Results after Less Invasive Locking Plating in Intra-Articular Fractures of the Distal Femur
Article information
Abstract
Abstract
Purpose
The purpose of this study was to determine the clinical outcomes after a less invasive locking plating technique in intra-articular fractures of the distal femur.
Materials and Methods
This was a retrospective 19 case series of patients with distal femoral intra-articular fractures treated with a less invasive locking plating technique in a single center (Dankook University Hospital) from June 2010 to April 2016. Nineteen patients (11 males and 8 females) with a mean age of 55.9 years were enrolled. The functional outcomes were evaluated using the visual analogue scale (VAS), range of knee joint motion (flexion & extension), and Knee Society score. The radiology outcomes were evaluated with parameters measured in a plain radiograph (deviation angle of alignment axis on coronal and sagittal plane, mechanical lateral distal femur angle).
Results
The mean follow-up period was 26.4 months (range, 12–72 months) and the mean duration to union was 15.94 weeks (range, 11–28 weeks). The mean VAS was 1.36 (range, 0–8) and the range of motion of the knee joint was extension 4.73° (range, 0°-30°) and flexion 107.36° (range, 60°-135°). The mean Knee Society score was 85.47 (range, 47–100). The mean deviation angle of the coronal alignment axis was 4.07° (range, 1.3°-8.8°), the mean deviation angle of the sagittal alignment axis was 3.23° (range, 0.7°-7.0°), and the mechanical lateral femoral angle was 87.75° (range, 82.8°-95.5°). Six patients had traumatic osteoarthritis at the final follow-up.
Conclusion
The purpose of this study was to evaluate the clinical and radiologic outcomes of intraar-ticular fractures of the distal femur in patients who underwent an anatomical reduction through an open reduction, and converted to an extra-articular fracture with rigid internal fixation. The results were relatively satisfactory.
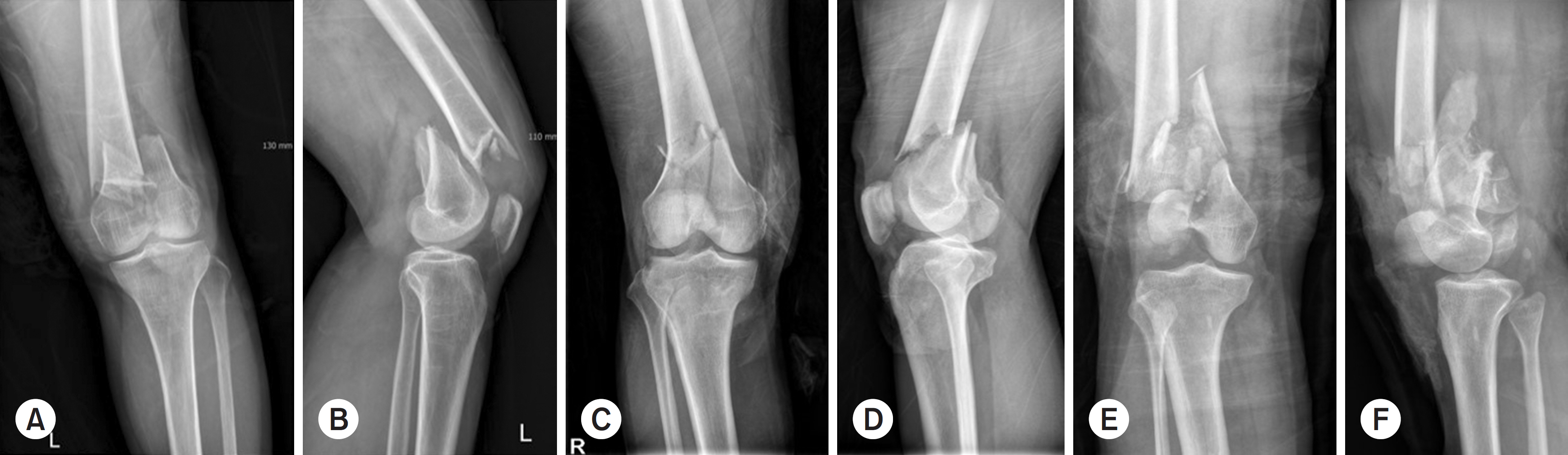
Simple radiographs show anterior-posterior and lateral view of distal femur fractures: AO/OTA classification. (A, B) type C1 fracture, (C, D) type C2 fracture, (E, F) type C3 fracture.

Intraoperative photograph showing the lateral parapatella approach for articular exposure and reconstruction.

Following reduction, an appropriate-sized plate was slid in a distal-to-proximal direction over the periosteum at the lateral aspect of the distal femur.

Intraoperative radiograph (using C-arm) for check the alignment of the distal femur and positioning of the plate.

Radiological changes in osteoarthritis at the final follow-up after the minimally invasive plate osteosynthesis technique for a distal femur complete intra-articular fracture.


