Failure of Intramedullary Nailing for Subtrochanteric Atypical Femoral Fractures Caused by Endosteal Cortical Thickening
Article information
Abstract
Abstract
Purpose
Recent literature has noted incidences of subtrochanteric atypical femoral fractures (AFFs) in patients who have taken long-term bisphosphonates (BPs). Most cases of subtrochanteric AFFs have been treated with intramedullary nailing and cases of delayed union have been reported. On the other hand, there is no data available on the complications associated with endosteal thickening or cortical thickening. This study evaluated the results of surgical treatment according to the endosteal thickening of the lateral cortex in subtrochanteric AFFs.
Materials and Methods
Investigation was performed at the Department of Orthopaedic Surgery, Jeju National University Hospital. The study consisted of patients with subtrochanteric AFFs, defined by the American Society for Bone and Mineral Research (ASBMR) major criteria, who underwent intramedullary nailing from March 2012 to October 2014. The cases were categorized into two groups based on the presence of endosteal thickening. The evaluation included the demographic data, radiographic data of initial reduction state, and duration of BPs.
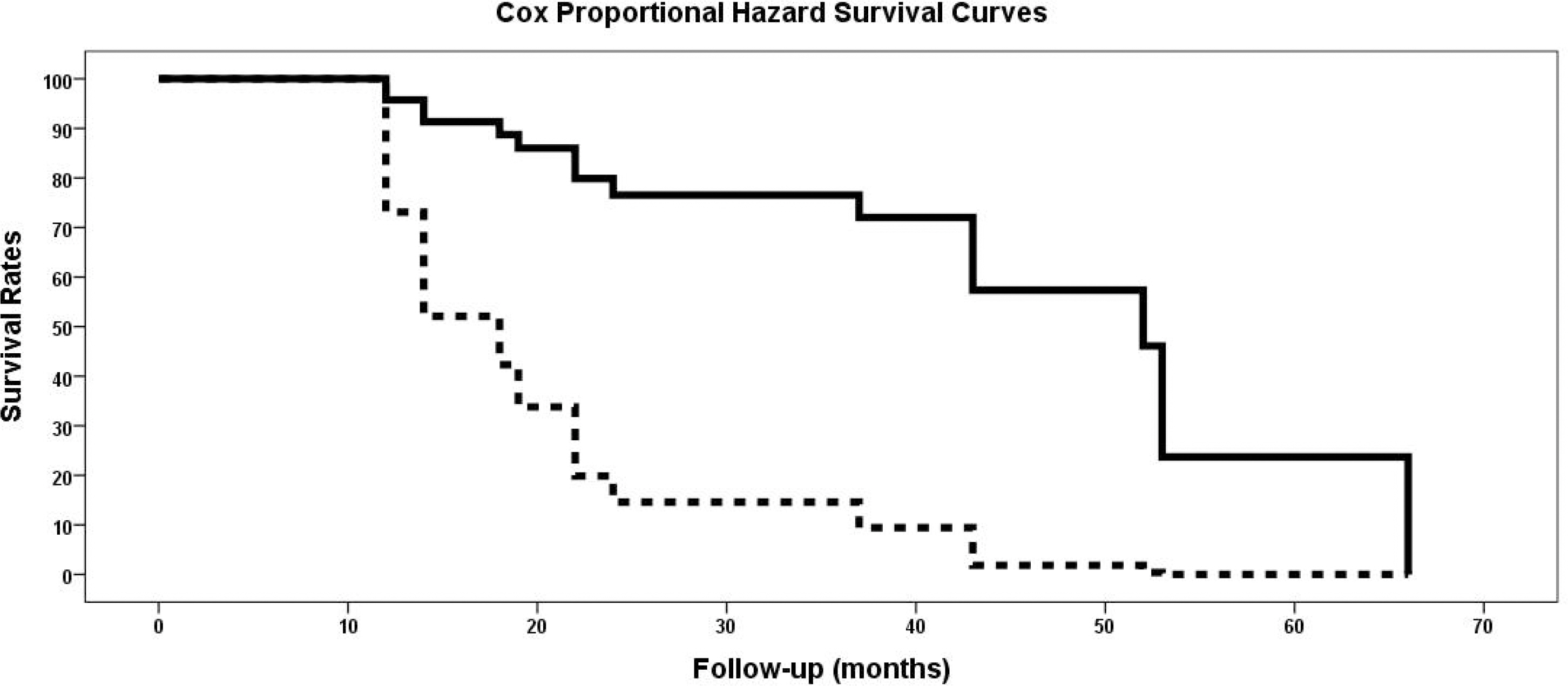
Results
The demographic data and duration of BPs were similar in the two groups. On the other hand, varus reduction (Group I: 12.5% vs. Group II: 78.9%; p=0.001), delayed union (Group I: 0% vs. Group II: 70.0%; p=0.003), nonunion (Group I: 0% vs. Group II: 47.4%; p=0.017), and union time (Group I: 5.5 months vs. Group II: 8.3 months; p<0.001) were significantly different in the two groups.
Conclusion
Endosteal thickening of the lateral cortex in subtrochanteric AFFs was identified as an independent factor that decides the reduction of the fracture and nonunion. The endosteal thickening should be removed to obtain anatomical alignment for successful surgical results.

(A) Atypical subtrochanteric fracture in the right femur, antero-posterior (AP) view. Endosteal thickening of the lateral cortex at the fracture site is depicted by a white arrow. (B) Atypical subtrochanteric fracture in the left femur, AP view. Endosteal thickening of the lateral cortex at the fracture site is depicted by a white arrow. (C) Atypical subtrochanteric fracture in the right femur, AP view. The lateral cortex thickness at the fracture site does not differ from the distal part (white arrowhead). (D) Atypical subtrochanteric fracture in the left femur AP view. Periosteal thickening of the lateral cortex is observed, but endosteal cortical thickening is not observed (white arrowhead).
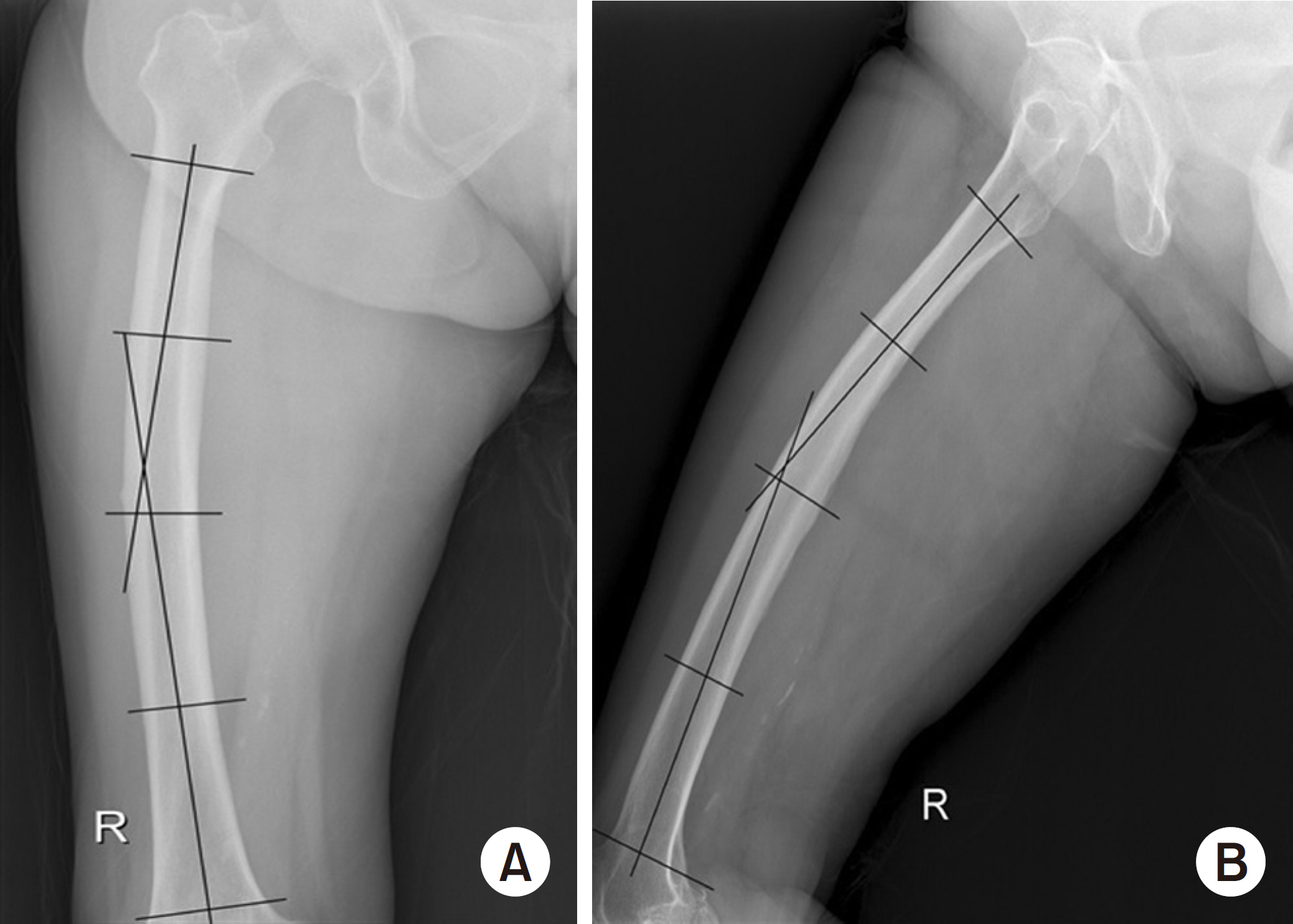
(A) Coronal plane femoral bowing was measured as the angulation between the proximal and distal quarters of the femoral diaphysis in the femur antero-posterior view. (B) Sagittal plane femoral bowing was measured as the angulation between the proximal and distal quarters of the femoral diaphysis in the femur lateral view.

(A, B) Atypical subtrochanteric fracture in the left femur, anteroposterior (AP) and lateral (LAT) views. Shortening, varus deformation, and total displacement of fracture were observed. Endosteal thickening of the lateral cortex at the fracture site is depicted by a white arrowhead. (C, D) These are left femur AP and LAT views taken nine months after surgery. The atypical subtrochanteric fracture was fixed with a long cephalo-medullary nail and cerclage cable. Callus formation was observed at four cortical regions (medial, lateral, anterior and posterior cortex) in the fracture site marked with white arrows.
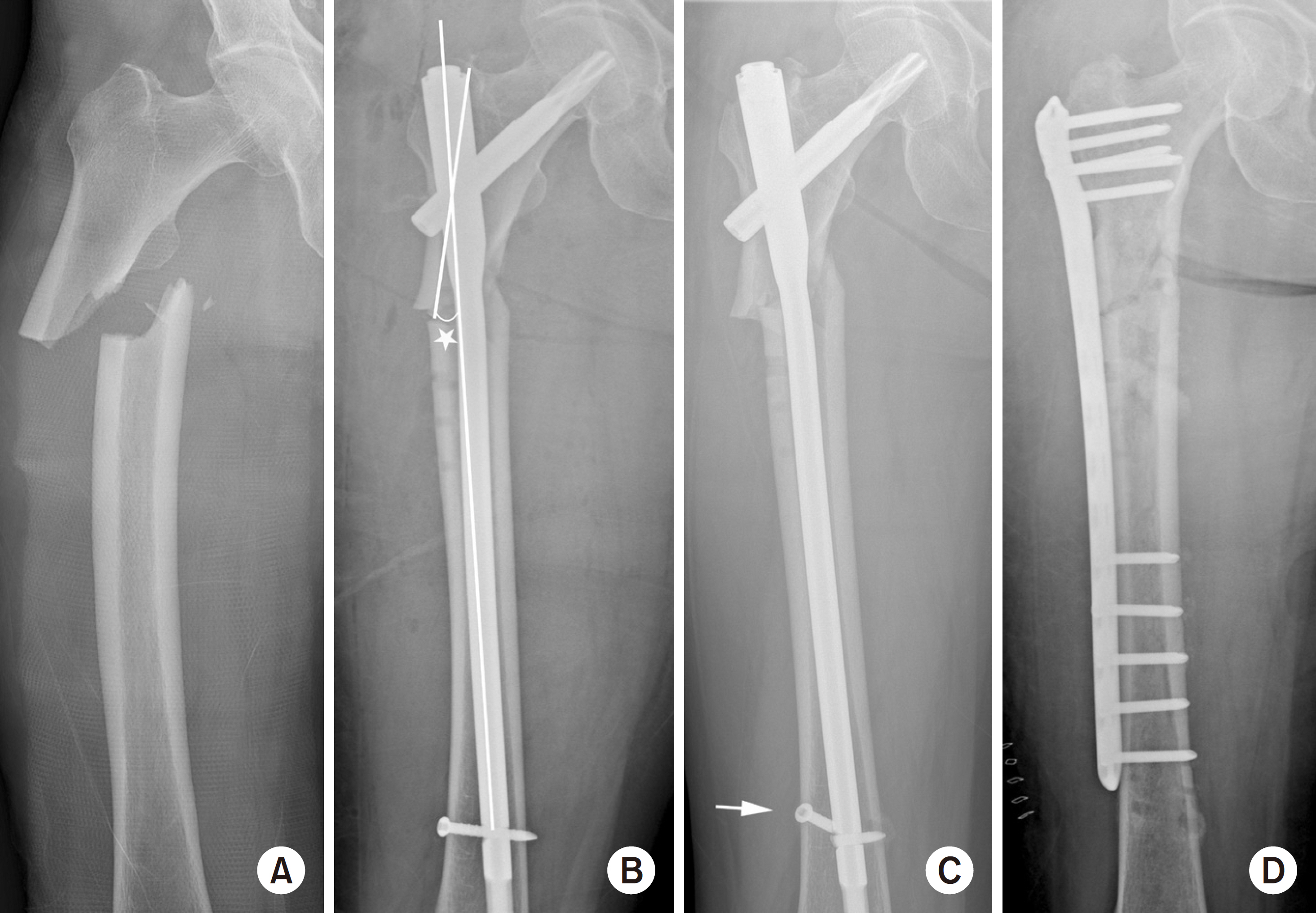
(A) Atypical subtrochanteric fracture in the right femur, antero-posterior (AP) view. (B) This is right femur AP view taken immediately after surgery. The atypical subtrochanteric fracture was fixed with a long cephalo-medullary nail. Compared to the contralateral side, 13 varus reduction was observed (asterisk). (C) This is the right femur AP view taken 12 months after surgery. Breakage of the distal interlocking screw (white arrow) and nonunion of the fracture are observed. (D) This is the right femur AP view after performing re-operation using a plate.

Thickening of the lateral cortex in subtrochanteric regions is observed on both sides. On the right side, both endosteal and periosteal cortical thickening are observed (white arrows), whereas only periosteal cortical thickening is observed on the left side (white arrowhead).