
2. Su J, Cao X. Can operations achieve good outcomes in elderly patients with Sanders II-III calcaneal fractures? Medicine (Baltimore) 96:e7553. 2017;
3. Gaskill T, Schweitzer K, Nunley J. Comparison of surgical outcomes of intraarticular calcaneal fractures by age. J Bone Joint Surg Am 92:2884–2889.
2010;
4. Sanders R. Displaced intraarticular fractures of the calcaneus. J Bone Joint Surg Am 82:225–250.
2000;
5. Basile A. Operative versus nonoperative treatment of displaced intraarticular calcaneal fractures in elderly patients. J Foot Ankle Surg 49:25–32.
2010;
6. Herscovici D Jr, Widmaier J, Scaduto JM, Sanders RW, Walling A. Operative treatment of calcaneal fractures in elderly patients. J Bone Joint Surg Am 87:1260–1264.
2005;
7. Hatzokos I, Karataglis D, Papadopoulos P, Dimitriou C, Christodoulou A, Pournaras J. Treatment of intraarticular comminuted os calcis fractures. Orthopedics 29:25–29.
2006;
8. Khorbi A, Chebil M, Ben Maitigue M, et al. [Screw fixation without bone graft of calcaneal joint fractures: 35 cases]. Rev Chir Orthop Reparatrice Appar Mot 92:45–51.
2006;French.
9. McGarvey WC, Burris MW, Clanton TO, Melissinos EG. Calcaneal fractures: indirect reduction and external fixation. Foot Ankle Int 27:494–499.
2006;
10. Schepers T, Patka P. Treatment of displaced intraarticular calcaneal fractures by ligamentotaxis: current concepts' review. Arch Orthop Trauma Surg 129:1677–1683.
2009;
11. Mittlmeier T, Morlock MM, Hertlein H, et al. Analysis of morphology and gait function after intraarticular calcaneal fracture. J Orthop Trauma 7:303–310.
1993;
12. Benirschke SK, Sangeorzan BJ. Extensive intraarticular fractures of the foot. Surgical management of calcaneal fractures. Clin Orthop Relat Res 292:128–134.
1993;
13. Boack DH, Wichelhaus A, Mittlmeier T, Hoffmann R, Haas NP. [Therapy of dislocated calcaneus joint fracture with the AO calcaneus plate]. Chirurg 69:1214–1223.
1998;German.
14. Letournel E. Open treatment of acute calcaneal fractures. Clin Orthop Relat Res 290:60–67.
1993;
15. Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res 290:76–86.
1993;
16. Dhillon MS, Bali K, Prabhakar S. Controversies in calcaneus fracture management: a systematic review of the literature. Musculoskelet Surg 95:171–181.
2011;
17. Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 13:369–372.
1999;
18. Burdeaux BD. Reduction of calcaneal fractures by the McReyn-olds medial approach technique and its experimental basis. Clin Orthop Relat Res 177:87–103.
1983;
19. Mann RA. Arthrodesis of the foot and ankle. In : Coughlin MJ, Mann RA, Saltzman CL, eds. Surgery of the foot and ankle. Vol 1 8th ed.th ed. Philadelphia, Mosby: 1091–1123; 2007.
20. Kline AJ, Anderson RB, Davis WH, Jones CP, Cohen BE. Minimally invasive technique versus an extensile lateral approach for intraarticular calcaneal fractures. Foot Ankle Int 34:773–780.
2013;
21. Weber M, Lehmann O, Sägesser D, Krause F. Limited open reduction and internal fixation of displaced intraarticular fractures of the calcaneum. J Bone Joint Surg Br 90:1608–1616.
2008;
22. Hospodar P, Guzman C, Johnson P, Uhl R. Treatment of displaced calcaneus fractures using a minimally invasive sinus tarsi approach. Orthopedics 31:1112. 2008;
23. Johal HS, Buckley RE, Le IL, Leighton RK. A prospective randomized controlled trial of a bioresorbable calcium phosphate paste (alpha-BSM) in treatment of displaced intraarticular calcaneal fractures. J Trauma 67:875–882.
2009;
24. Longino D, Buckley RE. Bone graft in the operative treatment of displaced intraarticular calcaneal fractures: is it helpful? J Orthop Trauma 15:280–286.
2001;
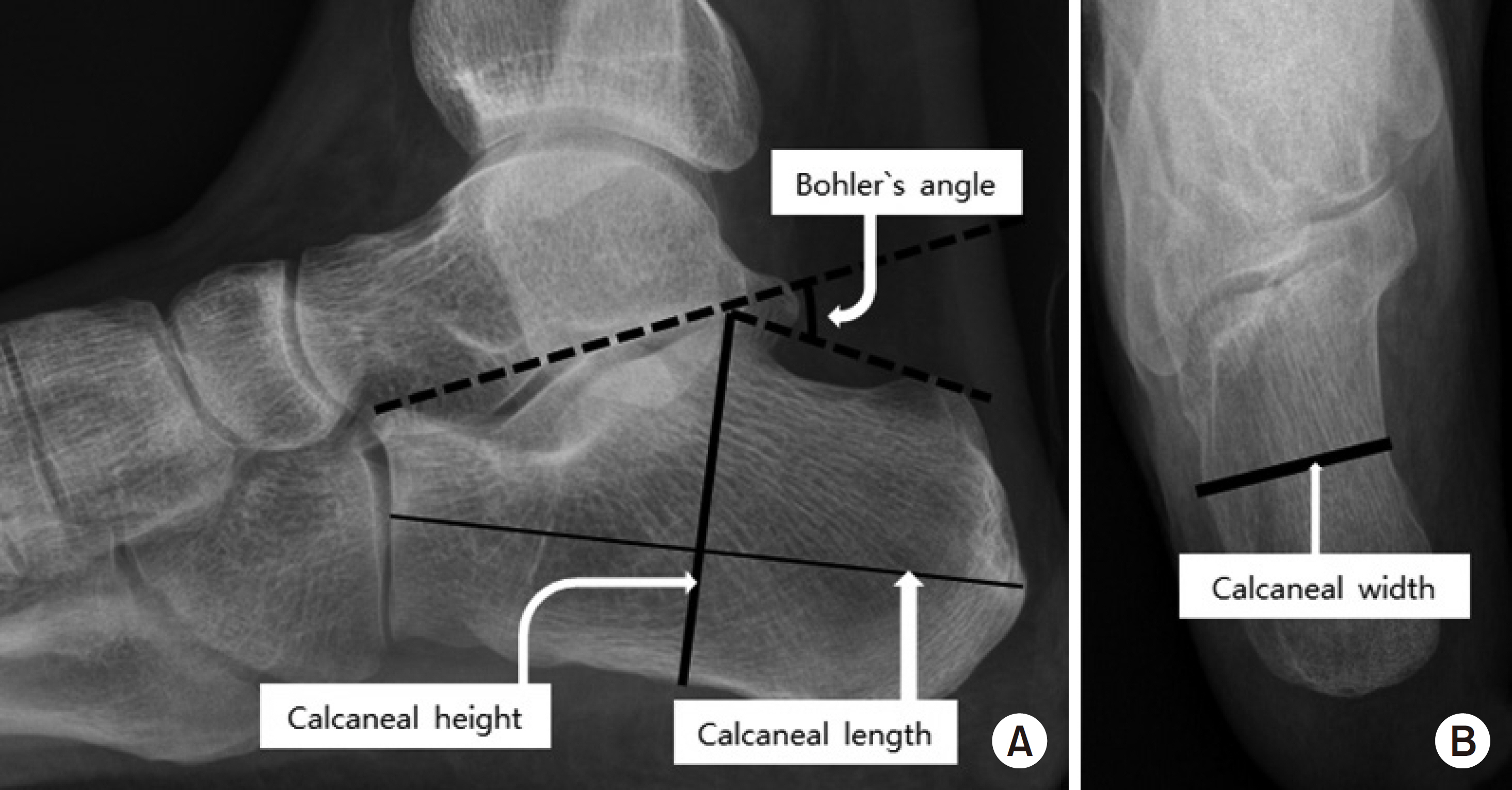
25. Su Y, Chen W, Zhang T, Wu X, Wu Z, Zhang Y. Bohler's angle's role in assessing the injury severity and functional outcome of internal fixation for displaced intraarticular calcaneal fractures: a retrospective study. BMC Surg 13:40. 2013;
26. Gonzalez TA, Lucas RC, Miller TJ, Gitajn IL, Zurakowski D, Kwon JY. Posterior facet settling and changes in Bohler's angle in operatively and nonoperatively treated calcaneus fractures. Foot Ankle Int 36:1297–1309.
2015;
27. Backes M, Dorr MC, Luitse JS, Goslings JC, Schepers T. Predicting loss of height in surgically treated displaced intraarticular fractures of the calcaneus. Int Orthop 40:513–518.
2016;
28. Stulik J, Stehlik J, Rysavy M, Wozniak A. Minimally-invasive treatment of intraarticular fractures of the calcaneum. J Bone Joint Surg Br 88:1634–1641.
2006;
29. Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res 290:87–95.
1993;
30. Ceccarelli F, Calderazzi F, Pedrazzi G. Is there a relation between AOFAS ankle-hindfoot score and SF-36 in evaluation of Achilles ruptures treated by percutaneous technique? J Foot Ankle Surg 53:16–21.
2014;