Clinical Outcomes of Minimally Invasive Surgery in Sanders Type IV Intra-Articular Calcaneal Fractures
Article information
Abstract
Abstract
Purpose
This study evaluated the radiologic and clinical results in patients who underwent minimal invasive surgery using sinus tarsi approach in Sanders type IV calcaneal fracture.
Materials and Methods
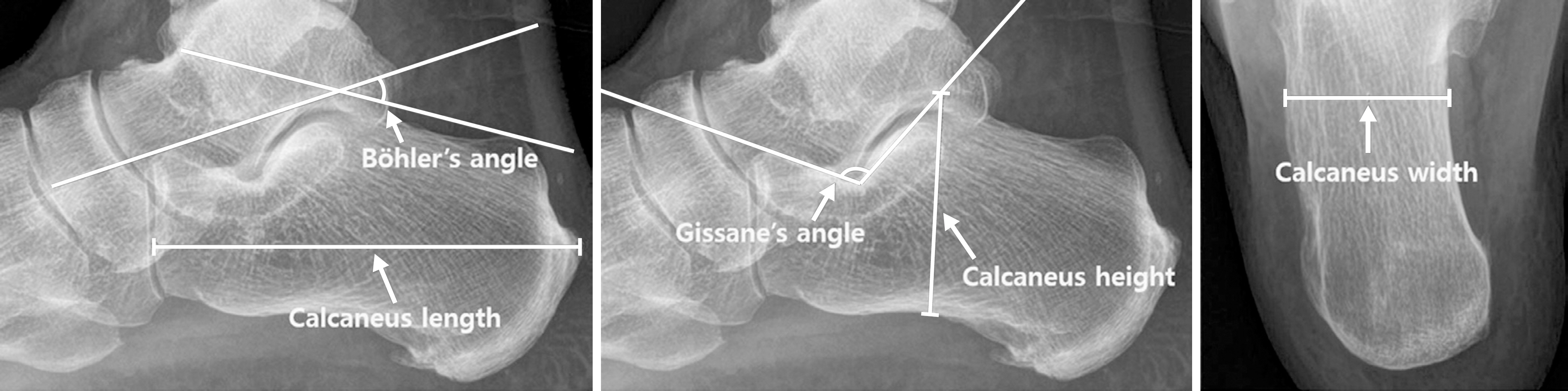
This retrospective study evaluated 13 cases of Sanders type IV calcaneus fractures that were treated by minimal invasive surgery using the sinus tarsi approach from July 2012 to April 2017. Further, these cases could be followed up for more than 12 months. Bone union, radiologic parameters such as Böhler's angle, Gissane's angle, calcaneal height, length, and width, the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, and the postoperative complications were evaluated.
Results
Bony union was achieved in all the cases at the final follow up, and the mean union time was 5.5 months. One patient underwent reoperation for a surgical site infection, six patients had post traumatic arthritis, and two of them underwent subtalar joint fusion. The mean AOFAS ankle-hindfoot score was 81.2. At the final follow-up, the mean values of Böhler's angle and Gissane's angle were 20° and 119.8°, respectively, and the mean values of the calcaneus height, length, and width were 46.8 mm, 81.8 mm, and 45.6 mm, respectively.
Conclusion
Minimal invasive surgery using the sinus tarsi approach for Sanders type IV calcaneal fracture resulted in satisfactory anatomic reduction and stable fixation, and satisfactory clinical and radiologic results were obtained in most of the patients. Minimal invasive surgery is thought to reduce the soft tissue-related complications as compared to surgery using the extensile lateral approach.

(A) Preoperative X-ray and computed tomography showing a Sanders type IV and joint depressive type calcaneal fracture. (B) The postoperative X-ray showing restoration of the of Böhler's angle, Gissane's angle, and the calcaneus height, length, and width.

Intraoperative fluoroscope images showing posterior facet reduction using Schantz pin and fixation with 6.5 mm cannulated screws and K-wire.