Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Article information
Abstract
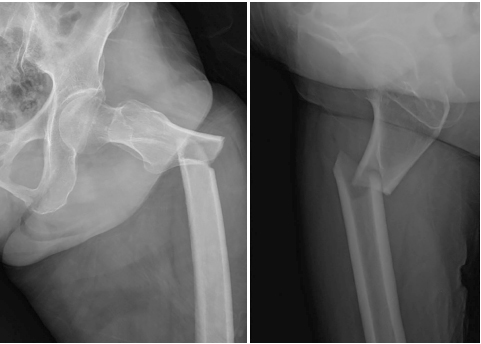
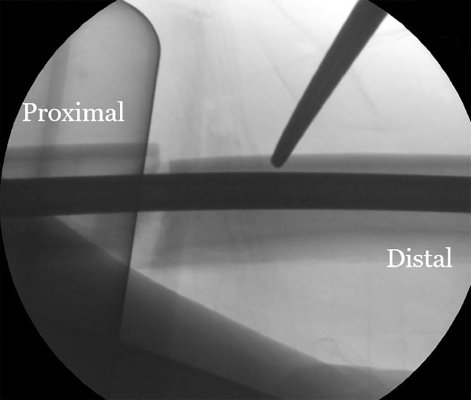
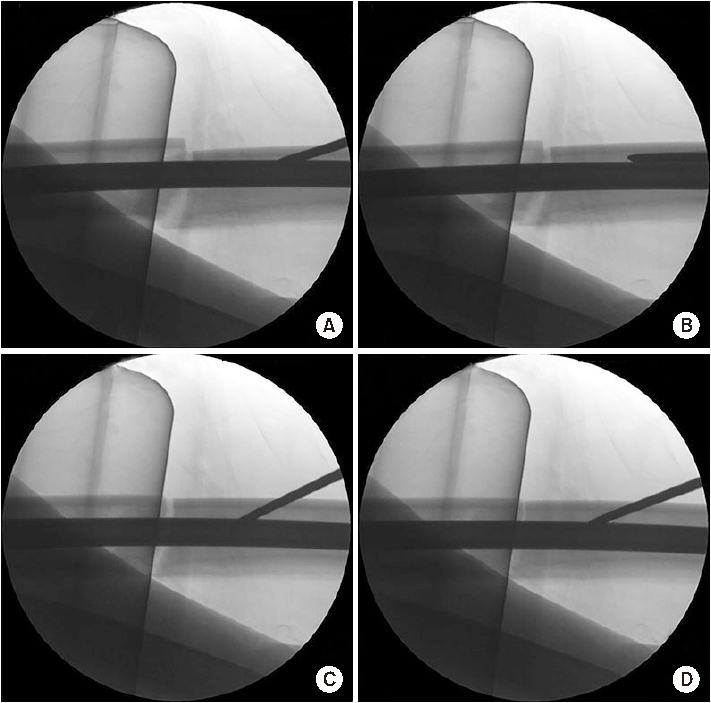
The subtrochanteric area is the place where mechanical stress is most concentrated in the femur. When a fracture happens, bone union is delayed and nonunion often occurs. The recommended treatment for atypical fractures is an anatomical reduction of the fracture site as the frequency of nonunion is higher than that of ordinary fractures. Various reduction methods have been suggested, and good results have been obtained. On the other hand, the occurrence of posterior displacement of the distal fragment during the insertion of an intramedullary nail is often overlooked. This is probably because the bone marrow of the femur tends to form an elliptical shape in the anteroposterior direction. The author attempted to insert a blocking screw into the distal part of the fracture to prevent posterior displacement of the distal fragment while performing intramedullary nailing of the femur fracture and achieved a good reduction state easily.
Notes
None.
None.